- Grant Medical Center, Ohio Health, Columbus, USA
- Department of Neurosurgery, Genesis Healthcare System, Zanesville, Ohio, USA
Correspondence Address:
Jason Milton
Grant Medical Center, Ohio Health, Columbus, USA
Department of Neurosurgery, Genesis Healthcare System, Zanesville, Ohio, USA
DOI:10.4103/sni.sni_60_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jason Milton, Julie Renner, Victor Awuor. B-cell lymphoma presenting as multiple nerve sheath tumors. 11-Jul-2017;8:142
How to cite this URL: Jason Milton, Julie Renner, Victor Awuor. B-cell lymphoma presenting as multiple nerve sheath tumors. 11-Jul-2017;8:142. Available from: http://surgicalneurologyint.com/surgicalint-articles/b%e2%80%91cell-lymphoma-presenting-as-multiple-nerve-sheath-tumors/
Abstract
Background:Diffuse Large B-cell Lymphoma (DLBCL) is the most common form of Non-Hodgkin lymphoma (NHL), accounting for 25-30 percent of cases in the United States.1 Extranodal sites are involved in approximately 40% of cases of DLBCL.
Case Description:In this report, we discuss the case of a patient with extranodal DLBCL within the cervical nerve roots that underwent surgical intervention due to the presence of cervical radiculopathy.
Conclusion:The diagnosis of DLBCL was surprising given the appearance of the masses on MRI being similar to that of a neurofibroma or schwannoma. Surgical decompression provided a tissue sample for biopsy as well as an opportunity for decompression of the nerve roots and restoration of function of the patient's left upper extremity.
Keywords: B-cell, lymphoma, spine, tumor
INTRODUCTION
Diffuse large B-cell lymphoma (DLBCL) accounts for 25–30% cases of non-Hodgkin lymphoma (NHL) in the United States.[
CASE DESCRIPTION
For 7 months, a 63-year-old female complained of left-sided neck pain and left upper extremity radiculopathy accompanied by progressive numbness and weakness. She exhibited 4/5 strength proximally and distally in the left arm alone.
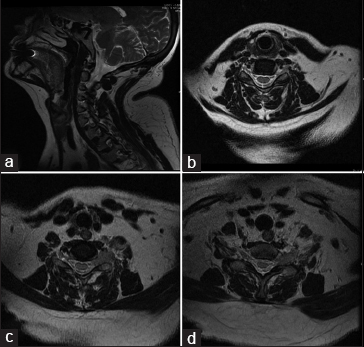
Electromyography (EMG) of the bilateral upper extremities demonstrated a left C6 and C7 radiculopathy. Magnetic resonance image (MRI) of the cervical spine revealed enhancing masses involving the left neural foramina at the C5-6, C6-7, and C7-T1 levels accompanied by nodular thickening of the left exiting nerve root at T1-2 level (T1 root) as revealed in
Surgery and postoperative status
The patient underwent a C6-7-T1 hemilaminectomy and facetectomy with subtotal resection of the C7 and T1 intradural nerve root tumors; this was accompanied by an instrumented fusion from C4-T7 with intraoperative neuromonitoring. The frozen section was equivocal. Postoperatively, the patient noted residual proximal left upper extremity hyperesthesias, with proximal LUE strength of 4/5 but distal increased weakness to the 3/5 level. Motor function in the right upper extremity (RUE) was 4/5 and both lower extremities were neurologically intact.
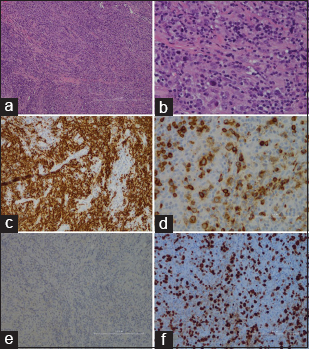
The pathology confirmed B-cell lymphoma as shown in
Figure 2
Histology. (a and b) H and E permanent sections reveal pleomorphic population of mononuclear cells including small and large forms at ×10 and ×40 magnification respectively, (c) CD20 immuno-histochemical staining reveals strong CD20 immunoreactivity, (d) CD79a immunohistochemical staining reveals strong CD79a immunoreactivity, (e) tissue biopsies are without GFAP immunoreac-tivity, (f) MIB-1 highlights increased mitotic activity
Chemotherapy and postoperative follow-up
The patient underwent chemotherapy consisting of 6 cycles of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP). In addition, she received two doses of systemic methotrexate and two doses of intrathecal methotrexate. Prior to beginning pharmacologic therapy, a postoperative MRI was obtained, which was of poor quality due to the presence of hardware. Six months after her diagnosis, repeat positron emission tomography–computed tomography was performed without evidence of residual mass or abnormal metabolic activity. Her neurological examination remained unchanged. She will undergo oncologic surveillance at 12 months and then will undergo follow-up yearly thereafter. At 6 months, the patient was considered to be in remission.
CONCLUSION
Nerve root infiltration has been reported in both T-cell and B-cell NHL, however, nervous system involvement does not usually occur in the absence of widespread disease.[
In our patient, a left-sided C6 and C7 radiculopathy correlated with MR-confirmed multifocal left-sided foraminal lesions. The decompressive laminectomy with instrumented fusion yielded B-cell lymphoma followed by appropriate chemotherapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Baehring JM, Batchelor TT. Diagnosis and Management of Neurolymphomatosis. Cancer J. 2012. 18: 463-8
2. Boyiadzis M, Foon KA, Lichtman MA, Kipps TJ, Seligsohn U.editors. Diffuse Large B-call Lymphoma. Williams Hematology. China: McGraw-Hill Companies, Inc; 2010. p.
3. Cappellari M, Benedetti F, Fiaschi A, Benedetti MD. Multiple radiculopathy as the presenting manifestation of primary spinal leptomeningeal B cell lymphoma detected by flow cytometry of cerebrospinal fluid. Neurol Sci. 2011. 32: 1171-4
4. Hughes RA, Britton T, Richards M. Effects of Lymphoma on the Peripheral Nervous System. J R Soc Med. 1994. 87: 526-30
5. Kapoor R, Revesz T, Powell M. Solitary cervical lymphoma presenting as a neurofibroma. Br J Neurosurg. 1992. 6: 583-6
6. Kelly JJ, Karcher DS. Lymphoma and Peripheral Neuropathy: A clinical review. Muscle Nerve. 2005. 31: 301-13
7. Shibata-Hamaguchi A, Samuraki M, Furui E, Ishida C, Kitagawa S, Nakao S. B-cell neurolymphomatosis confined to the peripheral nervous system. J Neurol Sci. 2007. 260: 249-52






John Lewis
Posted July 24, 2017, 12:17 am
This article sheds light on a truly unheard of diagnosis. I appreciate the thorough report on this case and have cited the article in a number of graduate reports. Thank you to Dr. Awuor for again delivering a well written scholarly article.