- Department of Radiology, The Aga Khan University Hospital, Karachi, Pakistan
- Department of Medicine, The Aga Khan University Hospital, Karachi, Pakistan
- Department of Surgery, The Aga Khan University Hospital, Karachi, Pakistan
- Department of Neurosurgery, The Aga Khan University Hospital, Karachi, Pakistan
Correspondence Address:
Rashid Jooma
Department of Neurosurgery, The Aga Khan University Hospital, Karachi, Pakistan
DOI:10.4103/sni.sni_267_17
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Waseem Mehmood Nizamani, Mubbashira Siddiqui, Sehrish Nizar Ali Momin, Muhammad Waqas, Rashid Jooma. Resolution of symptomatic secondary empty sella syndrome following lumbar–peritoneal shunt. 05-Apr-2018;9:72
How to cite this URL: Waseem Mehmood Nizamani, Mubbashira Siddiqui, Sehrish Nizar Ali Momin, Muhammad Waqas, Rashid Jooma. Resolution of symptomatic secondary empty sella syndrome following lumbar–peritoneal shunt. 05-Apr-2018;9:72. Available from: http://surgicalneurologyint.com/surgicalint-articles/resolution-of-symptomatic-secondary-empty-sella-syndrome-following-lumbar-peritoneal-shunt/
Abstract
Background:Post-surgical empty sella is related to the removal of pituitary tumors either from the transcranial or transphenoidal route, rendering diaphragma sellae incompetent at the end of the procedure. This subsequently leads to herniation of the third ventricle and optic apparatus into the empty sella. Studies have shown that in 50% of the cases, individuals with primary and secondary empty sella syndrome have developed defects in the visual fields. Benign increased intracranial pressure, cerebrospinal rhinorrhea, papilledema, and abnormalities affecting visual acuity may also occur as a result of empty sella.
Case Description:This case report discusses a rare treatment option for the symptomatic secondary empty sella syndrome. Patient underwent lumbar drain placement and that resulted in astonishingly significant improvement in vision. Keeping in view the beneficial effect of lumbar drain, lumbar–peritoneal (LP) shunt was inserted which showed drastic improvement in vision.
Conclusion:The surgical outcome of symptomatic cases of ESS is favorable. Various common surgical options were reported in literature; however, we have discussed an unconventional surgical option with an impressive outcome.
Keywords: Empty sella turcica, optic chiasma, pituitary adenoma, visual fields
INTRODUCTION
Post-surgical empty sella is related to the removal of pituitary tumors either from the transcranial or transphenoidal route, rendering diaphragma sellae incompetent at the end of the procedure.[
CASE REPORT
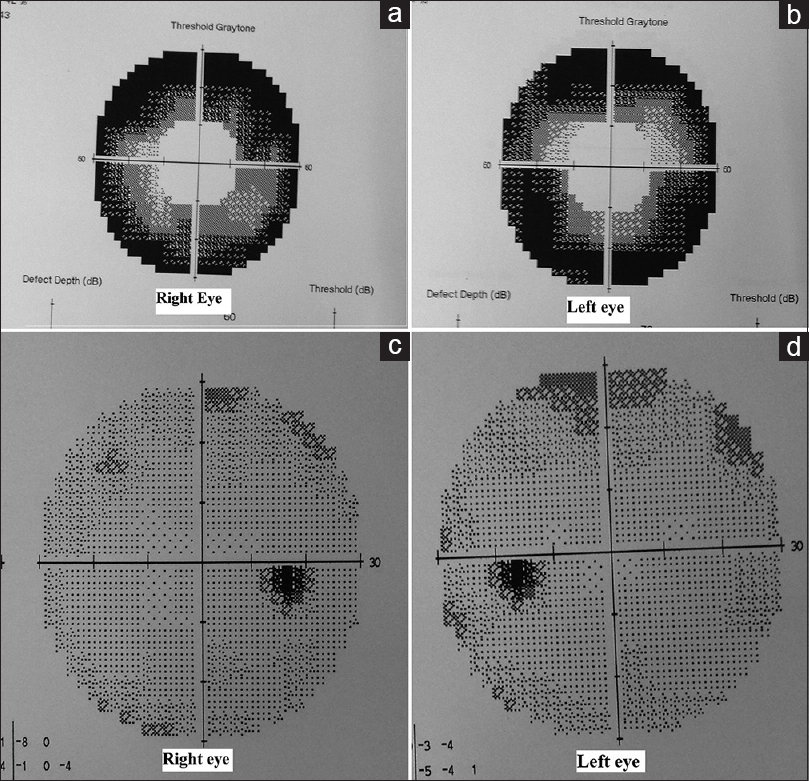
A 51-year-old lady was admitted in Aga Khan University Hospital, Karachi, with complaints of headache and blurring of vision. She was diagnosed as having pituitary macroadenoma [
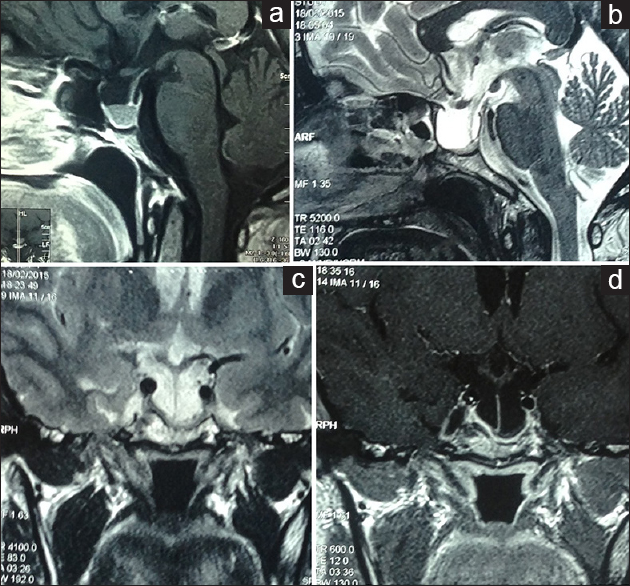
Figure 1
(a) Presurgical contrast enhanced T1 Sagittal MR image of the pituitary gland showing macroadenoma. Post surgical images (b) Sagittal T2 (c) Coronal T2 and (d) Post contrast T1 weighted Coronal images of the pituitary gland showing residual gland and evident empty sella turcica with downward herniation of optic chiasm and suprasellar structures
DISCUSSION
This case report highlights a rare treatment option for the symptomatic secondary empty sella syndrome resulting from post-surgical pituitary resection. Various studies have mentioned ways to prevent downward herniation of optic chiasma that have been resulting in visual defects in subjects. Around 50% of patients show visual field defects associated with both primary and secondary empty sella syndromes.[
Sellar or parasellar surgery Radiation therapy for an intrasellar expansion Bromocriptine therapy for a pituitary adenoma.
Radiation-induced vascular changes or strangulation of the optic nerves or chiasm are thought to compromise local blood flow. Downward herniation of the optic pathways is present in the majority of cases.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Fouad W. Review of empty sella syndrome and its surgical management. Alexandria J Med. 2011. 47: 139-47
2. Guinto G, del Valle R, Nishimura E, Mercado M, Nettel B, Salazar F. Primary empty sella syndrome: The role of visual system herniation. Surg Neurol. 2002. 58: 42-7
3. Kaptain GJ, Vincent DA, Laws ER. Cranial base reconstruction after transsphenoidal surgery with bioabsorbable implants: Technical note. Neurosurgery. 2001. 48: 232-4
4. Seiler RW, Mariani L. Sellar reconstruction with resorbable Vicryl patches, gelatin foam, and fibrin glue in transsphenoidal surgery: A 10-year experience with 376 patients. J Neurosurg. 2000. 93: 762-5
5. Thomé C, Zevgaridis D. Delayed visual deterioration after pituitary surgery-a review introducing the concept of vascular compression of the optic pathways. Acta Neurochir (Wien). 2004. 146: 1131-
6. Cybulski GR, Stone JL, Geremia G, Anson J. Intrasellar balloon inflation for treatment of symptomatic empty sella syndrome. Neurosurgery. 1989. 24: 105-9