- Department of Neurosurgery, Tokyo Women's Medical University, Kawada-cho, Shinjuku-ku, Tokyo, Japan
- Department of Neurosurgery, Tokyo Women's Medical University, Yachiyo Medical Center, Yachiyo, Chiba
Correspondence Address:
Tomonori Kobayashi
Department of Neurosurgery, Tokyo Women's Medical University, Kawada-cho, Shinjuku-ku, Tokyo, Japan
DOI:10.4103/sni.sni_239_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuichi Mochizuki, Tomonori Kobayashi, Akitsugu Kawashima, Takayuki Funatsu, Takakazu Kawamata. Chronic subdural hematoma of the posterior fossa treated by suboccipital craniotomy. 05-Feb-2018;9:20
How to cite this URL: Yuichi Mochizuki, Tomonori Kobayashi, Akitsugu Kawashima, Takayuki Funatsu, Takakazu Kawamata. Chronic subdural hematoma of the posterior fossa treated by suboccipital craniotomy. 05-Feb-2018;9:20. Available from: http://surgicalneurologyint.com/surgicalint-articles/chronic-subdural-hematoma-of-the-posterior-fossa-treated-by-suboccipital-craniotomy/
Abstract
Background:Chronic subdural hematoma (CSDH) of the posterior fossa is uncommon in adults. Only a few cases have been reported, and most of these were secondary to head injury or anticoagulant therapy. We herein describe a case of successful surgical treatment of CSDH in the posterior fossa after surgical removal of a large supratentorial and infratentorial dermoid cyst.
Case Description:A 71-year-old woman underwent removal of a left supratentorial and infratentorial dermoid cyst via a left transzygomatic approach. Three years, 6 months after surgery, screening computed tomography revealed CSDH in the supratentorial and infratentorial regions. Four months later, the patient was transferred to the emergency department with cerebellar ataxia, vomiting, and deterioration of consciousness. Two hematomas, one in the supratentorial region and one in the infratentorial region, were greatly compressing the brain, and seemed to be separate lesions. It was difficult to judge on computed tomography whether there was communication between these two hematoma cavities. The patient underwent hematoma removal via suboccipital craniotomy for the posterior fossa CSDH to resolve brain stem compression. Burr-hole irrigation was used for the supratentorial CSDH to avoid upper herniation. The patient recovered uneventfully and was discharged with no neurological deficits.
Conclusion:Although the optimal treatment for CSDH of the posterior fossa remains unclear because of the limited number of previous reports, direct decompression of the posterior fossa via suboccipital craniotomy should be considered, especially when CSDH exists primarily at the cerebellopontine angle and strongly compresses the brain stem.
Keywords: Chronic subdural hematoma, craniotomy, dermal cyst, posterior fossa, trepanation
INTRODUCTION
Chronic subdural hematoma (CSDH) of the posterior fossa is uncommon in adults. Only a few cases have been reported,[
CASE REPORT
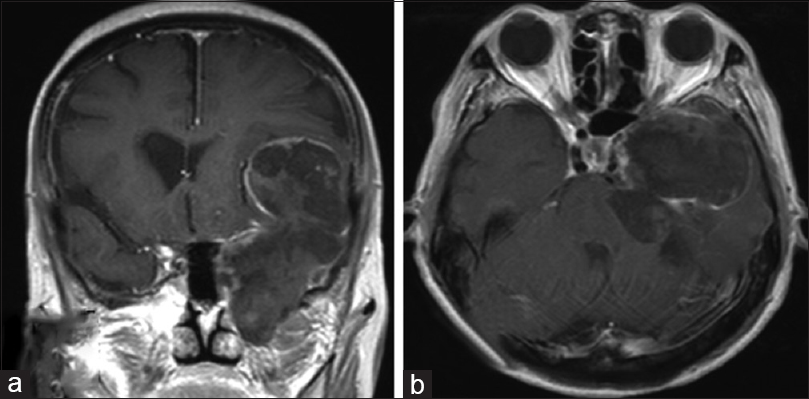
An asymptomatic 71-year-old woman was diagnosed with a left supratentorial and infratentorial dermoid cyst on screening magnetic resonance imaging (MRI) [
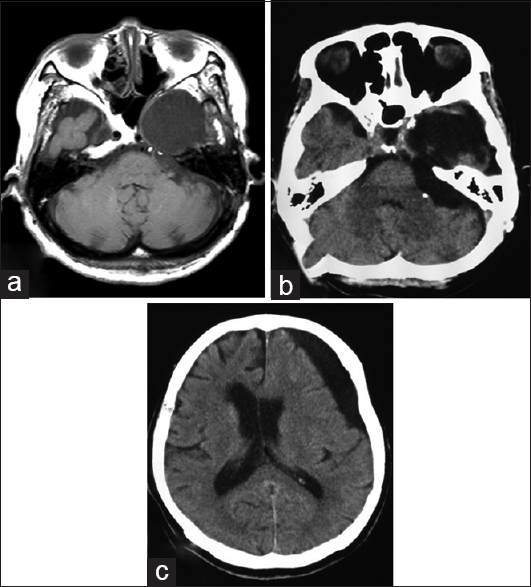
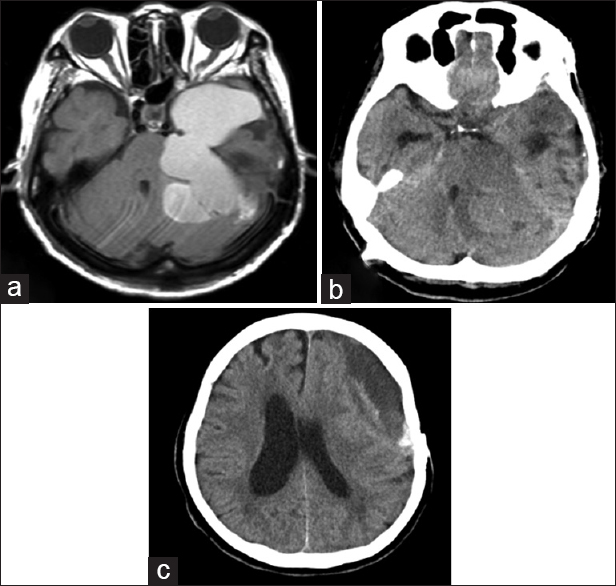
Figure 3
Imaging findings upon admission. (a) T1-weighted magnetic resonance imaging with contrast enhancement on admission showed a signal change from low to mildly high within the cavity. (b) Computed tomography on admission revealed low and iso-density of the infratentorial lesion with compression of the brain stem. (c) The supratentorial lesion also exhibited mixed density on computed tomography
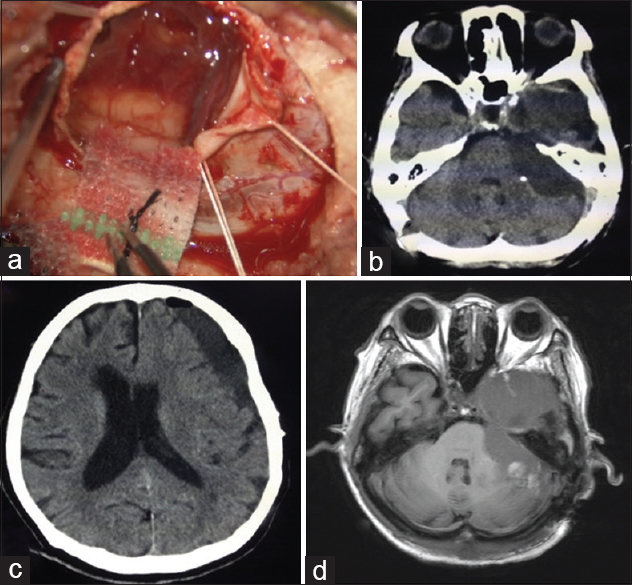
Figure 4
Intraoperative and postoperative findings. (a) Intraoperative image after dural incision shows the outer membrane of the haematoma on the cerebellar hemisphere. (b and c) Computed tomography after haematoma evacuation shows removal of the haematoma and resolution of the brain stem compression. (d) Postoperative MRI shows signal change in the cavity
DISCUSSION
The reported incidence of postoperative CSDH is 1.6% after brain tumor surgery, and the period between craniotomy and development of CSDH ranges from 3 to 5 months (mean, 4.3 months).[
CSDH of the posterior fossa is rare in adults.[
Previous reports have described surgical drainage (craniotomy or trepanation) and conservative therapy for treatment of CSDH.[
We finally confirmed the presence of communication between the supratentorial and infratentorial compartments and observed drainage to the infratentorial space upon irrigation of the supratentorial portion. Because we opened the top and bottom of the long hematoma cavity, including both the supratentorial and infratentorial portions, gravity induced the formation of a spontaneous drainage route, and complete removal of the hematoma was achieved.
CONCLUSION
We have herein described suboccipital craniotomy with supratentorial burr-hole irrigation for resolution of brain stem compression resulting from CSDH in the posterior fossa, with a good functional outcome. From a clinical viewpoint, we recommend that clinicians consider direct decompression of the posterior fossa via suboccipital craniotomy, especially when CSDH exists primarily in the cerebellopontine angle and strongly compresses the brain stem.
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this article.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initial will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Costa LB, De Andrade A, Fonseca Valadão G. Chronic subdural hematoma of the posterior fossa associated with cerebellar hemorrhage: Report of a rare disease with MRI findings. Arq Neuropsiquiatr. 2004. 62: 170-2
2. Kurisu K, Kawabori M, Niiya Y, Ohta Y, Mabuchi S, Houkin K. Bilateral chronic subdural hematomas of the posterior fossae. Neurol Med Chir (Tokyo). 2012. 52: 822-5
3. Stendel R, Schulte T, Pietila TA, Suess O, Brock M. Spontaneous bilateral chronic subdural haematoma of the posterior fossa. Case report and review of the literature. Acta Neurochir (Wien). 2002. 144: 497-500
4. Takahashi Y, Ohkura A, Sugita Y, Sugita S, Miyagi J, Shigemori M. Postoperative Chronic Subdural Hematoma Following Craniotomy. Neurol Med Chir. 1995. 35: 78-81
5. Takami H, Oshiro N, Hiraoka F, Murao M, Ide T. Rapid resolution of a spontaneous large chronic subdural haematoma in the posterior fossa under conservative treatment with platelet administration to aplastic anaemia. Clin Neurol Neurosurg. 2013. 115: 2236-9