- Department of Clinical Neuroscience, University of Tokushima, Tokushima, Japan
- Department of Neurosurgery, University of Tokushima, Tokushima, Japan
Correspondence Address:
Yuki Yamamoto
Department of Clinical Neuroscience, University of Tokushima, Tokushima, Japan
DOI:10.4103/sni.sni_46_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Yuki Yamamoto, Nobuaki Yamamoto, Junichiro Satomi, Izumi Yamaguchi, Masaaki Korai, Yasuhisa Kanematsu, Yasushi Takagi, Ryuji Kaji. Dural arteriovenous fistula in the superior orbital fissure: A case report. 07-May-2018;9:95
How to cite this URL: Yuki Yamamoto, Nobuaki Yamamoto, Junichiro Satomi, Izumi Yamaguchi, Masaaki Korai, Yasuhisa Kanematsu, Yasushi Takagi, Ryuji Kaji. Dural arteriovenous fistula in the superior orbital fissure: A case report. 07-May-2018;9:95. Available from: http://surgicalneurologyint.com/surgicalint-articles/dural-arteriovenous-fistula-in-the-superior-orbital-fissure-a-case-report/
Abstract
Background:Dural arteriovenous fistulas (dAVFs) are extremely rare in the superior orbital fissure, and they exhibit ocular symptoms similar to the dAVF in the cavernous sinus because of the intraorbital venous congestion. Hence, the distinction of these conditions is imperative because of some inherent differences in endovascular treatment techniques.
Case Description:A 58-year-old woman presented with a gradually worsening left eyeball protrusion and conjunctival congestion. The digital subtraction angiography revealed a dAVF with a shunting point in the left superior orbital fissure. Moreover, the inferolateral trunk of the left internal carotid artery and the left middle meningeal artery were involved as feeding arteries. Shunting blood flow drained into the facial vein through the superior ophthalmic vein (SOV) but not into the cavernous sinus, which was located just posterior to the superior orbital fissure. We performed transvenous coil embolization in the SOV through the facial vein, and the symptoms disappeared completely.
Conclusion:We experienced a case of a dAVF in the superior orbital fissure. This case presented a possibility of the presence of one subtype of the dAVF in the part of the cavernous sinus separated at the superior orbital fissure in front. Transvenous coil embolization in the SOV through the facial vein efficiently occluded the fistula.
Keywords: Dural arteriovenous fistula, superior orbital fissure, superior ophthalmic vein, transvenous coil embolization
INTRODUCTION
Dural arteriovenous fistulas (dAVFs) are abnormal direct connections between arteries and veins in the dura mater,[
CASE REPORT
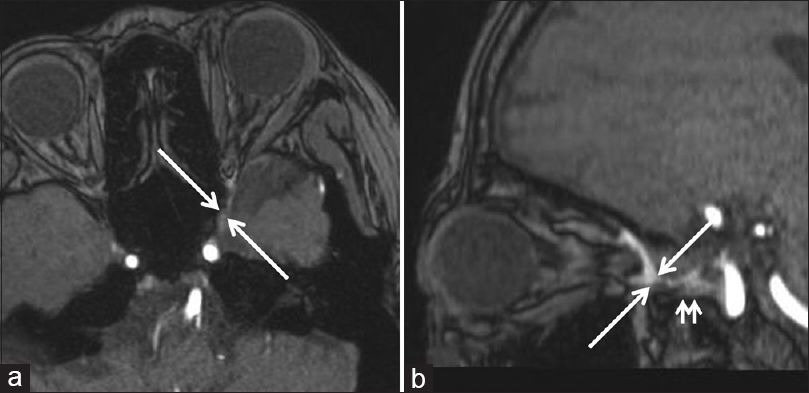
A 58-year-old woman without a previous medical and traumatic history presented with gradually worsening pulsatile proptosis and chemosis in her left eye. The initial examination revealed eye movement disturbance (abduction and elevation) and diplopia. Although ophthalmologic examination showed no visual acuity reduction or defect of visual field, it showed dilation of the retinal vein. The three-dimensional time-of-flight magnetic resonance (MR) angiography identified a high-intensity signal in the left SOV and the inferior ophthalmic vein (IOV) [
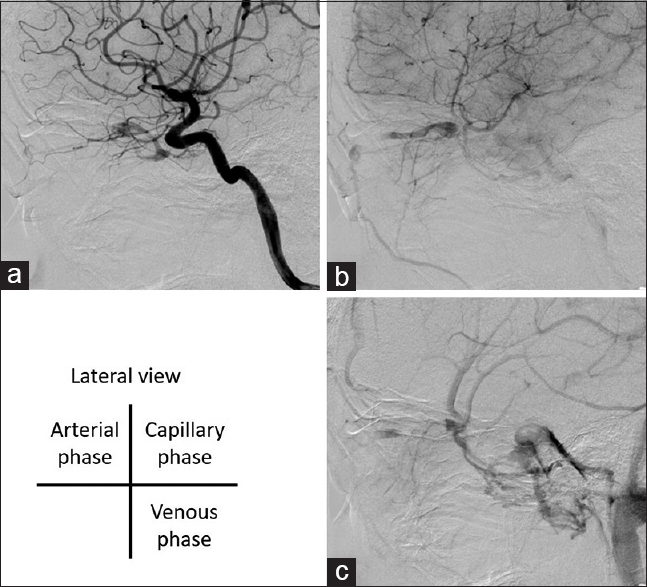
Figure 2
(a) The left internal carotid artery angiography (ICAG) reveals an arteriovenous fistula between the ILT of the internal carotid artery and the SOV. (b) Shunting blood flow drains from the SOV to the facial vein through the angular vein and not into the cavernous sinus. (c) In the venous phase of the ICAG, the cavernous sinus is revealed as normal intracranial venous return pathway (lateral view)
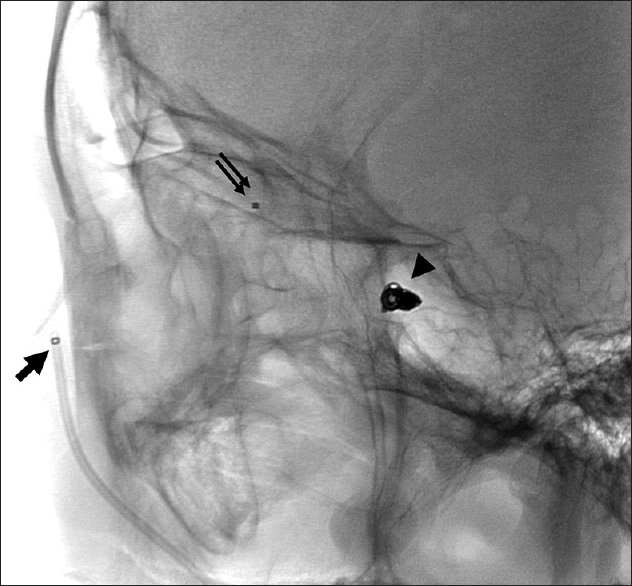
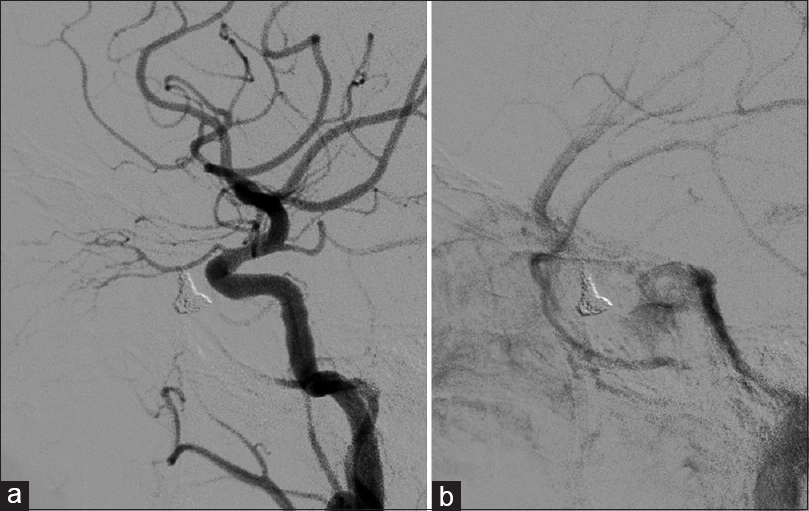
We planned transvenous coil embolization in the SOV at the left superior orbital fissure. Accordingly, we placed a 6-Fr guiding catheter (ENVOY, Codman Neurovascular) in the left internal jugular vein under local anesthesia and by the right femoral vein approach. We tried to precede a microcatheter using an approach route from the inferior petrosal sinus and the cavernous sinus to the SOV. However, as the connection between the cavernous sinus and the SOV could not be opened, any guidewire could not pass through it. Hence, we shifted to the anterior approach, placed a 4-Fr intermediate catheter (Cerulean G; Medikit) in the left facial vein, and preceded a microcatheter (Renegade; Stryker) to the shunting point in the SOV. We embolized the SOV using nine detachable coils (Orbit Galaxy 3–8 mm, Codman; Target nano 2–3 mm, Stryker) [
DISCUSSION
This dAVF case was characterized by the presence of a shunting point in the superior orbital fissure and separated from the cavernous sinus. dAVFs with a shunting point around the orbit are sporadic. Intraorbital AVF is only one out of 350 patients who received DSA suspected of cavernous sinus dAVF.[
Endovascular therapy for dAVFs is broadly categorized into transarterial and transvenous embolization. In this case, the ILT of the carotid artery and the MMA were involved as feeding arteries. However, transarterial embolization, especially using liquid embolizing materials, would be dangerous in this condition because the ILT branch (the anteromedial branch that runs through the superior orbital fissure) has a potential anastomosis with the ophthalmic artery.[
CONCLUSION
We experienced a rare dAVF case with a shunting point in the superior orbital fissure. The report suggests that detailed evaluations of the DSA and other neuroradiological imaging are imperative to distinguish dAVFs from CSdAVFs. From the perspective of the location of the shunting point and the type of feeding arteries, this case was considered a rare subtype of CSdAVF, and transvenous coil embolization by the facial vein approach an effective treatment of this condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Biondi A, Milea D, Cognard C, Ricciardi GK, Bonneville F, van Effenterre R.editors. Cavernous sinus dural fistulae treated by transvenous approach through the facial vein: Report of seven cases and review of the literature. Am J Neuroradiol. 2003. 24: 1240-6
2. Caragine LP, Halbach VV, Dowd CF, Higashida RT. Intraorbital arteriovenous fistulae of the ophthalmic veins treated by transvenous endovascular occlusion: Technical case report. Oper Neurosurg. 2006. 58:
3. Cheng KC, Chang CH, Lin WC. Spontaneous resolution of intraorbital arteriovenous fistulas. Ophthal Plast Reconstr Surg. 2009. 25: 245-7
4. Deguchi J, Yamada M, Ogawa R, Kuroiwa T. Transvenous embolization for a purely intraorbital arteriovenous fistula, Case report. J Neurosurg. 2005. 103: 756-9
5. Hayreh SS. Orbital vascular anatomy. Eye. 2006. 20: 1130-44
6. Hamada J, Morioka M, Kai Y, Sakurama T, Kuratsu J. Spontaneous arteriovenous fistula of the orbit: Case report. Surg Neurol. 2006. 65: 55-7
7. Kiyosue H, Tanoue S, Hongo N, Sagara Y, Mori H. Artery of the superior orbital fissure: An undescribed branch from the pterygopalatine segment of the maxillary artery to the orbital apex connecting with the anteromedial branch of the inferolateral trunk. Am J Neuroradiol. 2015. 36: 1741-7
8. Kobkitsuksakul C, Jiarakongmun P, Chanthanaphak E, Pongpech S. Noncavernous arteriovenous shunts mimicking carotid cavernous fistulae. Diagn Intervent Radiol. 2016. 22: 555-9
9. Lin CJ, Blanc R, Clarençon F, Piotin M, Spelle L, Williams M. Transvenous embolization of an intraorbital arteriovenous fistula using Onyx. J Clin Neurosci. 2010. 17: 783-5
10. Naqvi J, Laitt R, Leatherbarrow B, Herwadkar A. A case of a spontaneous intraorbital arteriovenous fistula: Clinico-radiological findings and treatment by transvenous embolisation via the superior ophthalmic vein. Orbit. 2013. 32: 124-6
11. Stiebel-Kalish H, Setton A, Nimii Y, Kalish Y, Hartman J, Huna Bar-On R. Cavernous sinus dural arteriovenous malformations: Patterns of venous drainage are related to clinical signs and symptoms. Ophthalmology. 2002. 109: 1685-91
12. Williamson RW, Ducruet AF, Crowley RW, McDougall CG, Albuquerque FC. Transvenous coil embolization of an intraorbital arteriovenous fistula: Case report and review of the literature. Neurosurgery. 2013. 72: E130-4