- Department of Neurological Surgery, Henry Ford Hospital, Detroit, Michigan, USA
Correspondence Address:
Thomas Noh
Department of Neurological Surgery, Henry Ford Hospital, Detroit, Michigan, USA
DOI:10.4103/sni.sni_474_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Thomas Noh, Rahul Chandra, Jimmy Kim, Ian Lee. A case of symptomatic spinal dural arteriovenous fistula after high-volume lumbar puncture. 01-Aug-2017;8:164
How to cite this URL: Thomas Noh, Rahul Chandra, Jimmy Kim, Ian Lee. A case of symptomatic spinal dural arteriovenous fistula after high-volume lumbar puncture. 01-Aug-2017;8:164. Available from: http://surgicalneurologyint.com/surgicalint-articles/a-case-of-symptomatic-spinal-dural-arteriovenous-fistula-after-high%e2%80%91volume-lumbar-puncture/
Abstract
Background:Spinal dural arteriovenous fistulas (DAVFs) are rare lesions that lead to venous congestion and ischemic injury resulting in neurologic deterioration. Here we present a patient diagnosed with glioblastoma multiforme (GBM) who became symptomatic from a spinal DAVF after a diagnostic high-volume lumbar puncture (LP).
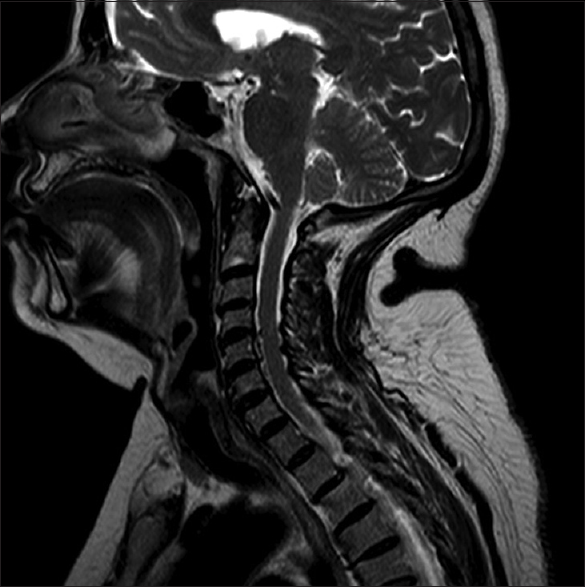
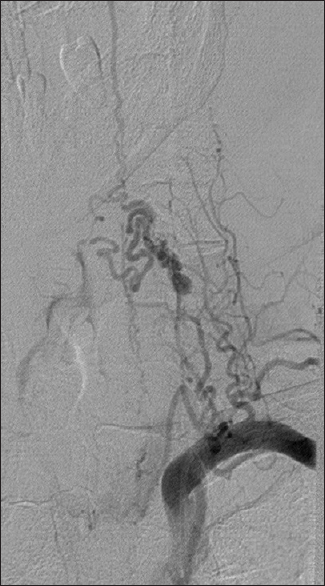
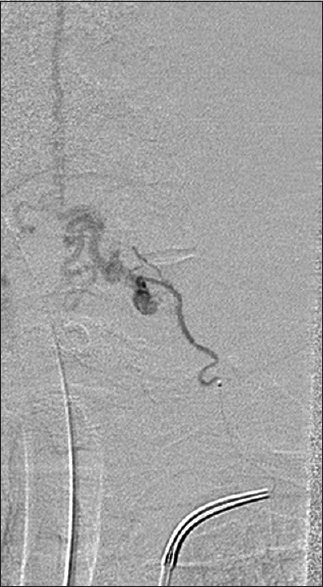
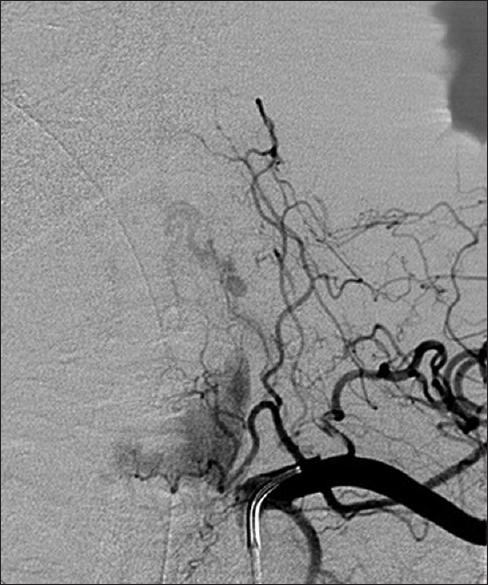
Case Description:When a 72-year-old female developed partial seizures in her left upper extremity without other focal neurological deficits, she underwent a magnetic resonance imaging (MRI) scan of the brain. The MRI revealed a right frontal/posterior corpus callosal lesion. She next had a MR-guided high-volume LP. A GBM was diagnosed following a biopsy. Postoperatively, after the LP, she was noted to have bilateral deltoid and bilateral 4/5 lower extremity weakness, with diffuse hyperreflexia. The MRI and magnetic resonance angiogram (MRA) of the cervical spine demonstrated a large venous varix at the C5-C6 level within the left neural foramen. She underwent successful complete embolization of two thyrocervical branches with direct communication to an enlarged anterior spinal artery. One month later, her neurological examination returned to baseline; she was walking independently with only 4+/5 residual weakness in her left lower extremity.
Conclusions:Here we report a patient with a cranial GBM and an incidental cervical spinal C5-C6 DAVF that became symptomatic after a high-volume LP. It is possible that the high-volume LP increased vascular congestion, thus precipitating the onset of cervical myelopathy.
Keywords: Arteriovenous malformation, dural arteriovenous fistula, glioblastoma multiforme, lumbar puncture, magnetic resonance angiography, magnetic resonance imaging
INTRODUCTION
Dural arteriovenous fistulas (DAVFs) are the most common vascular malformations of the spinal cord (1 out of 100,000 per year). Initial neurological symptoms include gait imbalance, numbness, and paresthesias.[
An acute decrease in cerebrospinal fluid (CSF) pressure attributed to a lumbar puncture (LP) may lead to the sudden engorgement of dural and epidural veins, resulting in medullary/cord ischemia.[
CASE DESCRIPTION
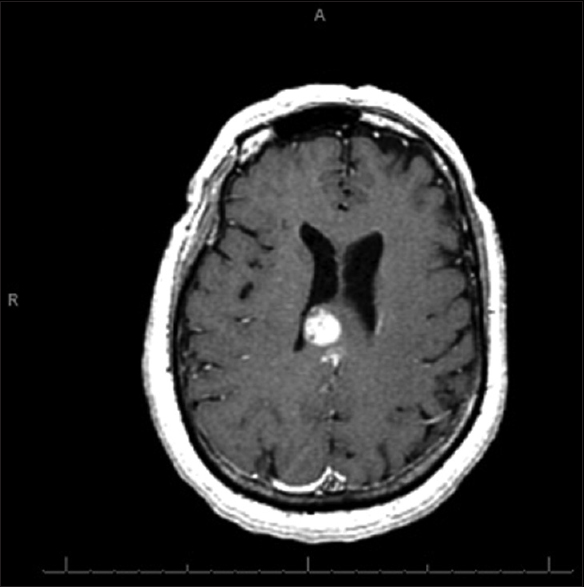
A 72-year-old female presented with partial seizures in her left upper extremity, but no other focal neurological deficit. Magnetic resonance imaging (MRI) of the brain revealed a right frontal/posterior corpus callosal enhancing lesion involving the internal capsule and crossing the midline [
DISCUSSION
This case highlights the emergence of a subacute neurological deficit following a high-volume LP in a patient with a cranial GBM. Both the MRI and MRA of the cervical spine ultimately demonstrated a large venous varix in the left neural foramen at the C5-C6 level. The most likely etiology of this patient’s myelopathy was acute/subacute increased vascular congestion of the DAVF following the high-volume LP.
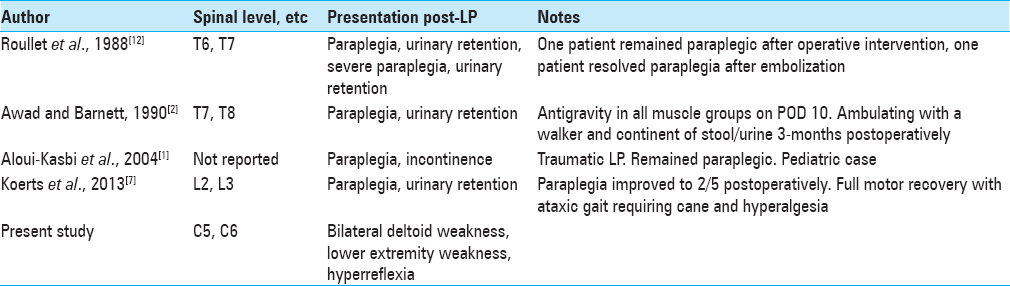
This phenomenon has been previously reported with thoracic arteriovenous malformations (AVMs). Roullet et al. described a patient whose T6/7 AVM became symptomatic after LP;[
DAVFs involve a single feeding artery connected to intradural veins. The decrease in CSF pressure caused by the LP may have exacerbated vascular congestion, as also documented by Monro-Kellie leading to focal hyperemia.[
The diagnosis of DAVFs can be established with MRI and confirmed with MRA-angiography.[
CONCLUSION
Here we report a patient with a cranial GBM and an incidental cervical spinal DAVF (C5-C6) that became symptomatic after a high-volume LP. Likely, the high-volume LP caused an increase in vascular congestion thus precipitating her cervical myelopathy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aloui-Kasbi N, Chaker M, Felah S, Mattousi N, Allani H, Bellagha I. Spinal vascular malformation in a child, revealed by lumbar puncture. Arch Pediatr. 2004. 11: 815-8
2. Awad IA, Barnett GH. Neurological deterioration in a patient with a spinal arteriovenous malformation following lumbar puncture. Case report. J Neurosurg. 1990. 72: 650-3
3. Bertuccio A, Robba C, Spena G, Versari PP. Intracranial and spinal dural arterio-venous fistula (DAVF): A surgical series of 107 patients. Acta Neurochir Suppl. 2016. 123: 177-83
4. Burtis MT, Ulmer JL, Miller GA, Barboli AC, Koss SA, Brown WD. Intradural spinal vein enlargement in craniospinal hypotension. AJNR Am J Neuroradiol. 2005. 26: 34-8
5. Kellie G. Appearances observed in the dissection of two individuals; Death from cold and congestion of the brain. Tr Med-Chir Soc Edinb. 1824. 1: 84-
6. Kim WY, Kim JB, Nam TK, Kim YB, Park SW. Cervical myelopathy caused by intracranial dural arteriovenous fistula. Korean J Spine. 2016. 13: 67-70
7. Koerts G, Vanthuyne V, Delavallee M, Rooijakkers H, Raftopoulos C. Spinal dural arteriovenous fistula presenting with paraplegia following lumbar puncture. J Neurosurg Spine. 2013. 19: 57-60
8. Lasjaunias P, Chiu M, ter Brugge K, Tolia A, Hurth M, Bernstein M. Neurological manifestations of intracranial dural arteriovenous malformations. J Neurosurg. 1986. 64: 724-30
9. Miller JD, Stanek AE, Langfitt TW. A comparison of autoregulation to changes in intracranial and arterial pressure in the same preparation. Eur Neurol. 1971. 6: 34-8
10. Mokri B. The Monro-Kellie hypothesis: Applications in CSF volume depletion. Neurology. 2001. 56: 1746-8
11. Monro A.editorsObservations on the Structure and Functions of the Nervous System [Electronic Resource]: Illustrated with Tables by Alexander Monro. Edinburgh, London: Printed for and sold by William Creech and Joseph Johnson; 1783. p.
12. Roullet E, Netter JM, Chiras J, Mahieux F, Amarenco P, Marteau R. Spinal dural arteriovenous fistulae: Exacerbation after myelography with metrizamide. Rev Neurol (Paris). 1988. 144: 371-5
13. Sood D, Mistry KA, Khatri GD, Chadha V, Garg S, Suthar PP. Congestive myelopathy due to intradural spinal AVM supplied by Artery of Adamkiewicz: Case report with brief literature review and analysis of the Foix-Alajouanine Syndrome definition. Pol J Radiol. 2015. 80: 337-43
14. Toossi S, Josephson SA, Hetts SW, Chin CT, Kralik S, Jun P. Utility of MRI in spinal arteriovenous fistula. Neurology. 2012. 79: 25-30