- Norton Neuroscience Institute, Norton Healthcare, Louisville, Kentucky, USA
- Neurodiagnostic Center of Louisville, Louisville, Kentucky, USA
- Department of Neurological Surgery, University of Louisville School of Medicine, Louisville, Kentucky, USA
Correspondence Address:
Christopher B. Shields
Norton Neuroscience Institute, Norton Healthcare, Louisville, Kentucky, USA
Department of Neurological Surgery, University of Louisville School of Medicine, Louisville, Kentucky, USA
DOI:10.4103/sni.sni_492_17
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Lisa B. E. Shields, Vasudeva G. Iyer, Yi Ping Zhang, Christopher B. Shields. Acute cauda equina syndrome following orthopedic procedures as a result of epidural anesthesia. 10-Apr-2018;9:81
How to cite this URL: Lisa B. E. Shields, Vasudeva G. Iyer, Yi Ping Zhang, Christopher B. Shields. Acute cauda equina syndrome following orthopedic procedures as a result of epidural anesthesia. 10-Apr-2018;9:81. Available from: http://surgicalneurologyint.com/surgicalint-articles/acute-cauda-equina-syndrome-following-orthopedic-procedures-as-a-result-of-epidural-anesthesia/
Abstract
Background:Cauda equina syndrome (CES) is a rare complication of spinal or epidural anesthesia. It is attributed to direct mechanical injury to the spinal roots of the cauda equina that may result in saddle anesthesia and paraplegia with bowel and bladder dysfunction.
Case Description:The first patient underwent a hip replacement and received 5 mL of 1% lidocaine epidural anesthesia. Postoperatively, when the patient developed an acute CES, the lumbar magnetic resonance imaging (MRI) scan demonstrated clumping/posterior displacement of nerve roots of the cauda equina consistent with adhesive arachnoiditis attributed to the patient's previous L4-L5 lumbar decompression/fusion. The second patient underwent spinal anesthesia (injection of 10 mg of isobaric bupivacaine for an epidural block) for a total knee replacement. When the patient developed an acute CES following surgery, the lumbar MRI scan showed an abnormal T2 signal in the conus and lower thoracic spinal cord over 4.3 cm.
Conclusions:Acute CES should be considered in patients undergoing spinal or epidural anesthesia for joint replacement surgery. Prompt evaluation with MRI studies may lead to appropriate medical/surgical measures to reverse the deficit.
Keywords: Anesthesia, arachnoiditis, cauda equina syndrome, lumbar spinal stenosis, neurosurgery, spine
INTRODUCTION
Cauda equina syndrome (CES) is infrequent and may be associated with spinal/epidural anesthesia. Several etiologies have been proposed for CES, including direct or indirect neural trauma, inadvertent dural puncture, infection, and/or increased ischemia to the cord attributed to the lithotomy position.[
We present two cases of CES following epidural anesthesia attributed to adhesive arachnoiditis/prior surgical scar and inappropriate needle placement.
CASE REPORTS
Case report 1
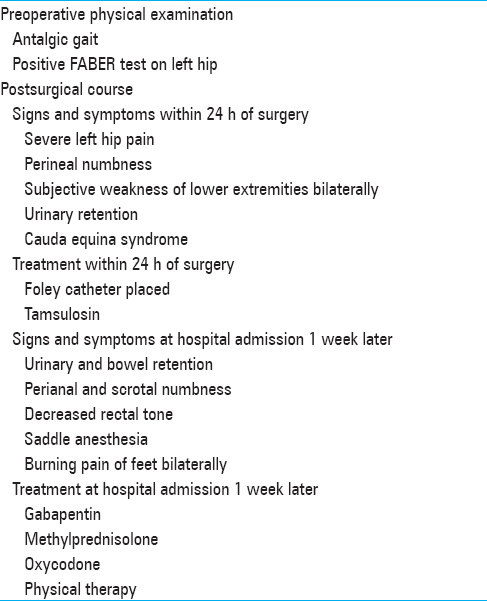
A 59-year-old male [height 6', weight 250 lbs (113.4 kg); body mass index (BMI) 33.91 kg/m2] presented with a 2-year history of groin and left hip pain without radicular symptoms [
The patient underwent a left total hip arthroplasty from an anterior approach. Prior to surgery, he received 5 mL 1% lidocaine epidural anesthesia through a catheter while seated. He immediately noted paresthesias in the left leg. The 17 G Tuohy needle was moved to the right, and the catheter was subsequently threaded 5 cm without paresthesia, blood, or CSF return. A 3 mL test dose was given, and there was no paresthesia. The patient was discharged home 6 h postoperatively. Within 24 h of surgery, he returned to the emergency department with urinary retention and a CES [
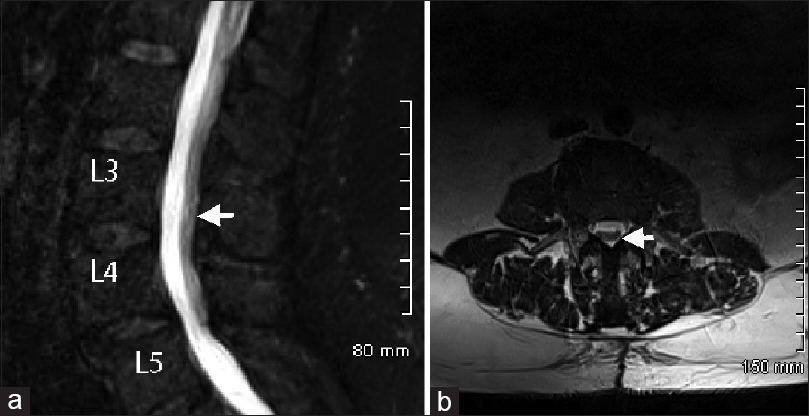
A lumbar magnetic resonance imaging (MRI) with and without gadolinium contrast revealed multilevel lumbar spondylosis and clumping/posterior displacement of nerve roots of the cauda equina from L2-3 through L5-S1 compatible with arachnoiditis due to the prior surgery [Figure
Case report 2
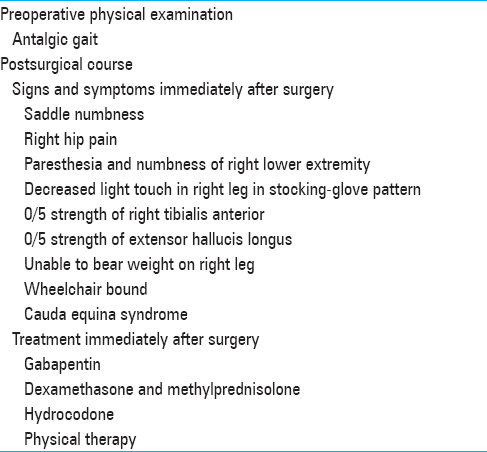
A 61-year-old female [height 5'3”, weight 260 lbs (117.9 kg); BMI 46.07 kg/m2) underwent a right total knee arthroplasty utilizing a femoral nerve block (e.g., single-shot epidural block) and general anesthesia [
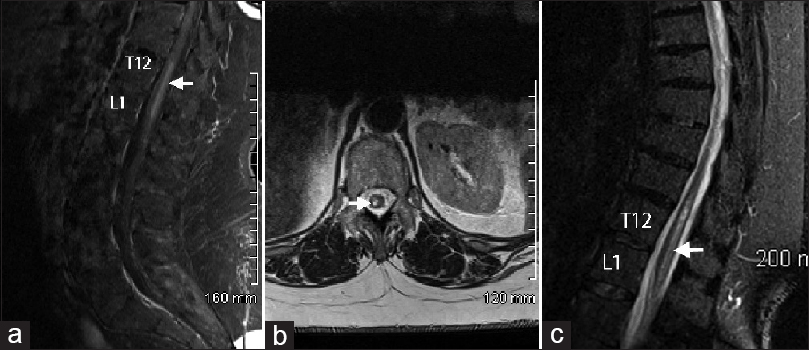
Postoperative thoracic and lumbar MRI scans with and without gadolinium contrast revealed an abnormal T2 signal in the conus and lower thoracic spinal cord over a 4.3 cm segment along with postoperative changes [Figure
Figure 2
(a) Sagittal and (b) axial views of a thoracic magnetic resonance imaging (MRI) scan revealed evidence of abnormal T2 signal in the conus over a 4.3 cm segment (arrows). (c) Sagittal view of a thoracic MRI scan performed 2 months later showed that the enhancement within the conus and the cord swelling had decreased, however, there were mild residual T2 signal changes (arrow)
DISCUSSION
Cauda equina syndrome has been reported in the setting of spinal or epidural anesthesia involving a host of local anesthetics, including bupivacaine, lidocaine, ropivacaine, and tetracaine.[
Few studies have implicated pre-existing lumbar pathology as playing an integral role in the development of CES following spinal or epidural anesthesia.[
Lumbosacral adhesive arachnoiditis resulting in CES may be attributed to the following: agents injected into the subarachnoid space, infection in the subarachnoid space, space occupying lesions such as neurofibroma, subarachnoid hemorrhage, vertebral trauma, or after spinal surgeries.[
Here, CES in our first case was attributed to epidural anesthesia administered in the presence of lumbar adhesive arachnoiditis in a patient who had a prior L4-5 laminectomy/fusion. Despite treatment with gabapentin, methylprednisolone, oxycodone, and physical therapy, he experienced no improvement of his symptoms. In the second case, the CES was attributed to the anesthesiologist's placing a needle at the L1-2 interspace. Direct injection into the cord/conus likely contributed to this neurological injury.
Physicians should be alert to the rare complication of CES that may arise following spinal or epidural anesthesia. Special attention should focus on patients who have undergone previous lumbar surgical intervention and may have developed adhesive arachnoiditis. Prompt identification of the precise etiology of CES permits timely treatment that may curtail or ameliorate the devastating consequences associated with this condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chabbouh T, Lentschener C, Zuber M, Jude N, Delaitre B, Ozier Y. Persistent cauda equina syndrome with no identifiable facilitating condition after an uneventful single spinal administration of 0.5% hyperbaric bupivacaine. Anesth Analg. 2005. 101: 1847-8
2. Gerancher JC. Cauda equina syndrome following a single spinal administration of 5% hyperbaric lidocaine through a 25-gauge Whitacre needle. Anesthesiology. 1997. 87: 687-9
3. Kubina P, Gupta A, Oscarsson A, Axelsson K, Bengtsson M. Two cases of cauda equina syndrome following spinal-epidural anesthesia. Reg Anesth. 1997. 22: 447-50
4. Moussa T, Abdoulaya D, Youssouf C, Oumar GC, Karim TS, Traore TJ. Cauda equina syndrome and profound hearing loss after spinal anesthesia with isobaric bupivacaine. Anesth Analg. 2006. 102: 1863-4
5. Pleym H, Spigset O. Peripheral neurologic deficits in relation to subarachnoid or epidural administration of local anesthetics for surgery. A survey of 21 cases. Acta Anaesthesiol Scand. 1997. 41: 453-60
6. Rice I, Wee MY, Thomson K. Obstetric epidurals and chronic adhesive arachnoiditis. Br J Anaesth. 2004. 92: 109-20
7. Stambough JL, Stambough JB, Evans S. Acute cauda equina syndrome after total knee arthroplasty as a result of epidural anesthesia and spinal stenosis. J Arthroplasty. 2000. 15: 375-9
8. Takasu M, Okita M, Araki T, Tanitame N, Tamura A, Suwaki N. Gadolinium enhancement of cauda equina after combined spinal-epidural anaesthesia. Br J Radiol. 2010. 83: e192-4
9. Vianna PT, Resende LA, Ganem EM, Gabarra RC, Yamashita S, Barreira AA. Cauda equina syndrome after spinal tetracaine: electromyographic evaluation--20 years follow-up. Anesthesiology. 2001. 95: 1290-1
10. Wu KC, Chiang YY, Lin BC, Su HT, Poon KS, Shen ML. Epidural cyst with cauda equina syndrome after epidural anesthesia. Acta Anaesthesiol Taiwan. 2010. 48: 148-51