- Department of Surgery, Section of Neurosurgery, The Aga Khan University Hospital, Karachi, Pakistan
Correspondence Address:
Muhammad S. Shamim
Department of Surgery, Section of Neurosurgery, The Aga Khan University Hospital, Karachi, Pakistan
DOI:10.4103/sni.sni_478_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Muhammad Waqas, Hussain Shallwani, Muhammad S. Shamim, Khabir Ahmad. Perioperative steroids for lumbar disc surgery: A meta-analysis of randomized controlled trials. 05-Apr-2017;8:42
How to cite this URL: Muhammad Waqas, Hussain Shallwani, Muhammad S. Shamim, Khabir Ahmad. Perioperative steroids for lumbar disc surgery: A meta-analysis of randomized controlled trials. 05-Apr-2017;8:42. Available from: http://surgicalneurologyint.com/surgicalint-articles/perioperative-steroids-for-lumbar-disc-surgery-a-meta%e2%80%91analysis-of-randomized-controlled-trials/
Abstract
Background:Our review question was “Does perioperative steroids administration, in comparison with other treatments or placebo, improve either postoperative pain control, length of hospital stay, or return to work in patients undergoing lumbar disc surgery?”
Methods:We searched PubMed, CINAHL PLUS, and Cochrane databases for randomized control trials (RCTs) studying the role of steroids for lumbar disc surgery. Studies that compared perioperative steroids with other treatments or placebo were included. Study outcomes included postoperative back pain, leg pain, length of hospital stay, and return to work. Data was extracted through a proforma. Means and mean differences were calculated for continuous data, whereas odds ratios were calculated for dichotomous data. Data were analyzed with the help of Rev Man 5.
Results:Twenty RCTs were included in the review. Quantitative analysis could be performed on 19 RCTs. Intraoperative steroids improve control of back pain at 24–48 hours. Although there was some benefit of steroid administration in controlling postoperative leg pain, it disappeared at 1 year and in the overall pooled analysis. The length of hospital stay was much shorter in the steroid group. The frequency of adverse events and complications also favored steroid administration.
Conclusion:Intraoperative epidural steroid administration offers some benefit in pain control with a significant reduction in the length of hospital stay. However, there is insufficient evidence to support the routine use of oral and intravenous steroids in the perioperative period.
Keywords: Lumbar surgery, lumbar surgery outcomes, microdiscectomy, perioperative steroids, randomized control trials
INTRODUCTION
The incidence of lumbosacral radiculopathy is estimated to be approximately 3–5%, and therefore, lumbar disc surgery is one of the most common procedures performed by spine surgeons in United States[
MATERIALS AND METHODS
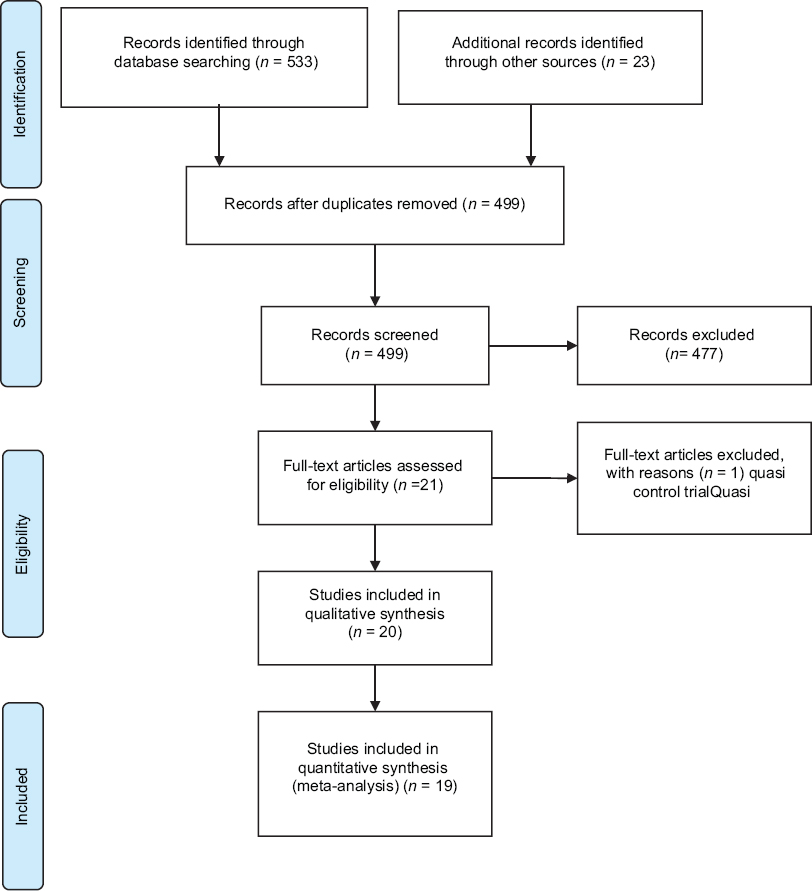
The study included an analysis of RCT studies for adult patients undergoing surgery for lumbar disc herniation who received preoperative, intraoperative, or postoperative steroids, administered through any route, i.e., oral, intravenous, or epidural. We searched PubMed, CINAHL PLUS, and Cochrane databases for randomized control trials (RCTs) studying the role of steroids for lumbar disc surgery. A detailed search strategy is given in
Data extraction
Two reviewers separately and independently extracted the data, which was then recorded in Microsoft Excel. In cases where desired data was not reported by authors, the corresponding authors were contacted for more details or missing data.
Risk of bias assessment
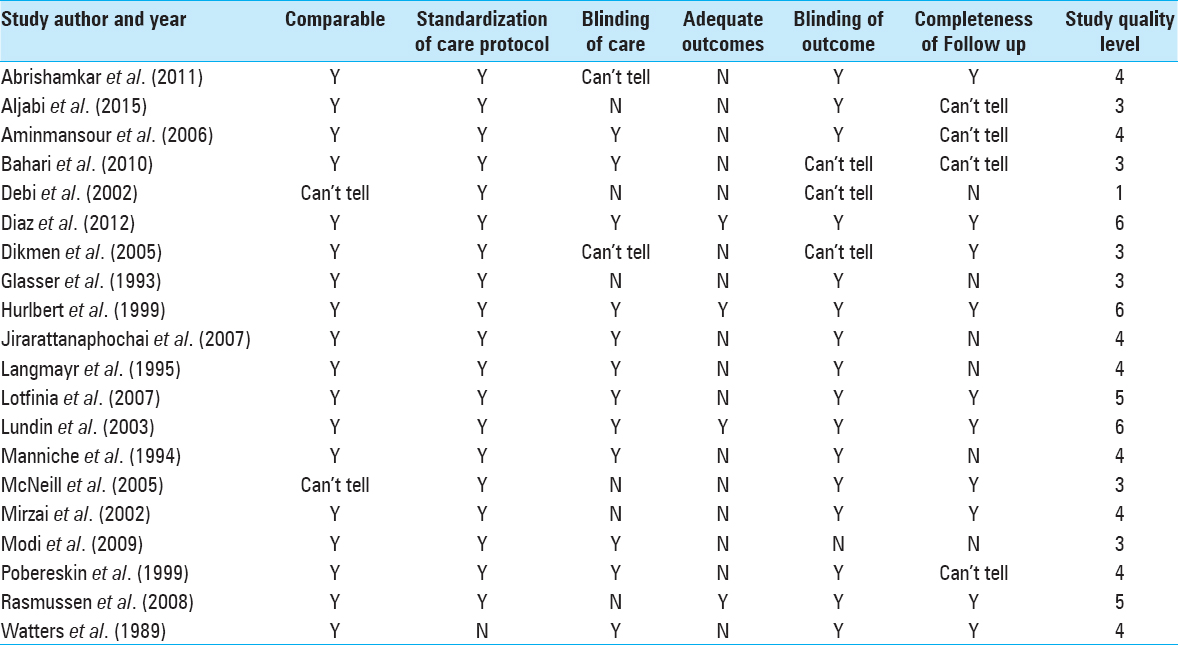
Risk of bias was assessed for each of the selected RCT on six quality parameters, i.e., comparability of treatment groups, standardization of care protocol, blinding of care, adequacy of outcomes, blinding of outcomes, and completeness of follow-up. Each parameter was given a score of 1-point if it was adequately described in the article. No score was given for absence of quality parameter or inadequate description of the same. Study quality level was obtained by adding the scores of each parameter to grade the studies from a total of 6 points.
RESULTS
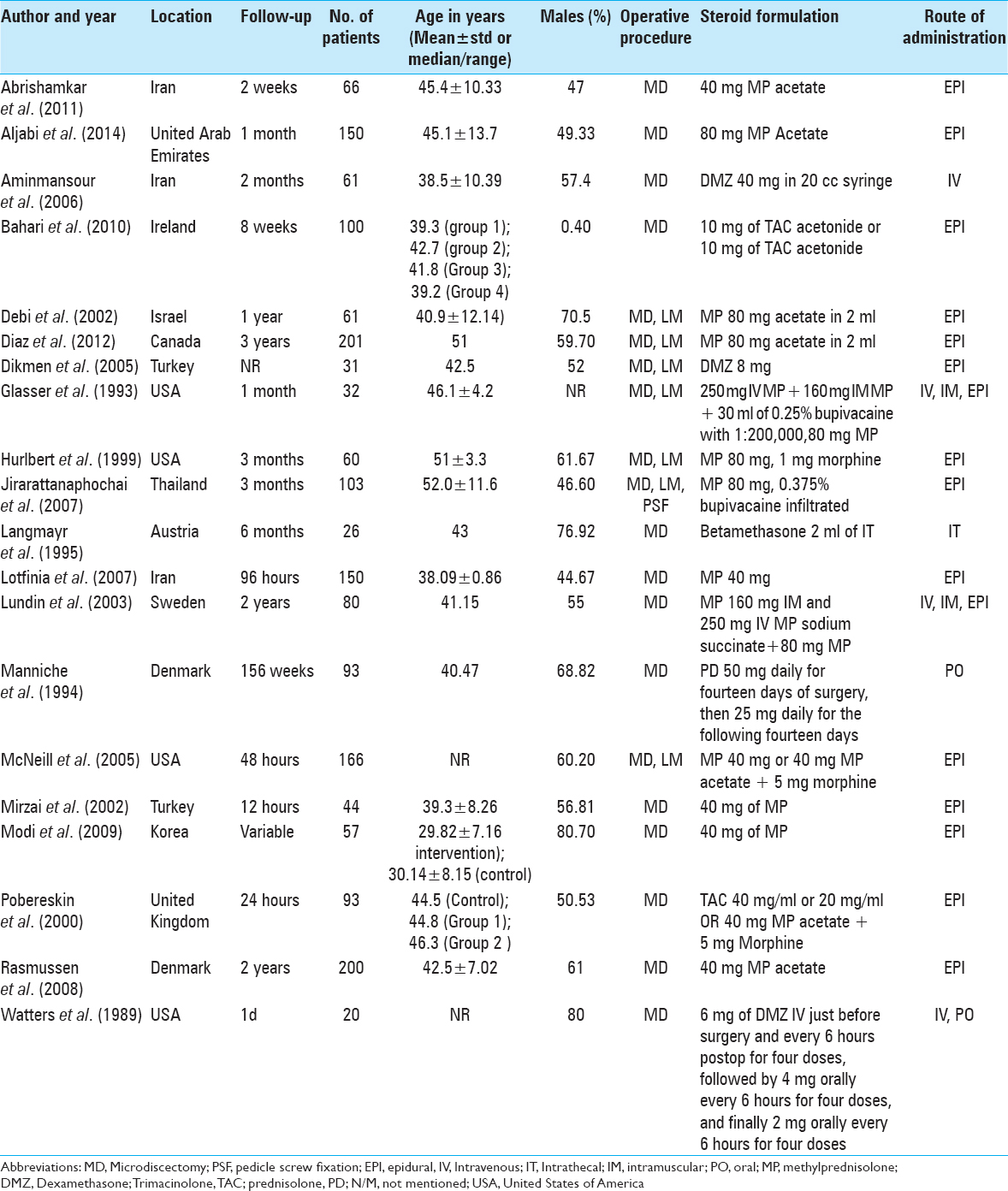
Twenty RCTs were included in this systematic review, and quantitative analysis was performed on 19 studies [
Two RCTs by Ludin et al.[
Postoperative back pain
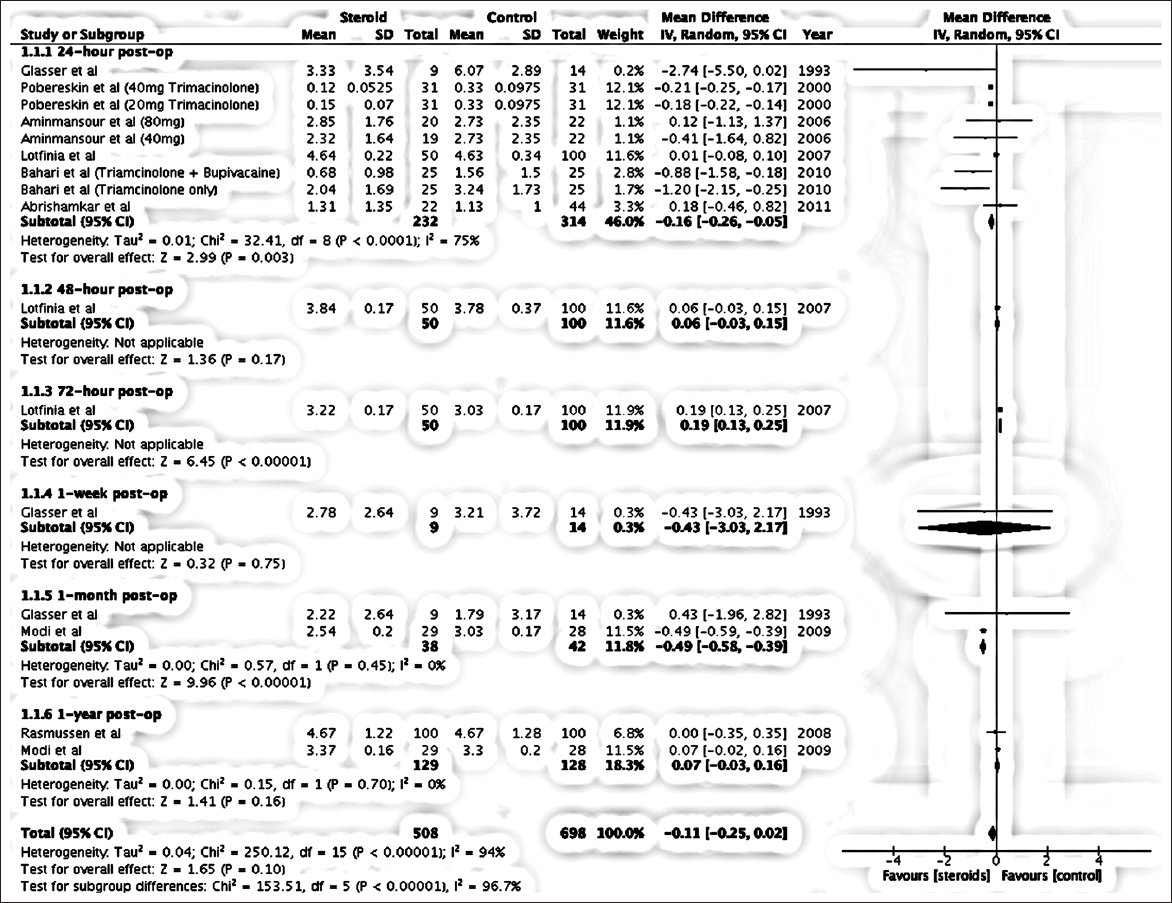
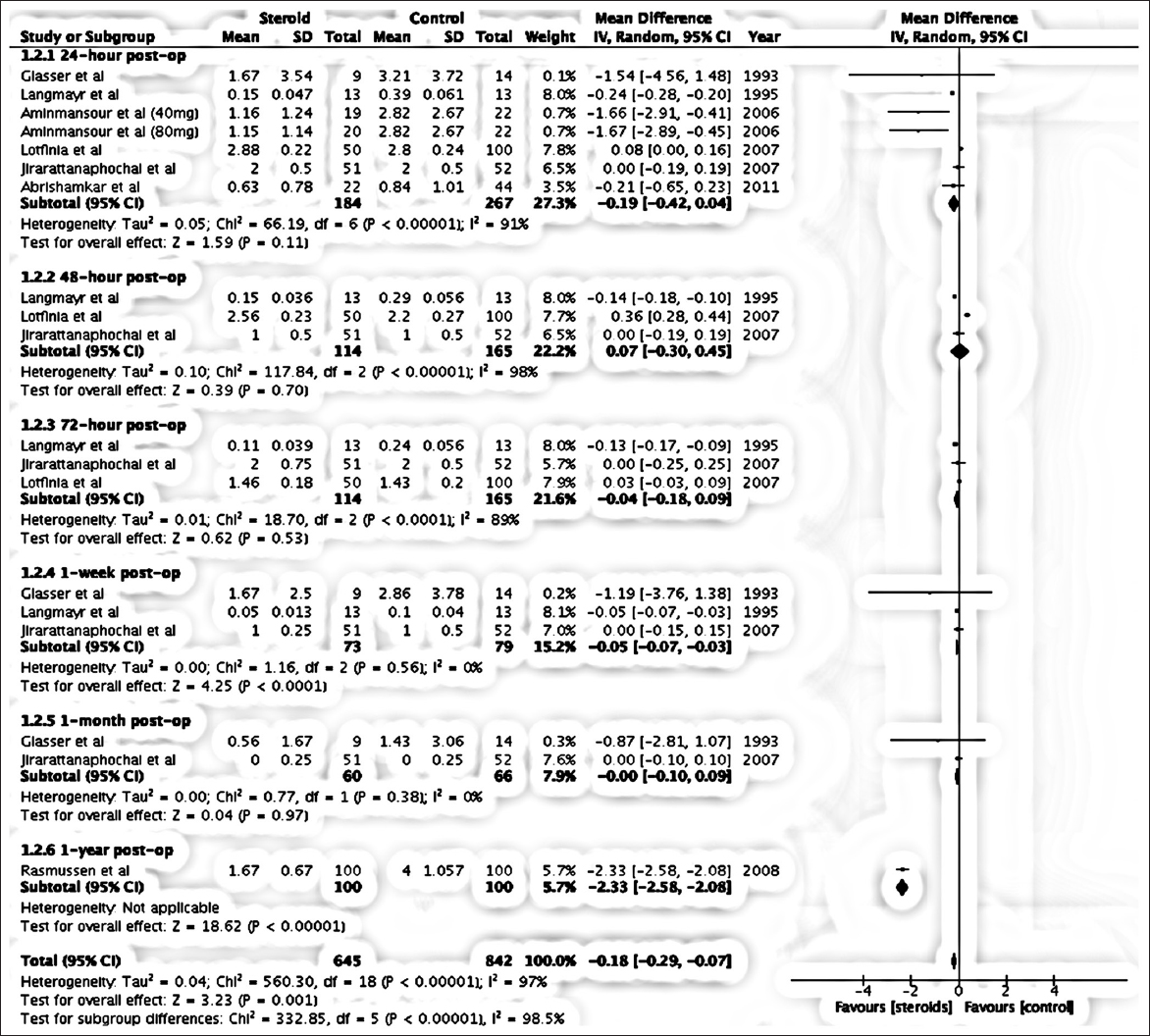
Six studies assessed postoperative back pain at 24 hours. The analysis favored the use of steroids, with a mean difference of −0.16 [95% confidence interval (CI) = −0.26, −0.05]. This difference was statistically significant with a P value of 0.003 [
Postoperative leg pain
The overall analysis favored the use of epidural steroids for reduction of leg pain. The analysis showed significant pain reduction with epidural steroids at 1 week and 1 year. The overall effect favored steroid group with mean difference of −0.18 (−0.29, −0.07). Test for effect Z was 3.32 (P value = 0.001).
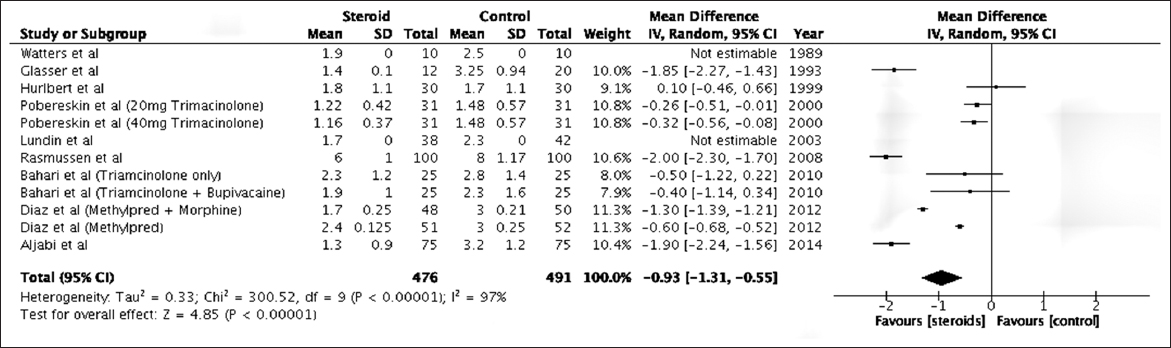
Length of hospital stay
The overall mean difference on LOS favored steroid group with a value of –0.93 (−1.31, −0.55), with a P value of 0.00001.
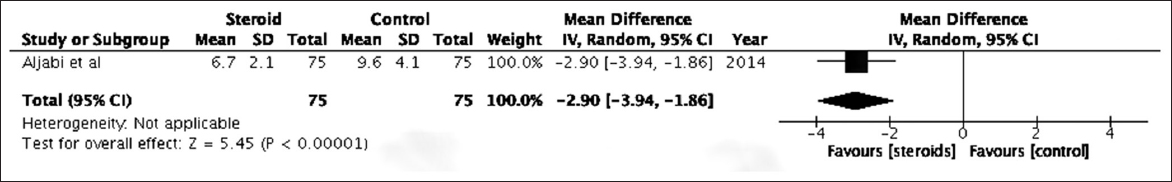
Return to work
The mean number of days for return to work favored the steroid group with a mean difference of –2.90 (95% CI − 3.94, −1.86).
Adverse events
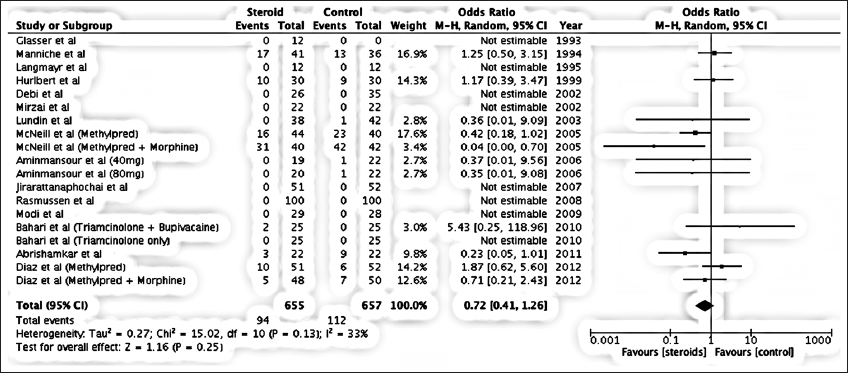
Fifteen RCTs reported AEs and an odds ratio of 0.71 (95% CI: 0.41, 1.26) favored steroid group [
DISCUSSION
Perioperative steroids better control back and leg pain. The administration of perioperative steroids resulted in improved postoperative back pain and postoperative leg pain. The overall mean difference in postoperative back pain between the two groups was small and not statistically significant, i.e., –0.11 (CI − 0.25, 0.02), with a P value of 0.1. RCTs by Pobereskin et al.,[
Analysis favored the steroid group for better postoperative leg pain control at 1 week and 1 year postoperatively [
RCT by Aminmansour et al.[
Perioperative steroids reduce length of stay
Patients receiving perioperative steroids exhibited shorter LOS. Eight of the nine RCTs included in analysis showed shorter hospital stay in steroid group with mean difference of −0.93 (−1.31, −0.55) [
Perioperative steroids reduced time to return to work
Only one RCT by Aljabi et al.[
Quality of randomized controlled trials
The quality of RCTs was assessed using a standardized 6-point scale specifically designed for systematic reviews. Only three RCTs conducted by investigators Diaz,[
Previous systematic reviews on the topic had several limitations. The review by Ranguis et al. in 2010 missed several key trials[
CONCLUSION
Intraoperative epidural steroid administration offers some benefit in pain control with a significant reduction in LOS. However, there is insufficient evidence to support the routine use of oral and intravenous steroids in the perioperative period.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akinduro OO, Miller BA, Haussen DC, Pradilla G, Ahmad FU. Complications of intraoperative epidural steroid use in lumbar discectomy: A systematic review and meta-analysis. Neurosurg Focus. 2015. 39: E12-
2. Aljabi Y, El-Shawarby A, Cawley DT, Aherne T. Effect of epidural methylprednisolone on post-operative pain and length of hospital stay in patients undergoing lumbar microdiscectomy. Surgeon. 2015. 13: 245-9
3. Aminmansour B, Khalili HA, Ahmadi J, Nourian M. Effect of high-dose intravenous dexamethasone on postlumbar discectomy pain. Spine. 2006. 31: 2415-7
4. Bahari S, El-Dahab M, Cleary M, Sparkes J. Efficacy of triamcinolone acetonide and bupivacaine for pain after lumbar discectomy. Eur Spine J. 2010. 19: 1099-103
5. Debi R, Halperin N, Mirovsky Y. Local application of steroids following lumbar discectomy. J Spinal Disord Tech. 2002. 15: 273-6
6. Diaz RJ, Myles ST, Hurlbert RJ. Evaluation of epidural analgesic paste components in lumbar decompressive surgery: A randomized double-blind controlled trial. Neurosurgery. 2012. 70: 414-24
7. Glasser RS, Knego RS, Delashaw JB, Fessler RG. The perioperative use of corticosteroids and bupivacaine in the management of lumbar disc disease. J Neurosurg. 1993. 78: 383-7
8. Grönblad M, Virri J, Tolonen J, Seitsalo S, Kääpä E, Kankare J. A controlled immunohistochemical study of inflammatory cells in disc herniation tissue. Spine. 1994. 19: 2744-51
9. Hozo S, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Method. 2005. 5: 1-
10. Hurlbert RJ, Theodore N, Drabier JB, Magwood AM, Sonntag VK. A prospective randomized double-blind controlled trial to evaluate the efficacy of an analgesic epidural paste following lumbar decompressive surgery. J Neurosurg Spine. 1999. 90: 191-7
11. Lotfinia I, Khallaghi E, Meshkini A, Shakeri M, Shima M, Safaeian A. Interaoperative use of epidural methylprednisolone or bupivacaine for postsurgical lumbar discectomy pain relief: A randomized, placebo-controlled trial. Ann Saudi Med. 2007. 27: 279-
12. Lundin A, Magnuson A, Axelsson K, Kogler H, Samuelsson L. The effect of perioperative corticosteroids on the outcome of microscopic lumbar disc surgery. Eur Spine J. 2003. 12: 625-30
13. Modi H, Chung KJ, Yoon HS, Yoo HS, Yoo JH. Local application of low-dose Depo-Medrol is effective in reducing immediate postoperative back pain. Int Orthop. 2009. 33: 737-43
14. Pobereskin L, Sneyd J. Does wound irrigation with triamcinolone reduce pain after surgery to the lumbar spine?. Br J Anaesth. 2000. 84: 731-4
15. Ranguis SC, Li D, Webster AC. Perioperative epidural steroids for lumbar spine surgery in degenerative spinal disease: A review. J Neurosurg Spine. 2010. 13: 745-57
16. Rasmussen S, Krum-Møller DS, Lauridsen LR, Jensen SEH, Mandøe H, Gerlif C. Epidural steroid following discectomy for herniated lumbar disc reduces neurological impairment and enhances recovery: A randomized study with two-year follow-up. Spine. 2008. 33: 2028-33
17. Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin. 2007. 25: 387-405
18. Weinstein JN, Lurie JD, Tosteson TD, Tosteson AN, Blood E, Abdu WA. Surgical versus non-operative treatment for lumbar disc herniation: Four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine. 2008. 33: 2789-