- Center for Minimally Invasive Spinal Surgery, ShinYurigaoka General Hospital, Kawasaki, Kanagawa 215-0026, Japan
- Spine Section, Department of Neurosurgery, Southern Tohoku Research Institute for Neuroscience, Koriyama, Japan
- Uchikado Neuro-Spine Clinic, Fukuoka, Japan
Correspondence Address:
Hidenori Matsuoka
Center for Minimally Invasive Spinal Surgery, ShinYurigaoka General Hospital, Kawasaki, Kanagawa 215-0026, Japan
DOI:10.4103/sni.sni_204_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hidenori Matsuoka, Yukoh Ohara, Yoshiyuki Tomita, Nahoko Kikuchi, Yoshitaka Hirano, Hisaaki Uchikado, Junichi Mizuno. Initial radiological findings utilizing titanium basket for cervical open door laminoplasty. 07-Sep-2017;8:217
How to cite this URL: Hidenori Matsuoka, Yukoh Ohara, Yoshiyuki Tomita, Nahoko Kikuchi, Yoshitaka Hirano, Hisaaki Uchikado, Junichi Mizuno. Initial radiological findings utilizing titanium basket for cervical open door laminoplasty. 07-Sep-2017;8:217. Available from: http://surgicalneurologyint.com/surgicalint-articles/initial-radiological-findings-utilizing-titanium-basket-for-cervical-open-door-laminoplasty/
Abstract
Background:Cervical laminoplasty, utilizing different spacers to ’’keep the door open,’’ is the gold standard in Japan for treating ossification of the posterior longitudinal ligament (OPLL) and cervical spondylotic myelopathy (CSM). Here, we utilized a novel titanium ’’basket’’ spacer (Laminoplasty Basket: L-Basket; Ammtec, Tokyo) to perform open door cervical laminoplasty to keep the “door open” while also allowing for bony fusion across the open door.
Methods:Twenty-seven patients with/without OPLL were treated with open door laminoplasty utilizing the basket spacer. Patients were analyzed with preoperative/postoperative JOA scores, and X-rays/computed tomography (CT) at least 12 months (range, 12–19 months) postoperatively.
Results:Improvement from the preoperative JOA score of 10.3 points to the postoperative JOA of 14.8 points was noted 3 months postoperatively. There were no complications except one patient who had transient C5 palsy. Twelve months postoperatively, X-rays/CT documented fusion on both the open (62%) and hinge sides (90.2%); circumferential fusion was observed 59.8% of the time.
Conclusion:This titanium “basket” spacer (Laminoplasty Basket: L-Basket; Ammtec, Tokyo) promoted bone union between the spacer and both lamina, lateral masses following cervical laminoplasty without undue complications.
Keywords: Bone union, novel titanium spacer, open door laminoplasty
INTRODUCTION
Open door cervical laminoplasty is a well-established procedure for treating patients with multilevel cervical spondylotic myelopathy (CSM) and ossification of the posterior longitudinal ligament (OPLL) in Japan. There are many types of artificial hydroxyapatite (HA) spacers and titanium plates have been utilized to “keep the door open.”[
MATERIALS AND METHODS
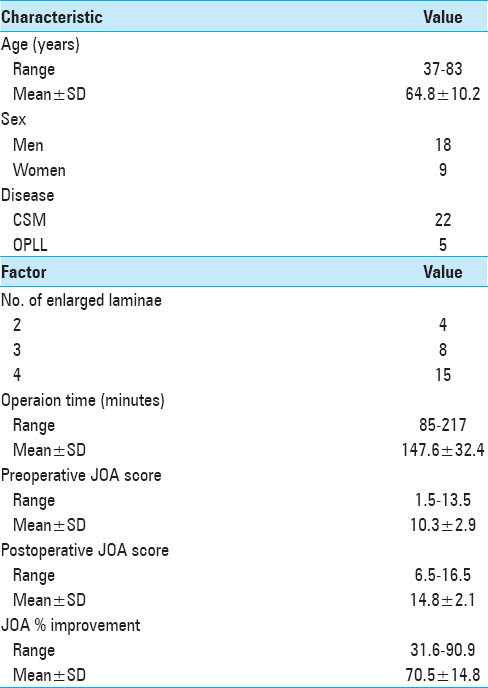
We retrospectively reviewed the medical records and clinical outcomes of 27 consecutive patients who underwent open door laminoplasty utilizing the L-Basket for cervical degenerative disease and OPLL. Postoperative X-ray and computed tomography (CT) studies were analyzed a minimum of 12-months postoperatively (follow-up period, 12–19 months). Preoperative deficits included myelopathy (94.1%) and radiculopathy (5.8%). Of the 27 cases (18 men and 9 women), the average preoperative JOA score was 10.3. All patients underwent preoperative X-ray, magnetic resonance (MR), and CT evaluations; 22 (81.5%) had cervical spondylosis and 5 (18.5%) had OPLL.
Surgical technique of open-door laminoplasty
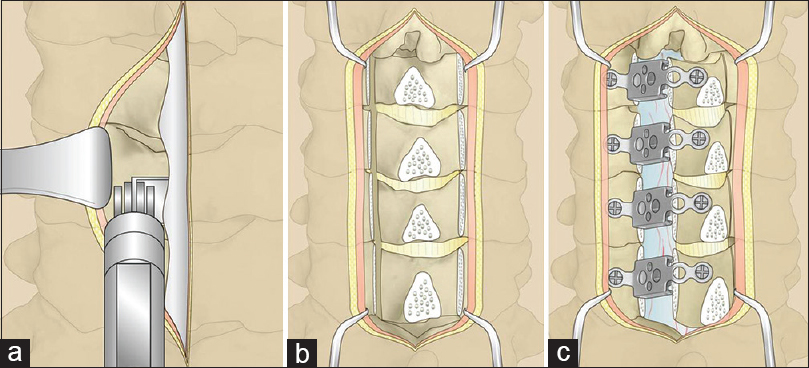
A standard surgical procedure of open-door laminoplasty was performed as follows [Figure
Computed tomography scan analysis
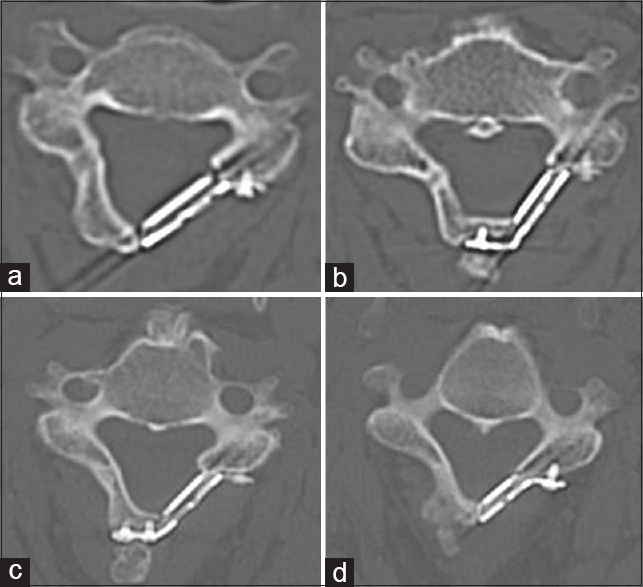
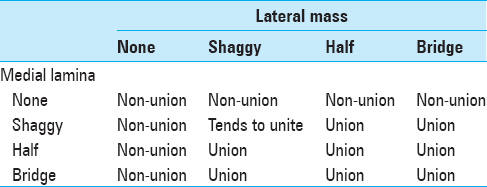
CT scans obtained after surgery were independently evaluated for healing by four different reviewers (all Neurosurgical Spinal Surgeons). Bone union at the open side and closed sides were both evaluated by axial CT images at 12 months after surgery to determine the state of the bone union at the medial and lateral sides of the titanium basket based on our classification [
Figure 2
CT classification of bone fusion at the open side (our classification). (a) none. No visible density between the basket and lamina, and lateral mass. (b) shaggy. Bone density is slightly visible between the basket and lamina, and lateral mass. (c) Half. Bone density is visible in the basket. (d) Bridge. Bone density is continuous from the lateral mass to lamina
RESULTS
Clinical outcome
Open door laminoplasty was safely performed in 27 patients, 92 laminae were elevated. Percentage JOA improvement was 70.5 ± 14.8 (standard deviation); the mean preoperative JOA score was 10.3 ± 2.9, and the mean postoperative score was 14.8 ± 2.1 [
Radiological measurements
Utilizing X-ray and CT studies 12 months postoperatively, bone union occurred on the hinged side 90.2% of the time. Fusion was confirmed on the open side 62.0% of the time; stage 1, 42 baskets; 22.8%, stage 2, 71 baskets: 38.6%, stage 3, 49 baskets: 26.6%, and stage 4, 22 baskets: 12.0%. Circumferential fusion was confirmed 59.8% of the time, whereas the nonunion rate on both sides was 6.5%.
DISCUSSION
The main purpose of the present study was to investigate the radiological union rate at the open side after laminoplasty. The L-Basket titanium plate with a titanium box associated with satisfactory short-term clinical results. In the present study, bone union at the hinge side was observed in 83/92 (90.2%) of 27 patients at 12 months; these data are similar to results published in other studies.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Deutsch H, Mummaneni PV, Rodts GE, Haid RW. Posterior cervical laminoplasty using a new plating system. J Spinal Disord Tech. 2004. 17: 317-20
2. Iguchi T, Kanemura A, Kurihara A, Kasahara K, Yoshida S, Doita M. Cervical laminoplasty: Evaluation of bone bonding of a high porosity hydroxyapatite spacer. J Neurosurg. 2003. 98: 137-142
3. Jin SW, Kim SH, Kim BJ, Choi JI, Ha SK, Kim SD. Modified open-door laminoplasty using hydroxyapatite spacers and miniplates. Korean J Spine. 2014. 11: 188-94
4. Kihara S, Umebayashi T, Hoshimaru M. Technical improvements and results of open-door expansive laminoplasty with hydroxyapatite implants for cervical myelopathy. Neurosurgery. 2005. 57: 348-56
5. Lee S, Chung CK, Kim CH. Risk factor analysis of hinge fusion failure after plate-only open-door laminoplasty. Global Spine J. 2015. 5: 9-16
6. Rhee JM, Register B, Hamasaki T, Franklin B. Plate-only open door laminoplasty maintains stable spinal canal expansion with high rate of hinge union and no plate failures. Spine (Phila Pa 1976). 2011. 36: 9-14
7. Takayasu M, Takagi T, Nishizawa T, Osuka K, Nakajima T, Yoshida J. Bilateral open-door cervical expansive laminoplasty with hydroxyapatite spacers and titanium screws. J Neurosurg (Spine 1). 2002. 96: 22-8
8. Tanaka N, Nakanishi K, Fujimoto Y, Sasaki H, Kamei N, Hamasaki T. Expansive laminoplasty for cervical myelopathy with interconnected porous calcium hydroxyapatite ceramic spacers: Comparison with autogenous bone spacers. J Spinal Disord Tech. 2008. 21: 547-52
9. Tanaka S, Tashiro T, Gomi A, Ujiie H. Cervical unilateral open-door laminoplasty with titanium miniplates through newly designed hydroxyapatite spacers. Neurol Med Chir (Tokyo). 2011. 51: 673-7
10. Tani S, Suetsuna F, Mizuno J, Uchikado H, Nagashima H, Akiyama M. New titanium spacer for cervical laminoplasty: Initial clinical experience. Neurol Med Chir (Tokyo). 2010. 50: 1132-36
11. Tung KL, Cheung P, Kwok TK, Wong KK, Mak KH, Wong WC. Single-door cervical laminoplasty using titanium miniplates alone. J Orthop Surg. 2015. 23: 174-9