- Department of Neurosurgery, Iwate Prefectural Chubu Hospital, Kitakami, Iwate, Japan
Correspondence Address:
Hiroshi Kashimura
Department of Neurosurgery, Iwate Prefectural Chubu Hospital, Kitakami, Iwate, Japan
DOI:10.4103/sni.sni_103_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Kenta Aso, Hiroshi Kashimura, Yoshiyasu Matsumoto, Hiroaki Saura. Microsurgical clipping for anterior communicating artery aneurysm associated with the accessory anterior cerebral artery via the pterional approach. 18-Jun-2018;9:120
How to cite this URL: Kenta Aso, Hiroshi Kashimura, Yoshiyasu Matsumoto, Hiroaki Saura. Microsurgical clipping for anterior communicating artery aneurysm associated with the accessory anterior cerebral artery via the pterional approach. 18-Jun-2018;9:120. Available from: http://surgicalneurologyint.com/surgicalint-articles/microsurgical-clipping-for-anterior-communicating-artery-aneurysm-associated-with-the-accessory-anterior-cerebral-artery-via-the-pterional-approach/
Abstract
Background:Accessory anterior cerebral artery (ACA), a type of median artery of anomalous triplicate ACA, is not rare, but aneurysms of the anterior communicating artery (ACoA) associated with accessory ACA can be a considerable challenge to treat surgically based on the morphological features of the ACoA complex.
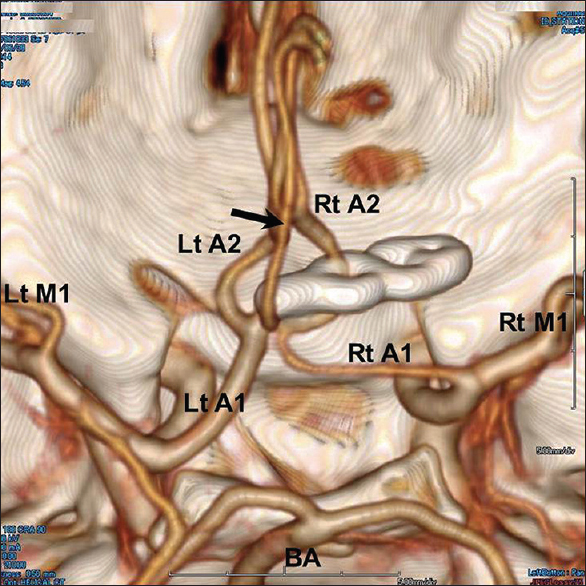
Case Description:A 35-year-old man was admitted to our hospital with severe headache and subsequent loss of consciousness. Initial computed tomography (CT) showed typical findings of subarachnoid hemorrhage in the basal cistern and three-dimensional CT angiography revealed an ACoA aneurysm arising from the trifurcation of the accessory ACA, the branching point of the ACoA, and the right A1 or A2 segment of the ACA. The aneurysmal fundus projected superolaterally to the right, and was treated via a right-sided pterional approach. The aneurysm was behind the ipsilateral A2 segment of the ACA and the accessory ACA was hidden behind the aneurysm. The aneurysm was successfully obliterated with clipping using a straight fenestrated Yasargil titanium clip. Complete aneurysm occlusion and patency of both the A2 segment of the ACA and the accessory ACA were confirmed intraoperatively by indocyanine green angiography.
Conclusion:In treating this aneurysm via the pterional approach, selection of approach side it is critical to preserve prevent the patency of the accessory ACA and to simultaneously perform aneurysm clipping without leaving a neck remnant. Selecting the optimal approach based on preoperative neuroimaging of which side will allow both these actions is important.
Keywords: Accessory anterior cerebral artery, aneurysm, anterior communicating artery, vascular anomaly
INTRODUCTION
The anatomy of the anterior cerebral artery (ACA) is highly variable.[
CASE DESCRIPTION
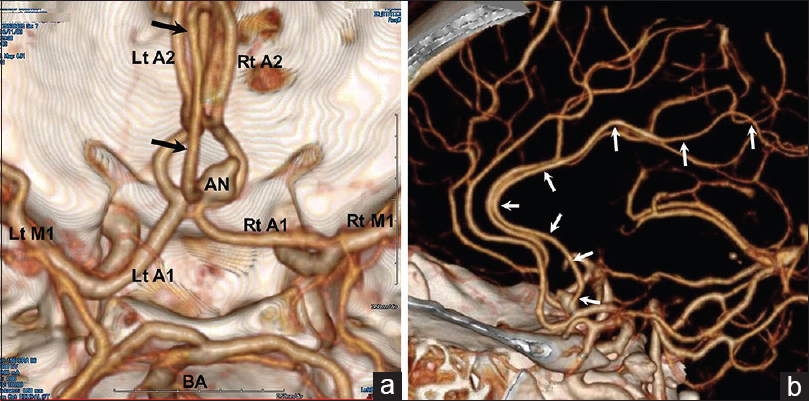
A 35-year-old man presented with severe headache and subsequent loss of consciousness and was admitted to our hospital. No focal neurological abnormalities were noted. Initial computed tomography (CT) showed findings typical of subarachnoid hemorrhage in the basal cistern. Three-dimensional CT angiography revealed an anomalous artery originating from the posterior surface of the ACoA and a saccular aneurysm arising from the trifurcation of the anomalous artery, the branching point of the ACoA with fenestration, and the right A1or A2 segment of the ACA [
Figure 1
(a) Preoperative three-dimensional CT angiogram, superoinferior view, showing a saccular aneurysm (AN) arising from the trifurcation of the accessory ACA (black arrows), the branching point of the ACoA with fenestration, and the right A1 or A2 segment of the ACA. Aneurysmal fundus projects superolaterally to the right. Lt: left; Rt: right; BA: basilar artery. (b) Left lateral view of the three-dimensional CT angiogram, showing the accessory ACA (white arrows) arising from the posterior surface of the ACoA and running around the genu of the corpus callosum, parallel to bilateral pericallosal arteries, which distributed branches to the medial frontal lobes
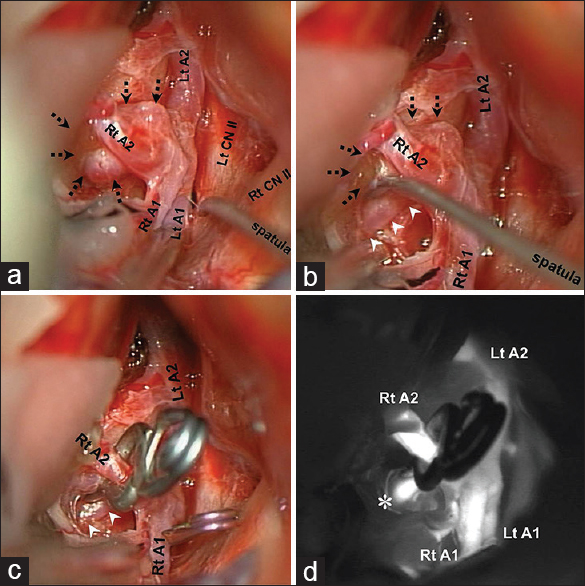
Right frontotemporal craniotomy was performed. Following dissection of the Sylvian fissure and interhemispheric fissure, the ACoA complex including bilateral A1 and A2 segments of the ACA, and the anterior surface of the ACoA were exposed [
Figure 2
Intraoperative photographs showing the aneurysm (dotted arrows) and its relationship to bilateral A1 and A2 segments of the anterior cerebral artery (ACA), and the accessory ACA. (a) Partial resection of the ipsilateral gyrus rectus, allowing visualization of the aneurysm fundus behind the ipsilateral A2 segment of the ACA. (b) Gently pushing the aneurysm (dotted arrows) forward using the spatula to the corner of the ACoA, allowing visualization of the accessory ACA, working between the right frontal lobe and right A2 segment of the ACA. (c) The aneurysm is occluded by a straight fenestrated clip placed with the aperture around the ipsilateral A2 segment of the ACA, preserving the accessory ACA (white arrowheads). (d) Intraoperative indocyanine green angiogram showing patency of both the right A2 segment of the ACA and the accessory ACA (*), and disappearance of the aneurysm. Lt: left; Rt: right; CN: cranial nerve; Lt CN: left cranial nerve
The postoperative course was uneventful, and the patient was discharged with no neurological deficits.
DISCUSSION
The presence of the accessory ACA is well described, but several terms have been used to describe this variation, including medial ACA, median artery of the corpus callosum (MACC), third A2, triple A2, and superior pericallosal artery.[
The two basic surgical approaches used for aneurysm of the ACoA are the interhemispheric approach and the pterional approach. We use a pterional approach for the ACoA aneurysm, except for giant, thrombosed, or extremely high-positioned ACoA aneurysms. Our criteria in selecting the side of the pterional approach are as follows: inferiorly projecting aneurysms are treated from the dominant A1 side to avoid hazardous bleeding, whereas superiorly projecting aneurysms are treated from the side of aneurysm fundus projection for easy dissection of the neck.[
When possible, placement of a straight or angled nonfenestrated clip across the aneurysm neck under direct visual observation remains the safest, simplest method of surgical aneurysm ligation. However, due to variations in the direction of ACoA aneurysms and the regional microvasculature, placement of a straight clip may be impeded by structures traversing the operative trajectory. Zada et al. reported that fenestrated clips were helpful in such situations and were used in 20 of 199 patients who underwent surgical treatment of ACoA aneurysms.[
In treating this an eurysm via a pterional approach, simultaneously preserving preventing patency of the accessory ACA and achieving aneurysm clipping without a neck remnant is critical. Thus, selecting the optimal approach side to achieve both these actions based on preoperative neuroimaging is important. If these actions are expected to be difficult via a pterional approach, even with use of a fenestrated clip, an interhemispheric approach or coil embolization should be considered. Ogawa et al. reported 27 patients with ACoA aneurysms associated with accessory ACA who underwent microsurgical clipping via the bifrontal interhemispheric approach. This approach offers the advantage of allowing a wide operative field and attainment of a good understanding of the vascular structures near the ACoA. It is particularly useful in cases of vascular anomaly in this region.
Recognizing and reporting this variant could be helpful in preventing complications of surgery. Although injury to the accessory ACA itself is unlikely to result in clinical deficits, precise knowledge of the vascular anatomy, including such variants, is essential to help minimize the risk of complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alpers BJ, Berry RG, Paddison RM. Anatomical studies of the circle of Willis in normal brain. AMA Arch Neurol. 1959. 81: 409-18
2. Baptista AG. Studies on the arteries of the brain. II. The anterior cerebral artery: Some anatomic features and their clinical implications. Neurology. 1963. 13: 825-35
3. Gibbons K, Hopkins LN, Heros RC. Occlusion of an “accessory” distal anterior cerebral artery during treatment of anterior communicating artery aneurysms. Report of two cases. J Neurosurg. 1991. 74: 133-5
4. Gomes FB, Dujovny M, Umansky F, Berman SK, Diaz FG, Ausman JI. Microanatomy of anterior cerebral artery. Surg Neurol. 1986. 26: 129-41
5. Kwak R, Niizuma H, Hatanaka M, Suzuki J. Anterior communicating artery aneurysms with associated anomalies. J Neurosurg. 1980. 52: 162-4
6. Ogawa A, Suzuki M, Sakurai Y, Yoshimoto T. Vascular anomalies associated with aneurysms of the anterior communicating artery: Microsurgical observations. J Neurosurg. 1990. 72: 706-9
7. Suzuki M, Fujisawa H, Ishihara H, Yoneda H, Kato S, Ogawa A. Side selection of pterional approach for anterior communicating artery aneurysms – surgical anatomy and strategy. Acta Neurochir (Wien). 2008. 150: 31-9
8. Yasargil MG, Yasargil MG.editors. Anterior cerebral artery complex. Microneurosurgery. Stuttgart: Georg Thieme Verlag; 1984. I: 92-128
9. Zada G, Christian E, Liu CY, Giannotta SL. Fenestrated aneurysm clips in the surgical management of anterior communicating artery aneurysms: Operative techniques and strategy. Neurosurg Focus. 2009. 26: E7-