- Department of Neurosurgery, National Institute of Mental Health and Neurosciences, Bengaluru, Karnataka, India
- Department of Neuropathology, National Institute of Mental Health and Neurosciences, Bengaluru, Karnataka, India
Correspondence Address:
A. R. Prabhuraj
Department of Neuropathology, National Institute of Mental Health and Neurosciences, Bengaluru, Karnataka, India
DOI:10.4103/sni.sni_117_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Ajit M. Mishra, A. R. Prabhuraj, Nupur Pruthi, Shilpa Rao. Adult intramedullary epidermoid cyst without spinal dysraphism: A case report. 18-Jun-2018;9:122
How to cite this URL: Ajit M. Mishra, A. R. Prabhuraj, Nupur Pruthi, Shilpa Rao. Adult intramedullary epidermoid cyst without spinal dysraphism: A case report. 18-Jun-2018;9:122. Available from: http://surgicalneurologyint.com/surgicalint-articles/adult-intramedullary-epidermoid-cyst-without-spinal-dysraphism-a-case-report/
Abstract
Background:Intramedullary epidermoid cyst (IEC), typically associated with spinal dysraphism, is rare, with fewer than 80 such cases reported in the literature. Here we present an adult with an IEC without spinal dysraphism.
Case Description:A 41-year-old female presented with the gradual onset of a progressive spastic paraparesis attributed to a magnetic resonance imaging (MRI)-documented D8-9 intramedullary lesion. Following microsurgical excision of the IEC, she fully recovered.
Conclusion:IECs are rare lesions, typically found in conjunction with spinal dysraphism. Utilizing MRI studies to document the lesion location, gross total microsurgical excision is the procedure of choice. Early excision of these benign lesions maximizes functional recovery.
Keywords: Dysraphism, epidermoid, intramedullary, spinal
INTRODUCTION
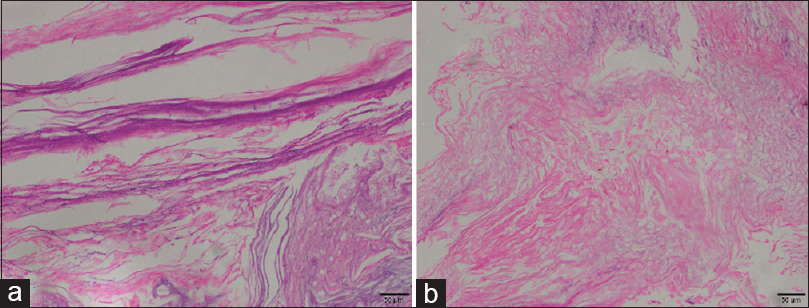
Inclusion of ectodermal tissue remnants, entrapped during the 3rd and 5th week of gestation during neural tube closure, gives rise to epidermoid cysts.[
Here, we present an adult with an IEC identified on magnetic resonance (MR) at the D8-9 level that was successfully excised without residual neurological deficit or recurrence (e.g., at 6 months.)
CASE REPORT
A 41-year-old female presented with a progressive spastic paraparesis (e.g., left greater than right) of 2 years duration accompanied by 1 month of urinary incontinence. The examination revealed right lower extremity motor function at 2/5, left at 4/5, diffuse lower extremity hyperreflexia, bilateral Babinski responses, and a relative bilateral T12 sensory level.
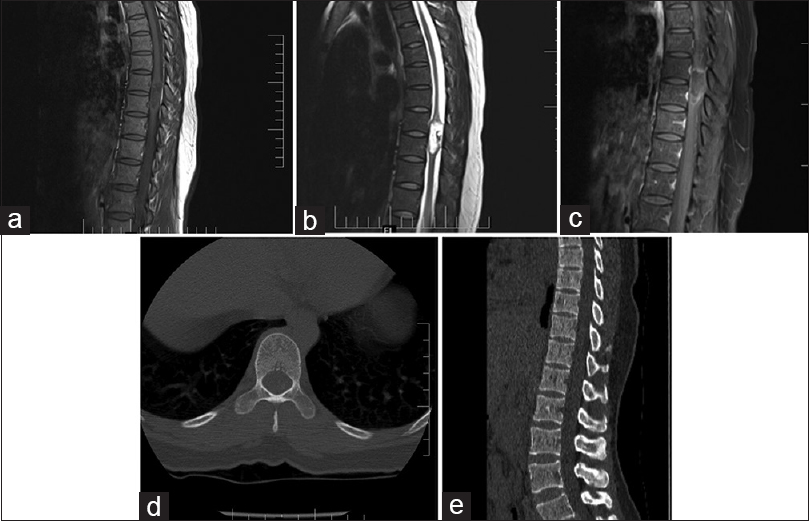
The MR image revealed a well-defined intramedullary lesion at the D8-9 level, measuring 3.1 × 1.2 × 1.2 cm (vertical, anterior–posterior, transverse diameter). It was hypointense on T1, hyperintense on T2-weighted images, with a faint rim of enhancement with post gadolinium diethylenetriamine pentaacetate (GD-DTPA) injection [
DISCUSSION
Spinal IEC in adults constitutes <1% of intramedullary tumors.[
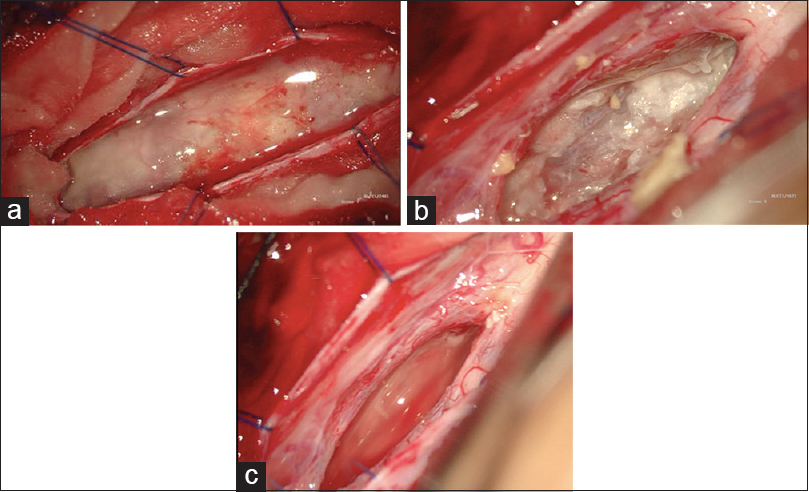
Although microsurgical excision provides the best chance for cure, if lesion's capsules are densely populated surrounding normal neural tissues, then they should be left in place to avoid increasing surgical/neurological dysfunction/morbidity.[
CONCLUSION
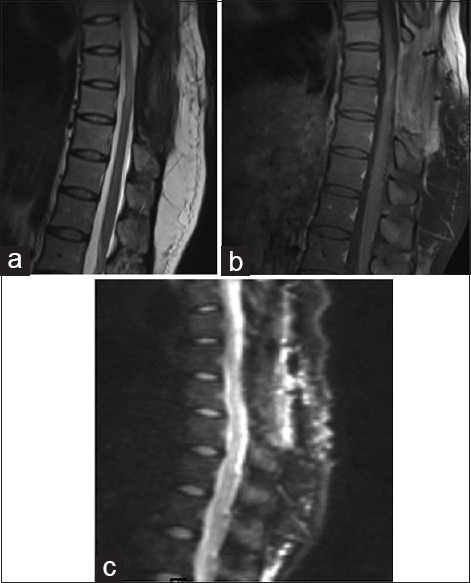
IECs are rare in adults without spinal dysraphism. Here, an adult presented with a 2-month history of a progressive paraparesis and an MR-documented T8-9 lesion. Six months following microsurgical subtotal excision of the IEC (e.g. residual posterior capsule densely adherent to the cord), the patient recovered 4+/5 motor function and, the MR documented no tumor recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Babayev R, Abbasov B, Eksi MS. Thoracic intramedullary epidermoid cyst—timely fashion diagnosis and treatment. Childs Nerv Syst. 2015. 31: 793-6
2. Bansal S, Ailawadhi P, Suri A, Kale SS, Sarat Chandra P, Singh M. Ten years’ experience in the management of spinal intramedullary tumors in a single institution. J Clin Neurosci. 2013. 20: 292-8
3. Bretz A, Van den Berge D, Storme G. Intraspinal epidermoid cyst successfully treated with radiotherapy: Case report. Neurosurgery. 2003. 53: 1429-31
4. Chandra PS, Manjari T, Devi BI, Chandramouli BA, Srikanth SG, Shankar SK. Intramedullary spinal epidermoid cyst. Neurol India. 2000. 48: 75-7
5. Graillon T, Rakotozanany P, Meyer M, Dufour H, Fuentes S. Intramedullary epidermoid cysts in adults: Case report and updated literature review. Neurochirurgie. 2017. 63: 99-102
6. Kukreja K, Manzano G, Ragheb J, Medina LS. Differentiation between pediatric spinal arachnoid and epidermoid-dermoid cysts: Is diffusion-weighted MRI useful?. Pediatr Radiol. 2007. 37: 556-60