- Department of Neurosurgery, Dokkyo Medical University Koshigaya Hospital, Koshigaya-shi, Saitama, Japan
Correspondence Address:
Ryuta Nakae
Department of Neurosurgery, Dokkyo Medical University Koshigaya Hospital, Koshigaya-shi, Saitama, Japan
DOI:10.4103/sni.sni_193_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryuta Nakae, Masaya Nagaishi, Akio Hyodo, Kensuke Suzuki. Embolization of a spinal dural arteriovenous fistula with ethylene-vinyl alcohol copolymer (Onyx) using a dual-lumen microballoon catheter and buddy wire technique. 01-Aug-2017;8:166
How to cite this URL: Ryuta Nakae, Masaya Nagaishi, Akio Hyodo, Kensuke Suzuki. Embolization of a spinal dural arteriovenous fistula with ethylene-vinyl alcohol copolymer (Onyx) using a dual-lumen microballoon catheter and buddy wire technique. 01-Aug-2017;8:166. Available from: http://surgicalneurologyint.com/surgicalint-articles/embolization-of-a-spinal-dural-arteriovenous-fistula-with-ethylene%e2%80%91vinyl-alcohol-copolymer-onyx-using-a-dual%e2%80%91lumen-microballoon-catheter-and-buddy-wire-technique/
Abstract
Background:N-butyl 2-cyanoacrylate (NBCA) remains the standard embolic agent for spinal dural arteriovenous fistula (SDAVF) treatment. Treatment of SDAVF with ethylene-vinyl alcohol copolymer (Onyx, ev3-Covidien, Irvine CA, USA) is currently not well established. Although several cases have reported the use of Onyx to embolize an intracranial dural arteriovenous fistula using a dual-lumen microballoon catheter, Onyx embolization of an SDAVF using a dual-lumen microballoon catheter has not been reported.
Case Description:We treated a 57-year-old man with an SDAVF using a dual-lumen microballoon catheter and buddy wire technique to perform transarterial Onyx embolization via the left sixth intercostal artery.
Conclusions:Onyx embolization using a dual-lumen microballoon catheter was effective. Furthermore, the buddy wire technique was useful for providing rigid support of the microcatheter in a narrow and tortuous intercostal artery.
Keywords: Balloon catheter, buddy wire technique, ethylene-vinyl alcohol copolymer, Onyx, spinal dural arteriovenous fistula
INTRODUCTION
Endovascular embolization has become an accepted alternative to surgical management of spinal dural arteriovenous fistula (SDAVF).[
CASE PRESENTATION
History and examination
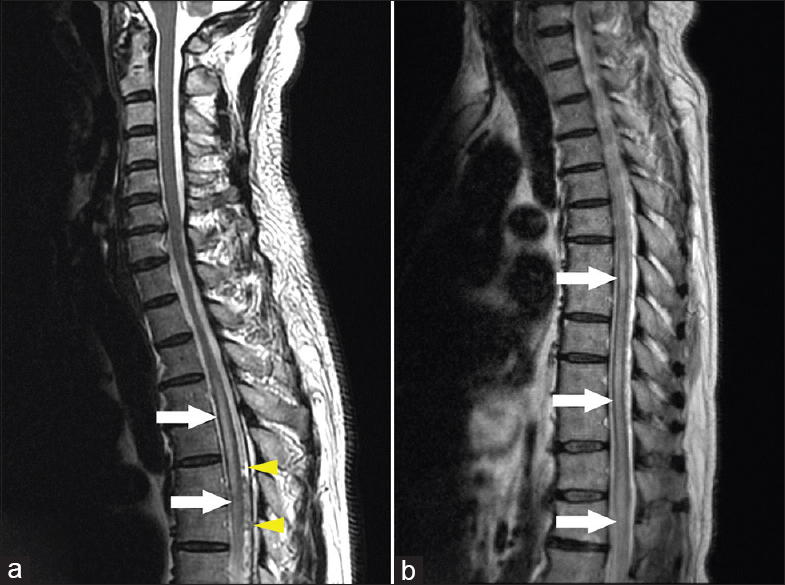
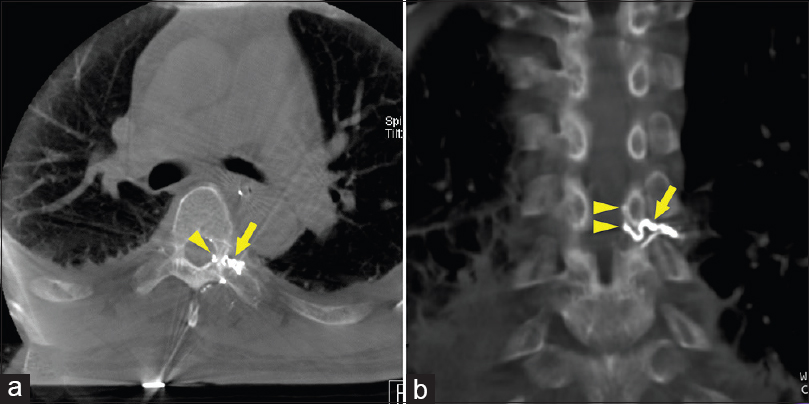
A 57-year-old male, with an 18-month history of urinary incontinence and 15 months of progressive lower extremity numbness, presented with a 10 days of increased lower extremity weakness. The patient had no history of trauma. The neurological examination documented a bilateral paraparesis (manual muscle testing 2/5) accompanied by mild hyporeflexia and dysesthesia relative T9 sensory level. The spinal magnetic resonance imaging (MRI) study revealed spinal cord edema T3 to the conus medullaris and enlarged perimedullary thoracic veins; these findings were consistent with a SDAVF [
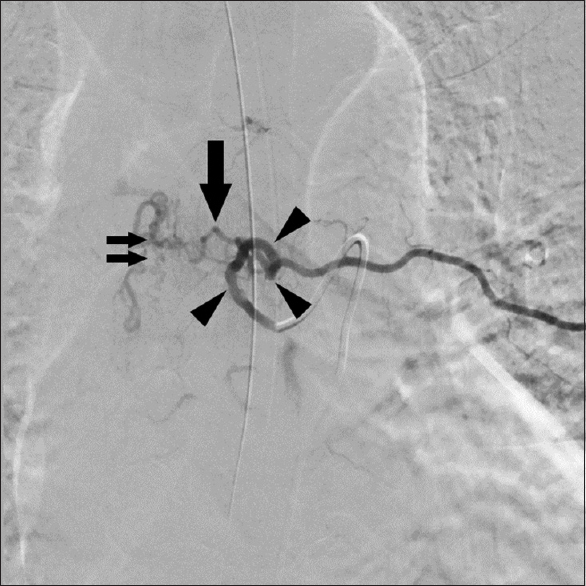
Figure 2
Anterior view of selective injection of the left sixth intercostal artery via a 4 Fr catheter demonstrates a spinal dural arteriovenous fistula supplied by a radiculomeningeal artery (large arrow) and drained through enlarged perimedullary veins (small double arrows). The course of the left sixth intercostal artery was tortuous and its orifice was narrow (arrowheads)
Selective embolization procedure
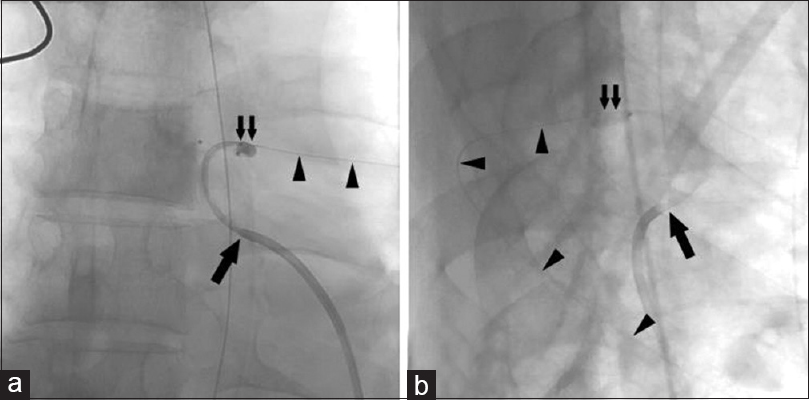
Five days after admission, we performed a super selective embolization. Under general anesthesia, a 6 Fr introducer sheath was inserted into the right femoral artery. Following arterial access, 4000 U of heparin was injected and an activated clotting time of 275 s was achieved. Our attempts to catheterize the left sixth intercostal artery orifice using a 5 Fr guiding catheter (CX catheter-A II Michaelson type, Gadelius Medical, Tokyo, Japan) over a 0.035-inch outer diameter guidewire (Radifocus, Terumo, Tokyo, Japan) were unsuccessful; we could not advance both a guidewire and guiding catheter. However, we were able to navigate a 0.0165-inch inner diameter microcatheter (Excelsior SL-10, Stryker, Fremont, CA, USA) into the distal left sixth intercostal artery over a 0.014-inch outer diameter, 200 cm microguidewire (CHIKAI, Asahi Intecc, Nagoya, Japan). We exchanged the microguidewire for a 0.014-inch outer diameter, 300 cm microguidewire (Aguru, Boston Scientific, Marlborough, MA, USA), and the guiding catheter and microcatheter for a 5 Fr multipurpose guiding catheter (Envoy, Codman and Shurtleff, Raynham, MA, USA). Insertion of the microguidewire into the distal left sixth intercostal artery as a buddy wire stabilized the guiding catheter in the artery orifice [
Figure 3
Anterior (a) and lateral views (b). A 5 Fr guiding catheter is inserted into the left sixth intercostal artery orifice (large arrow). A buddy wire is shown in the left sixth intercostal artery (arrowheads) and a dual-lumen microballoon catheter is shown in the dorsal spinal artery (small double arrows) during balloon inflation
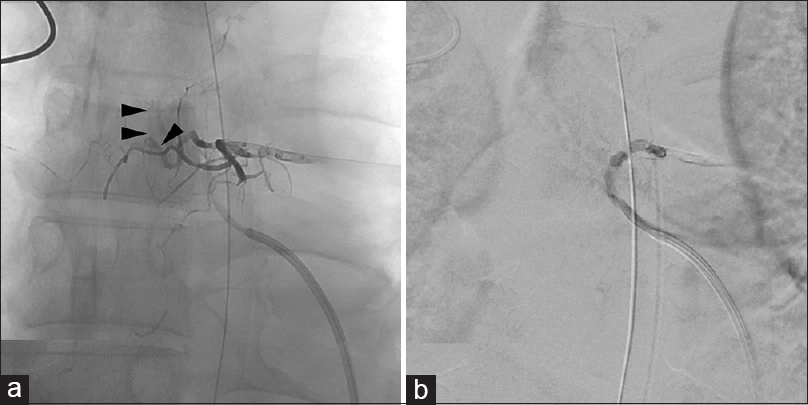
Figure 4
(a) Unsubtracted fluoroscopic image obtained postprocedure shows the Onyx cast. Note the dense penetration of Onyx into the proximal perimedullary veins (arrowheads). (b) Anterior view of selective injection of the left sixth intercostal artery postprocedure demonstrates occlusion of the spinal dural arteriovenous fistula
Postoperative course
Lower extremity weakness markedly improved within three postprocedure weeks, and his urinary and sensory symptoms partially resolved at 6 months. The thoracic MRI 3 months postprocedure revealed the spinal cord edema had resolved, and the enlarged perimedullary veins were no longer visible [
DISCUSSION
The goal of surgical and endovascular SDAVF treatment is to permanently obliterate the fistula and its draining vein.[
NBCA is currently the standard embolic agent for SDAVF; however, the permanent cure rates are not high. Niimi et al.[
Viscosity of Onyx
The viscosity of Onyx, a liquid embolic agent, makes it useful for the endovascular treatment of intracranial dural arteriovenous fistula; however, Onyx has only been used to treat SDAVF in 10 patients.[
Disadvantages of Onyx
However, some disadvantages of Onyx should be noted.[
Super selective embolization of SDAVF
To perform super selective embolization of SDAVF safely, the guiding catheter must be inserted into the intercostal artery for rigid support of the microcatheter. However, this can be difficult to achieve because the caliber of the orifice of the intercostal arteries is often small, and their course can be looped or elongated. Nishino et al.[
CONCLUSION
This case highlights two points. First, Onyx can be used to successfully treat SDAVF via a dual-lumen microballoon catheter. Second, the buddy wire technique is effective for providing rigid support of the microcatheter in narrow and tortuous intercostal arteries. Our initial experience indicates that Onyx embolization using a dual-lumen microballoon catheter is effective for the treatment of SDAVF, as it facilitates controlled penetration of the embolic agent into the draining vein.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adamczyk P, Amar AP, Mack WJ, Larsen DW. Recurrence of “cured” dural arteriovenous fistulas after Onyx embolization. Neurosurg Focus. 2012. 32: E12-
2. Bakker NA, Uyttenboogaart M, Luijckx GJ, Eshghi OS, Mazuri A, Metzemaekers JD. Recurrence rates after surgical or endovascular treatment of spinal dural arteriovenous fistulas: A meta-analysis. Neurosurgery. 2015. 77: 137-44
3. Gokhale S, Khan SA, McDonagh DL, Britz G. Comparison of surgical and endovascular approach in management of spinal dural arteriovenous fistulas: A single center experience of 27 patients. Surg Neurol Int. 2014. 5: 7-
4. Jagadeesan BD, Grigoryan M, Hassan AE, Grande AW, Tummala RP. Endovascular balloon-assisted embolization of intracranial and cervical arteriovenous malformations using dual-lumen coaxial balloon microcatheters and Onyx: Initial experience. Neurosurgery. 2013. 73: ons238-43
5. Jellema K, Sluzewski M, van Rooij WJ, Tijssen CC, Beute GN. Embolization of spinal dural arteriovenous fistulas: Importance of occlusion of the draining vein. J Neurosurg Spine. 2005. 2: 580-3
6. Niimi Y, Berenstein A, Setton A, Neophytides A. Embolization of spinal dural arteriovenous fistulae: Results and follow-up. Neurosurgery. 1997. 40: 675-
7. Nishino K, Ito Y, Hasegawa H, Kikuchi B, Fujii Y, Tanaka R. Modified buddy wire technique for coil embolization of posterior circulation aneurysms. Neuroradiology. 2007. 49: 49-55
8. Nogueira RG, Dabus G, Rabinov JD, Ogilvy CS, Hirsch JA, Pryor JC. Onyx embolization for the treatment of spinal dural arteriovenous fistulae: Initial experience with long-term follow-up. Technical case report. Neurosurgery. 2009. 64: E197-8
9. Sivakumar W, Zada G, Yashar P, Giannotta SL, Teitelbaum G, Larsen DW. Endovascular management of spinal dural arteriovenous fistulas. A review. Neurosurg Focus. 2009. 26: E15-
10. Song JK, Gobin YP, Duckwiler GR, Murayama Y, Frazee JG, Martin NA. N-butyl 2-cyanoacrylate embolization of spinal dural arteriovenous fistulae. AJNR Am J Neuroradiol. 2001. 22: 40-7
11. Spiotta AM, James RF, Lowe SR, Vargas J, Turk AS, Chaudry MI. Balloon-augmented Onyx embolization of cerebral arteriovenous malformations using a dual-lumen balloon: A multicenter experience. J Neurointerv Surg. 2015. 7: 721-7
12. Steinmetz MP, Chow MM, Krishnaney AA, Andrews-Hinders D, Benzel EC, Masaryk TJ. Outcome after the treatment of spinal dural arteriovenous fistulae: A contemporary single-institution series and meta-analysis. Neurosurgery. 2004. 55: 77-87
13. Warakaulle DR, Aviv RI, Niemann D, Molyneux AJ, Byrne JV, Teddy P. Embolisation of spinal dural arteriovenous fistulae with Onyx. Neuroradiology. 2003. 45: 110-2