- Neurosurgical Spine/Education, Department of NeuroScience, NYU Winthrop Hospital, Mineola, New York, USA
Correspondence Address:
Nancy E. Epstein
Neurosurgical Spine/Education, Department of NeuroScience, NYU Winthrop Hospital, Mineola, New York, USA
DOI:10.4103/sni.sni_182_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein, Renee D. Hollingsworth. Nursing review section of surgical neurology international: Evaluation of cervical disc disease and when surgery is warranted. 07-Jul-2017;8:136
How to cite this URL: Nancy E. Epstein, Renee D. Hollingsworth. Nursing review section of surgical neurology international: Evaluation of cervical disc disease and when surgery is warranted. 07-Jul-2017;8:136. Available from: http://surgicalneurologyint.com/surgicalint-articles/nursing-review-section-of-surgical-neurology-international-evaluation-of-cervical-disc-disease-and-when-surgery-is-warranted/
Abstract
Background:Patients with cervical disc disease may present with radiculopathy (root compression), myelopathy (cord compression), or myeloradiculopathy. These complaints must be correlated with x-ray, magnetic resonance (MR) imaging, and computed tomographic (CT) scans. Although most patients can be managed nonsurgically, those with significant neurological deficits and larger disc herniations may require surgery.
Methods:The symptoms of cervical radiculopathy include pain radiating down one or both arms, while myelopathy may result in more diffuse numbness tingling or weakness in the upper and/or lower extremities. The neurological signs for cervical discs include; focal or diffuse loss of motor strength changes in reflexes (hyporeflexic, normal reflexes, or hyperreflexia), a loss of sensation (e.g., to pin, vibration, touch, and position), and cerebellar dysfunction (e.g., loss of coordination). Patients’ symptoms and signs must correlate with focal nerve root and/or spinal cord compression seen on MR and/or CT studies.
Results:MR examinations best document soft disc herniations, while CT scans most readily demonstrate calcification/ossification of cervical discs and accompanying arthritic changes. Bulging/protruding can typically be managed nonsurgically. Alternatively, significantly extruded or sequestrated discs, resulting in moderate/marked spinal cord and/or nerve root compression may warrant surgery. Most operations from front of the neck for cervical discs are called anterior cervical discectomy/fusion (ACDF), while those performed from the back of the neck are called laminoforaminotomies.
Conclusion:Patients with cervical radiculopathy (root compression) and/or myelopathy (cord compression) with disc herniations on MR/CT studies may or may not require surgery.
Keywords: Anterior cervical discectomy/fusion, cervical discs, extruded, laminoforaminotomy, myelopathy, nonsurgical, radiculopathy, sequestrated, surgical
INTRODUCTION
Evaluation of patients for cervical disc disease starts with assessment of neurological symptoms (complaints) and signs (examination/neurological deficits). These findings are then closely correlated with radiographic pathology, documented utilizing a combination of X-rays [anteroposterior (AP), lateral, flexion, and extension], magnetic resonance (MR) images, and computed tomographic (CT) scans [Figures
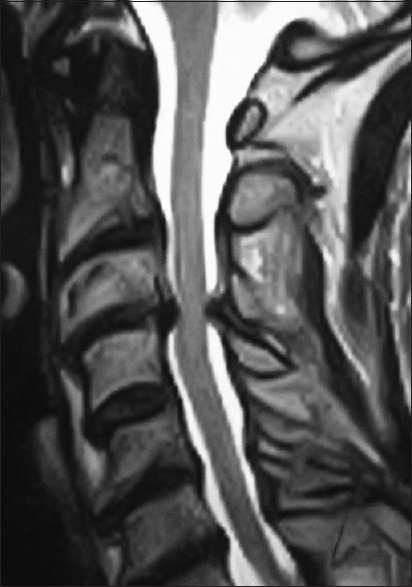
Figure 1
This is a sagittal (lateral or side view) T2-weighted cervical magnetic resonance (MR) scan (note the spinal fluid is hyperintense or white). There is an anterior central disc herniation at the C3-C4 level (in the front) accompanied by posterolateral laminar shingling (the C4 lamina is pushed under the lamina of C3) plus ossification of the yellow ligament
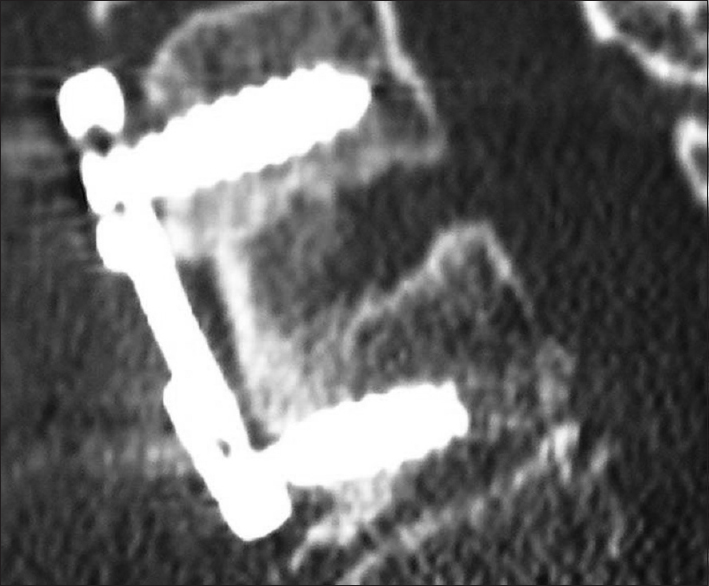
Figure 5
This patient underwent a two-level anterior cervical discectomy and fusion utilizing a dynamic ABC plate (Aesculap, Tuttlingen, Germany). This was performed for anterior cervical disc herniations at the C4-C5 and C6-C7 levels. The intervening level did not have to be fused as the patient had a prior multilevel posterior fusion
Figure 6
On this lateral x-ray (taken from the side), a one-level anterior cervical discectomy and fusion (ACDF) was performed using iliac crest autograft and a dynamic ABC plate. Note the graft between the vertebrae can be visualized, but the subsequent CT [
Figure 8
This lateral (side view) two dimensional computed tomography (CT) study best documents fusion across the graft/vertebral body junctions both superiorly (above) and inferiorly (below). Fusion is confirmed by the absence of lucency (no dark line), and the presence of bony trabeculation spanning the graft/body interfaces. Also observe how well you can see the graft, screws, and plate
Figure 9
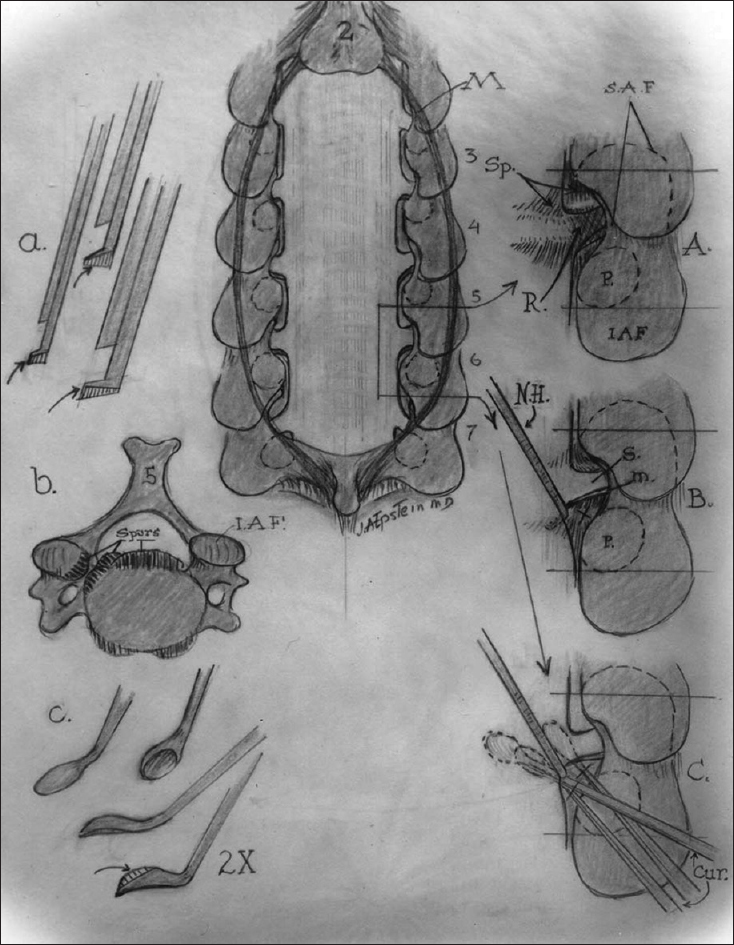
This illustration (Joseph A. Epstein MD, Copyright Nancy E. Epstein MD) demonstrates posterior cervical surgery, including a laminectomy and laminotomy. In
The majority of patients, who have just minimal bulging/protruding discs on MR and/or CT studies without significant spinal cord or nerve root, may be managed without surgery. Nevertheless, too many of these patients are presently offered and too many are undergoing “unnecessary” surgery. Alternatively, surgery is appropriate for patients with severe focal neurological deficits (root and/or cord compression) and MR and/or CT studies documenting large extruded/sequestrated soft or calcified discs resulting in “significant” spinal cord and/or nerve root compression.
ANATOMY OF THE CERVICAL SPINE
Bony anatomy of seven cervical vertebral bodies
In the cervical spine, there are seven vertebrae anteriorly (in the front), a central canal (e.g., where the spinal cord is located with the facet joints on each side), and the posterior elements (e.g., the laminae and spinous processes). At the C1 level, there is just an arch. Here, the odontoid process from C2 extends cephalad and is “lashed” in the front (anteriorly with ligaments) to the C1 arch.
Cervical cord and nerve roots
The spinal cord extends from the base of the brain through the cervical spinal canal to the thoracic spine below. Exiting from either side are the cervical nerve roots: C1-C8. The C1 root exits above the C1 arch, while the remaining roots exit inferior to the designated levels; e.g., at the C5-C6 level, the C6 root exits the canal.
Cervical discs
Discs are like shock absorbers facilitating flexibility/cushioning between the vertebral bodies. There is no disc at the C1-C2 level; but rather, they are located between the C2-C3 down through C7T1 levels. The disc itself is comprised of an outer annulus fibrosus (firm capsule), while the center contains the nucleus pulposus (more hydrated in younger patients, more desiccated in older patients). Between the discs and the vertebral bodies themselves are the cartilaginous end plates.
Yellow ligament
In the back of the cervical spine, on each side (not in the middle), the yellow ligament (ligamentum flavum) attaches to the mid portion of the lamina above and extends to the leading edge of the lamina below. Arthritic changes of this ligament (calcification/ossification) may contribute to significant spinal stenosis/cord compression/myelopathy.
Vertebral arteries of the cervical spine
In the cervical spine, the vertebral arteries travel through the foramen transversaria and exit at C2 crossing over through the ponticulus posticus. During anterior cervical and posterior cervical surgery, the vertebral arteries may be directly injured. Furthermore, with posterior surgery, lateral mass and pedicle screws may directly compromise the vertebral foramina, resulting potentially in vertebral artery perforation, brain stem infarction, and death.
Neurological symptoms of cervical discs
The most common complaints for cervical disc disease include neck pain, focal burning/numbness, tingling, or weakness in the arms or hands. Patients with radiculopathy have compression of a single or multiple nerve roots. Those with myelopathy, defined as cord compression, may experience these symptoms involving entire extremities (arms/hands/legs); rarely do they develop sphincter (bowel/bladder) dysfunction.
Gait evaluation
Pathological changes to the patient's gait may reflect different diseases in addition to cord compression. For example, a wide based gait and loss of balance may be seen with cervical myelopathy (e.g., large disc herniations/calcified discs with stenosis). Other changes in gait may be attributed to peripheral neuropathy (e.g., due to diabetes, B12 deficiency (combined systems disease), or even Parkinson's disease (e.g., magnetic-shuffling gait).
NEUROLOGICAL SIGNS
Motor deficits in the upper extremities with radiculopathy/myelopathy
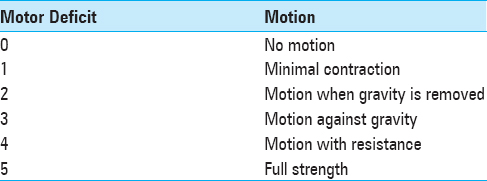
When discussing motor weakness, it is defined from 0 (no motor function) to 5 (normal function) [
Motor deficits in the lower extremities with cervical myelopathy
If patients have significant spinal cord compression/myelopathy, they may also demonstrate increased weakness involving the lower extremities; iliopsoas (elevator of the hip), quadriceps (straightening out the knee), extensor hallucis longus/dorsiflexors (holding the foot up in extension), or plantar flexor weakness (pushing the foot down).
Reflex deficits in the upper extremities with radiculopathy and myelopathy
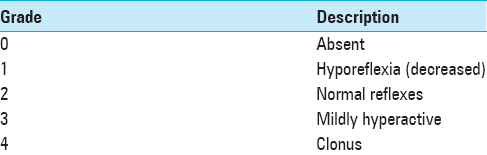
The reflexes in the upper and lower extremities are graded 0–4 [
Reflex deficits in the lower extremities with radiculopathy and myelopathy
Hyperactive reflexes in the lower extremities may also reflect compression of the spinal cord. These include evaluation of the patellar (knee reflex) and Achilles responses (ankle reflex) (e.g., with myelopathy these may be increased to the 3-4+ to 5 levels) along with assessment of Babinski signs (stimulate the bottom of the foot and the toes go up/extensor) [
SENSORY EXAMINATION
Pin appreciation and light touch (anterolateral spinothalamic tract)
Deficits to pin appreciation indicate compression of the anterior spinothalamic tract located in the front/sides of the spinal cord (anterolaterally). The sensory examination is performed using a pin (new one per patient) to determine whether the patient can feel a pinprick and light touch in the different cervical nerve root distributions. The major sensory deficits to pin appreciation are found in the following distributions. For C5 there is a loss of pin appreciation in a silver dollar over the upper arm. A C6 deficit to pin extends down the arm over the thumb and index finger, a C7 deficit involves mostly the third digit (often with some of the index finger mixed in). C8 root deficits involve the lateral aspect of the 4th digit and 5th digit. One must differentiate loss of pin appreciation in the hands from carpal tunnel (median nerve) or cubital tunnel (ulnar nerve) syndromes.
Vibration and position appreciation (posterior columns)
The posterior columns, located at the back of the spinal cord in the center, control vibration and position appreciation. Vibration is tested with a tuning fork placed over the bony prominences of the hands, knees, and ankles. Position testing involves elevation/lowering of the fingers/wrists and toes/ankles. Patients with severe cervical myelopathy (cord compression) may demonstrate a loss of vibration/position appreciation in the upper compared with the lower extremities.
Cerebellar examination
Patients with cervical disease and myelopathy may have “balance” problems.
Finger-Nose-Finger: The cerebellar exam includes assessment of the ability to put your finger to your nose-then touch the examiner's finger-and touch your nose again.
Heel to Shin: You ask the patient to run down with one ankle over the shin on the opposite side; if there is a lot of tremor/flailing, etc. this indicates dysfunction.
Tandem Gait Testing: This is tested by asking patients to walk on an imaginary line heel to toe to heel to toe. If they veer to one side or the other, or are off-balance, you have your answer.
SYMPTOMS AND SIGNS FOR SURGICAL CERVICAL DISCS
C5 nerve root deficits arising from pathology at the C4-C5 level
If a patient has unilateral (off to one side) compression of a C5 nerve root, they may exhibit weakness upon elevating the shoulder (deltoid deficit), a loss/diminution of the biceps reflex, and sensory loss of pin appreciation in the C5 distribution (silver dollar over the upper shoulder). If there is bilateral nerve root compression the deficit may be present on both sides. In the presence of marked cord compression, you may have both the C5 root deficits and cord findings.
C6 root deficits arising from pathology at the C5-C6 level
In a patient with unilateral C6 root compromise, the patient's motor deficit is characterized by trouble extending the wrist, opposing the thumb and index finger, and opposing the thumb (C6) and pinky (C7). The sensory deficit will be a loss of pin appreciation over the thumb and index finger (sometimes also over the middle digit). The reflex loss involves to some degree the biceps reflex response, but more so the brachioradialis (over the forearm). Cerebellar dysfunction may be characterized by the inability to perform finger-nose-finger without a tremor. If there is pathology bilaterally, the deficits will appear on both sides and may additionally include cord findings.
C7 root deficits from pathology at the C6-C7 level
A C7 motor deficit is characterized by weakness of apposition of the thumb (C6) and pinky (C7), marked focal weakness of extensors of the phalanges (C7), and triceps. This may be accompanied by a loss of the triceps reflex. Additionally, decreased pin appreciation may be noted over the third digit (sometimes there is “overflow” over to the index and 4th finger). If this deficit is bilateral, there may also be cord compressive symptoms/signs.
C8 root deficits from pathology at the C7-T1 level
A C8 root deficit is defined by weakness of the intrinsic demonstrated by spreading the fingers apart. There is no specific reflex loss. The sensory deficit is over the upper arm.
Diagnostic testing
After a complete neurological examination, diagnostic testing identifies the location of cervical disc disease (e.g., soft tissue or calcified). Noninvasive studies include x-rays, MR, and CT studies. Invasive modalities such as myelograms and myelogram-CT studies are only rarely utilized.
X-rays
Plain radiographs of the cervical spine are taken from the front (anterior/posterior or AP), from the side (lateral views), and also include flexion (bending forward) and extension studies (bending backward) to document stability. They may show normal alignment, or document vertebral body slippage, fractures, and dislocations. X-rays are still used to “clear” the cervical spine following trauma, but CT studies are more accurate. Following surgery (e.g., ACDF: anterior cervical discectomy and fusion) plain and dynamic x-rays may document graft/plate locale, and fusion [Figures
Magnetic resonance scans
MR scans utilize magnetic fields and radio waves to create images of the soft tissue and bony structures (showing the water content) of the cervical spine. MR best shows the soft tissues including the spinal cord, nerve roots, soft disc herniations, tumors, synovial cysts, enlarged yellow ligament, and other pathology on lateral (sagittal images), coronal (from the front), and axial (cross section) images [
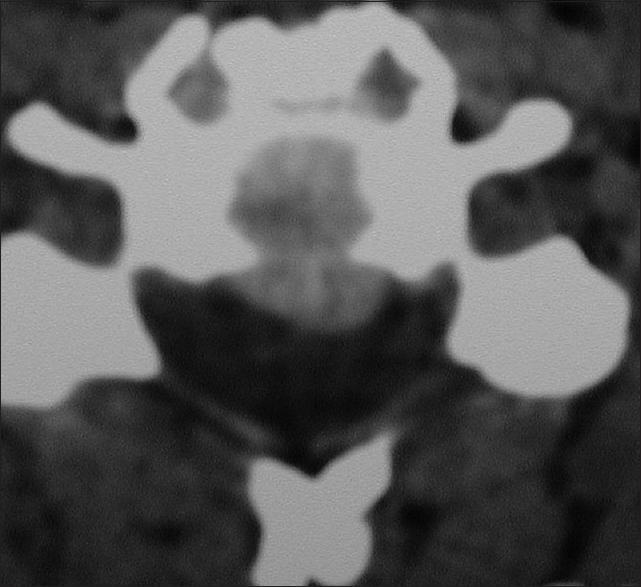
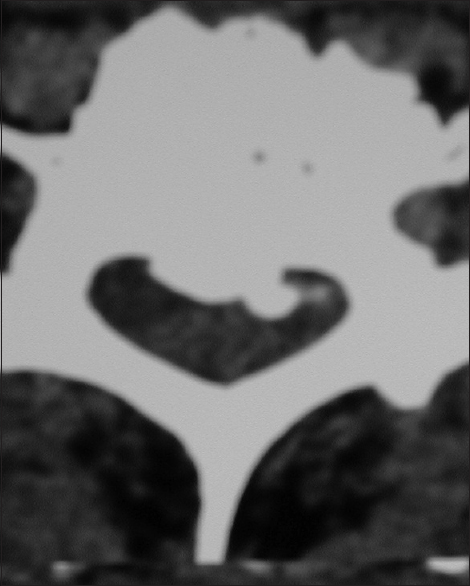
Computed tomography scans
Computerized tomography (CT) scans utilize x-ray images obtained from different angles and a computer to create a three-dimensional image of the spine. CT scans directly show the ossified/calcific changes of the discs, vertebral bodies, ligaments, and facet joints, [Figures
Conservative therapy
Why can most patients (e.g., up to 80%) with cervical disc herniations may be managed conservatively? First, many MR and CT studies are “overread,” meaning there is no significant spinal cord or nerve root compression, but those reading them exaggerate the findings to avoid “missing” something. Second, many patients with pain alone have no neurological deficits, and nonsurgical management should be considered. Conservative treatment includes: antiinflammatory medications, steroids, nerve transmitters, and muscle relaxants. Physical therapy, although sometimes helpful, if too rigorous may result in worsening of disc herniations. Typically, their efficacy simply coincides with the normal improvement of symptoms that would spontaneously over several successive months.
Contraindications to cervical epidural injections
The use of epidural steroid in the cervical spine is not approved by the Food and Drug Administration (FDA). More critically, they pose severe risks/complications that include: inadvertent injections into the cord itself resulting in quadriplegia, injection into the vertebral arteries resulting in stroke/death, injection directly into nerve roots resulting in focal paralysis, infection, abscess, and meningitis. Furthermore, they have no documented long-term efficacy.
Surgical options
There are various surgical options to deal with cervical disc herniations. If the discs are centrally located or anterolateral (somewhat off to the side), then an anterior approach (from the front) is typically warranted. For those that are extremely lateral or foraminal (way off to the side), a posterior approach may be utilized.
Neuroanesthesia for cervical spine surgery
Patients undergoing cervical surgery require physiological monitoring. This is initiated by placing electrodes over the brain, arms, wrists, legs, and ankles. Baseline recordings should be obtained prior to intubation, final positioning, and induction. They must then be recorded throughout the duration of surgery. Somatosensory evoked potentials (SSEP) monitor the back of the spinal cord, motor evoked potentials evaluate the anterior cord (e.g., anterior horns), while the electromyographs directly reflect irritation to the roots/muscles. To monitor these potentials successfully, anesthesia needs to utilize total intravenous anesthesia (TIVA) (e.g., without inhalant agents).
Anterior diskectomy/fusion
For disc herniations located anteriorly/anterolaterally, an ACDF may be necessary [Figures
Posterior diskectomy; laminoforaminotomy
For the disc that is very posterior and lateral/foraminal, performing disc removal from behind the neck can be accomplished by removing a portion of the lateral lamina above and below the level in question [
SUMMARY
Cervical disc disease needs to be appropriately diagnosed and treated. Patients may present with radiculopathy and/or myelopathy and neurological deficits that correlate with MR and/or CT findings of soft or calcified disc herniations. Most patients with cervical discs (e.g., 80%) respond to nonsurgical treatment; this should, however, not include epidural cervical injections that risk quadriplegia, stroke, and death. When surgery is warranted it may be performed from the front (ACDF) or behind (laminotomy). Notably, too many patients are subjected to unnecessary surgery, so the decision to have an operation should carefully considered, and other opinions obtained.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.