- Department of Surgery, Division of Neurosurgery, University of Arizona College of Medicine – Phoenix, Maricopa Medical Center, Phoenix, Arizona, USA
- Department of Radiology, University of Arizona College of Medicine – Phoenix, Maricopa Medical Center, Phoenix, Arizona, USA
Correspondence Address:
Tina W. Wong
Department of Surgery, Division of Neurosurgery, University of Arizona College of Medicine – Phoenix, Maricopa Medical Center, Phoenix, Arizona, USA
DOI:10.4103/sni.sni_115_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Tina W. Wong, Daniel G. Gridley, Iman Feiz-Erfan. Epidural venous plexus engorgement due to inferior vena cava thrombosis resulting in cauda equina syndrome: Case report and literature review. 04-Jul-2018;9:129
How to cite this URL: Tina W. Wong, Daniel G. Gridley, Iman Feiz-Erfan. Epidural venous plexus engorgement due to inferior vena cava thrombosis resulting in cauda equina syndrome: Case report and literature review. 04-Jul-2018;9:129. Available from: http://surgicalneurologyint.com/?post_type=surgicalint_articles&p=8915
Abstract
Background:Epidural venous plexus congestion at L5-S1 due to inferior vena cava (IVC) thrombosis led to an acute cauda equina syndrome (CES). Laminectomy to rule out an epidural abscess, allowing for resection of the dilated veins, led to immediate symptom resolution.
Case Description:A 47-year-old male presented with acute urinary retention and left greater than right lower extremity paresis of 2 weeks duration. Magnetic resonance imaging (MRI) revealed a contrast-enhancing space-occupying anterior epidural L5-S1 level lesion resulting in cauda equina compression. As the patient was septic, he underwent an emergency laminectomy for a presumed epidural abscess. Intraoperative findings, however, documented a markedly dilated epidural venous plexus secondary to a newly diagnosed IVC thrombus. One day postoperatively, the patient was symptom-free and neurologically intact.
Conclusions:Here we report a patient who uniquely presented with a CES characterized by acute paraparesis. This was attributed to a massively engorged anterior lumbar epidural venous plexus attributed to newly diagnosed IVC thrombus.
Keywords: Cauda equina syndrome, epidural venous plexus engorgement, inferior vena cava thrombosis
INTRODUCTION
Well-established causes of cauda equina syndrome (CES) include spinal tumors, infection/inflammation, critical stenosis, arteriovenous malformations, and hemorrhages.[
CASE REPORT
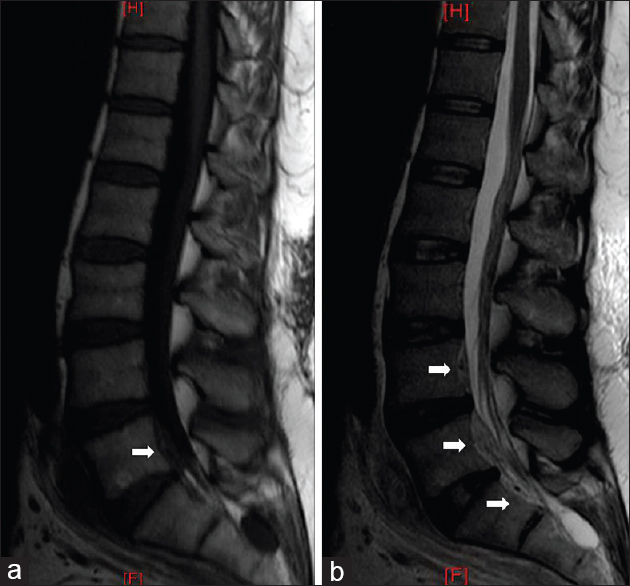
A 47-year-old male presented with 2 weeks of a progressive left lower extremity paraparesis and 5 days of urinary dysfunction. On admission, he demonstrated a leukocytosis of 21.6 × 103 cells/μL, along with Streptococcus viridans septicemia. Also noted was acute venous thrombosis extending from the left popliteal vein to the IVC (e.g., at the confluence of left and right common iliac vein) [
Figure 1
A venacavagram performed during IVC filter placement demonstrating filling defect near the confluence of the common iliac veins (a) with delayed reconstitution of contrast flow into the right, but not left, common iliac vein (b). Findings are consistent with an occlusive thrombus in the left common iliac vein with extension into the proximal IVC which is near-occlusive in nature
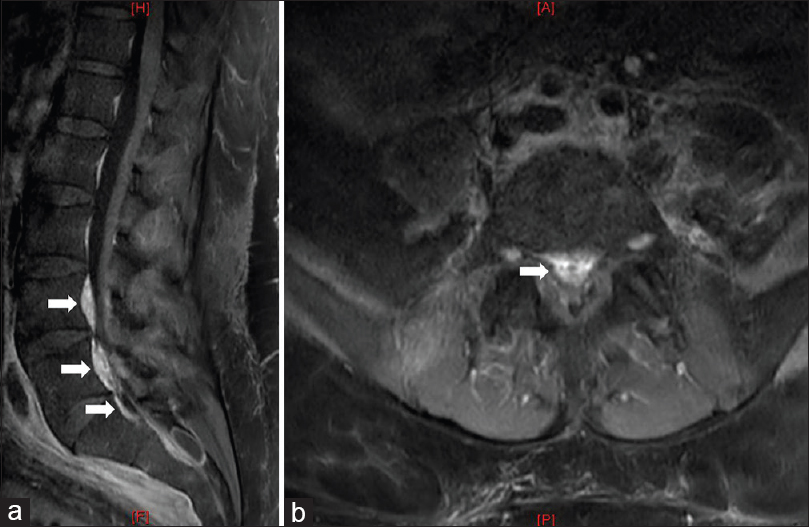
Figure 2
(a) Sagittal T1-weighted MR sequence revealing a lesion in the L5-S1 anterior epidural space that is heterogeneously hypointense (arrow). (b) Sagittal T2-weighted MR sequence with anterior spinal epidural lesion that is mixed iso- and hyperintense centrally with a rim of hypointensity peripherally (arrows), most prominently seen at L4-S1 but also present at T12-L3 levels. There is evidence of mass effect with compression of the thecal sac
DISCUSSION
EVPE engorgement causing low back pain, radiculopathy, and CES is rare, and the diagnosis is often missed. It was first described in the 1940s by Cohen[
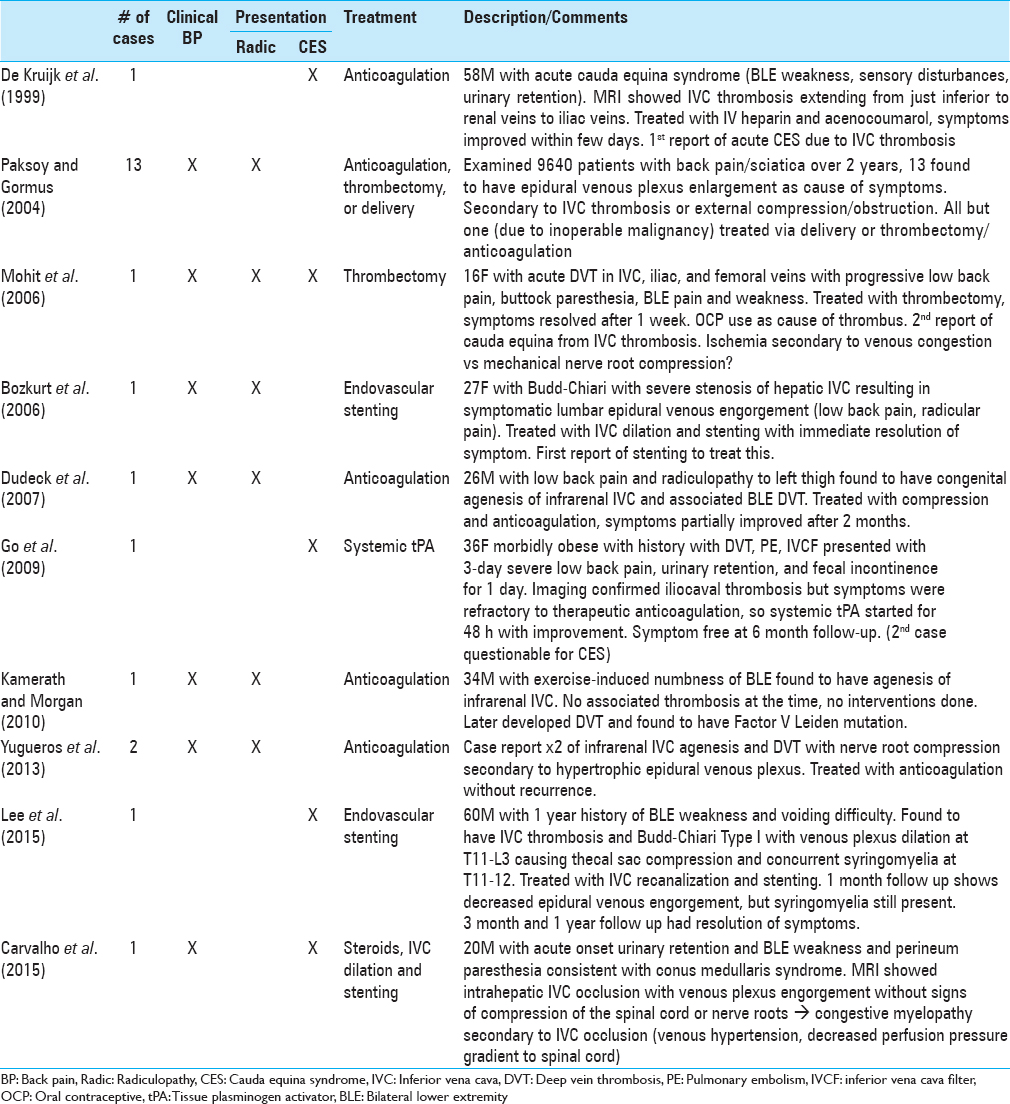
There are only 20 previously reported cases of myelopathy associated with EVPE secondary to IVC thrombosis, only five of which exhibited symptoms of CES [
CONCLUSION
Symptomatic massive engorgement of the L5-S1 anterior EVPE resulted in a CES due to iliocaval thrombosis. Following a laminectomy to rule out an epidural abscess, coagulation/resection of the dilated venous plexus resulted in full symptom resolving.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bozkurt G, Cil B, Akbay A, Turk CC, Palaoglu S. Intractable radicular and low back pain secondary inferior vena cava stenosis associated with Budd-Chiari syndrome: Endovascular treatment with cava stenting: Case report and review of the literature. Spine (Phila Pa 1976). 2006. 31: E383-6
2. Carvalho DZ, Hughes JD, Liebo GB, Bendel EC, Bjarnason H, Klaas JP. Venous Congestive Myelopathy due to Chronic Inferior Vena Cava Thrombosis Treated with Endovascular Stenting: Case Report and Review of the Literature. J Vasc Interv Neurol. 2015. 8: 49-53
3. Cohen I. Extradural varix simulating herniated nucleus proposes. J Mt Sinai Hosp. 1941. 8: 136-8
4. De Kruijk J, Korten A, Boiten J, Wilmink J. Acute cauda equina syndrome caused by thrombosis of the inferior vena cava. J Neurol Neurosurg Psychiatry. 1999. 67: 827-8
5. Dudeck O, Zeile M, Poellinger A, Kluhs L, Ludwig WD, Hamm B. Epidural venous enlargements presenting with intractable lower back pain and sciatica in a patient with absence of the infrarenal inferior vena cava and bilateral deep venous thrombosis. Spine (Phila Pa 1976). 2007. 32: E688-91
6. Epstein BS. Low back pain associated with varices of the epidural vein simulating herniation of the nucleus proposes. Am J Res. 1947. 57: 736-40
7. Go MR, Baril DT, Leers SA, Chaer RA. Acute cauda equina syndrome secondary to iliocaval thrombosis successfully treated with thrombolysis and pharmacomechanical thrombectomy. J Endovasc Ther. 2009. 16: 233-7
8. Kamerath J, Morgan WE. Absent inferior vena cava resulting in exercise-induced epidural venous plexus congestion and lower extremity numbness: A case report and review of the literature. Spine (Phila Pa 1976). 2010. 35: E921-4
9. Lee JH, Song WJ, Kang KC. Myelopathy-mimicking symptoms of epidural venous engorgement and syringomyelia due to inferior vena cava stenosis at the thoracolumbar junction in a patient with Budd-Chiari syndrome. J Neurosurg Spine. 2015. 23: 467-70
10. Mohit AA, Fisher DJ, Matthews DC, Hoffer E, Avellino AM. Inferior vena cava thrombosis causing acute cauda equina syndrome. Case report. J Neurosurg. 2006. 104: 46-9
11. Mukherjee S, Thakur B, Crocker M. Cauda equina syndrome: A clinical review for the frontline clinician. Br J Hosp Med (Lond). 2013. 74: 460-4
12. Paksoy Y, Gormus N. Epidural venous plexus enlargements presenting with radiculopathy and back pain in patients with inferior vena cava obstruction or occlusion. Spine (Phila Pa 1976). 2004. 29: 2419-24
13. Yugueros X, Alvarez B, Fernandez E, Boque M, Matas M. Compressive symptoms due to thrombosed or hypertrophic collateral circulation in infrarenal inferior vena cava agenesis. Ann Vasc Surg. 2013. 27: 238 e239-238 e213