- Department of Neurosurgery, Umberto I General Hospital, Università Politecnica delle Marche, Ancona, Italy
Correspondence Address:
M. Dobran
Department of Neurosurgery, Umberto I General Hospital, Università Politecnica delle Marche, Ancona, Italy
DOI:10.4103/sni.sni_222_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: M. Dobran, A. Marini, D. Nasi, M. Gladi, V. Liverotti, M. Della Costanza, F. Mancini, M. Scerrati. Risk factors of surgical site infections in instrumented spine surgery. 06-Sep-2017;8:212
How to cite this URL: M. Dobran, A. Marini, D. Nasi, M. Gladi, V. Liverotti, M. Della Costanza, F. Mancini, M. Scerrati. Risk factors of surgical site infections in instrumented spine surgery. 06-Sep-2017;8:212. Available from: http://surgicalneurologyint.com/surgicalint-articles/risk-factors-of-surgical-site-infections-in-instrumented-spine-surgery/
Abstract
Background:The incidence of wound infections associated with instrumented spine surgery ranges from 2 to 20%. These complications may lead to poor outcomes. Knowing the risk factors associated with surgical site infections (SSI) after utilizing spinal implants is essential to avoid these complications, including hardware removal.
Methods:We reviewed retrospectively 550 patients who underwent spinal fusion surgery from 2011 to 2015; 16 developed SSI after spinal instrumentation. The diagnosis of SSI was established based on positive wound swab or blood cultures, and various clinical, laboratory, and radiological findings. Additional preoperative and intraoperative risk factors were analyzed.
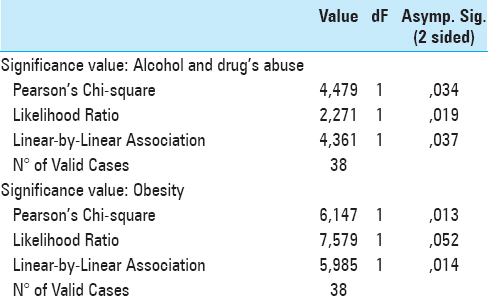
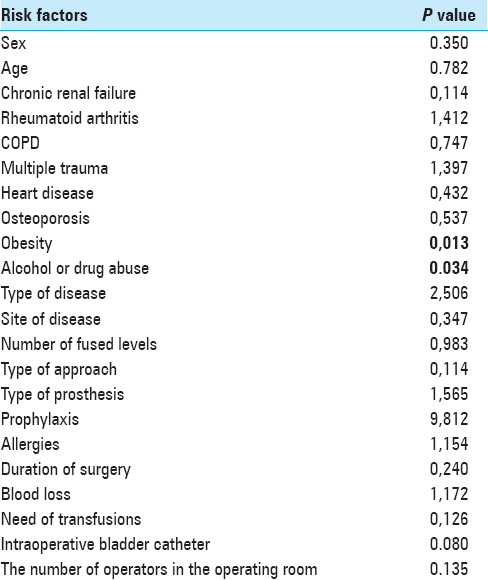
Results:The incidence of SSI after spinal instrumentation surgery was 2.9%. Obesity was a statistically significant parameter (P = 0.013) that contributed to SSI along with the alcoholism and/or drug abuse (P = 0.034); use of a Foley catheter nearly reached significance levels.
Conclusions:There is an increased risk of SSI in patients who are obese or use drugs and/or alcohol. Clear preoperative identification of these risk factors prior to implanting spinal instrumentation should help prevent SSI in the future.
Keywords: Spinal hardware, spinal implants, spinal infections, spine surgery, surgical site infections, risk factors
INTRODUCTION
The incidence of wound infections associated with instrumented spine surgery ranges from 2 to 20%, and typically leads to poor outcomes.[
MATERIALS AND METHODS
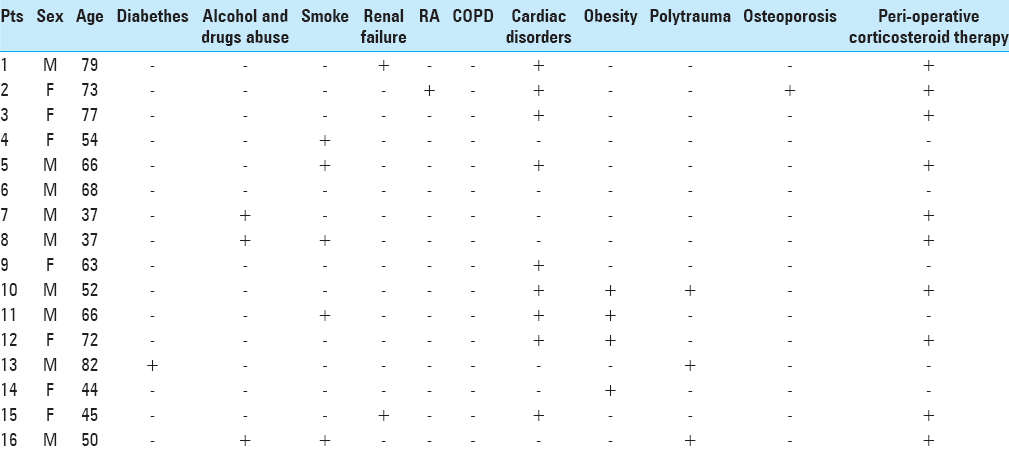
We reviewed retrospectively 550 patients who underwent spinal fusion from 2011 to 2015; there were 16 patients (9 males and 7 females) who developed SSI. They averaged 60.2 years (range 37–82 years) of age.
Wound prophylaxis
All procedures were performed using a standard surgical scrub and 2 g cefazolin sodium was administered 30 minutes before skin incision and then once a day for 48 hours after surgery. Surgical drains are placed and then removed 48 hours postoperatively. The choice of hardware for instrumented fusion was based on spinal pathology and typically included titanium screws/rods or cervical plates.
Assessment/diagnosis of SSI
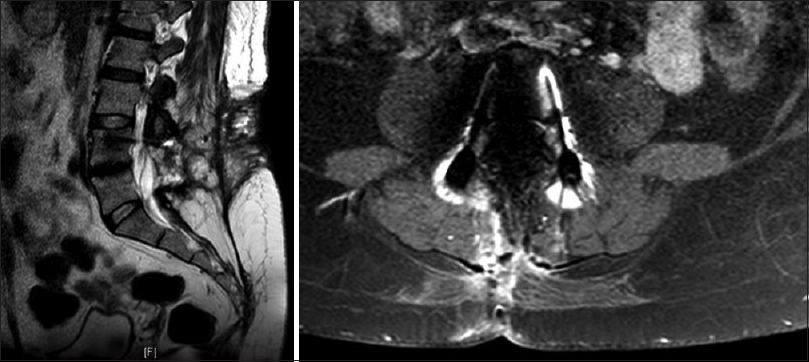
All patients had postoperative laboratory tests and a computed tomography (CT) scan 48–72 hours after surgery. Magnetic resonance imaging (MRI) and inflammatory laboratory tests were made only in patients with suspicion of infection. Diagnostic criteria of SSI included local wound redness, dehiscence, secretions, tenderness to palpation [
Analysis of risk factors for SSI
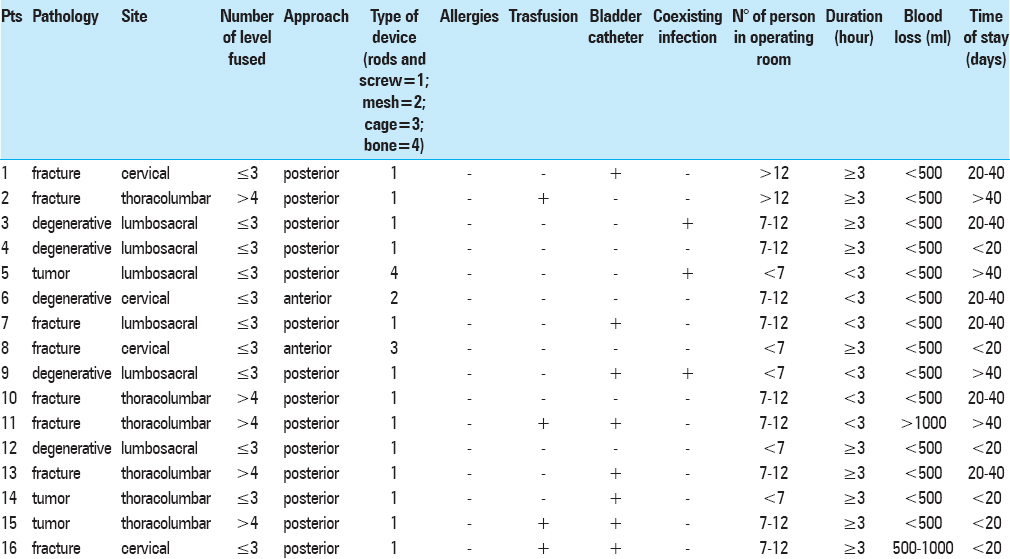
Multiple risk factors for SSI were analyzed in this study including sex, age, smoking status, diabetes mellitus, obesity (BMI >30), chronic renal failure, chronic obstructive pulmonary disease (COPD), rheumatoid arthritis, chronic heart disease, osteoporosis, polytrauma, presence of co-infections at the time of surgery, preoperative corticosteroids intake. Intraoperative factors included type of disease (degenerative spine disease, tumors, pathologic fracture for concomitant osteoporosis, and traumatic fracture), surgical vertebral level (cervical, thoracolumbar, and lumbar or lumbosacral), surgical approach (anterior or posterior), number of fused levels (≤3 or >4), type of implanted prosthesis, perioperative antibiotic prophylaxis, operation time, number of operators present in the operating room, blood loss, need for transfusion, Foley catheter, and length of stay in the postoperative period.
Statistical evaluation
Data were compared with a control group of 16 patients and analyzed by univariate statistical analysis with Chi-square test for the discrete variables. P < 0.05 was considered statistically significant. The software used for data analyses was SPSS (IBM, SPSS Statistics 24, Armonk, NY, Version 20).
RESULTS
The risk factors found to contribute to SSI in our series included obesity (statistically significant parameter with a P value of 0.013), as well as history of alcohol or drug abuse with a P value of 0.034 [Tables
DISCUSSION
SSI after instrumented spinal surgery have an incidence between 0.7% and 12%.[
The abuse of alcohol and drugs causes reduction of liver response to infection diseases, nutritional depletion and increased vulnerability of the immune system to infections.[
We found no statistical correlation of SSI with associated diseases (e.g., chronic renal failure, rheumatoid arthritis, COPD, cardiovascular disease, osteoporosis, and polytrauma). The use of short-term corticosteroid therapy did not significantly increase the risk of SSI, but studies show long treatments, in the course of chronic diseases, as metastases or rheumatoid arthritis, are potential risk factors.[
Finally, we showed that intraoperative risk factors do not contribute to SSI. This included no correlation with the estimated blood loss, transfusion requirements, operative time, or even the use of an intraoperative Foley.
CONCLUSIONS
In this study, significant risk factors contributing to SSI (16/550) included obesity and drug and alcohol abuse. Other risk factors such as the use of Foley catheter and number of people in operating room are less important with P values near statistical significance.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Clark CE, Shufflebarger HL. Late -developing infection in instrumented idiopathic scoliosis. Spine (Philadelphia 1976). 1999. 24: 1909-12
2. Dan X, Jian-Xiong M, Xin-Long M, Dong-Hui S, Jie W, Yang C. A methodological, systematic review of evidence-based independent risk factors for surgical site infections after spinal surgery. Eur Spine J. 2013. 22: 605-15
3. Dobran M, Iacoangeli M, Di Somma LGM, Di Rienzo A, Colasanti R, Nocchi N. Neurological outcome in a series of 58 patients operated for traumatic thoracolumbar spinal cord injuries. Surg Neurol Int. 2014. 5: S329-32
4. Dobran M, Nasi D, Brunozzi D, Di Somma L, Gladi M, Iacoangeli M. Treatment of unstable thoracolumbar junction burst fractures: Short-segment pedicle fixation with inclusion of fracture level versus long-term instrumentation. Acta Neurochir (Wien). 2016. 158: 1883-9
5. Dobran M, Iacoangeli M, Nasi D, Nocchi N, Di Rienzo A, di Somma L. Posterior titanium screw fixation without debridement of infected tissue for the treatment of thoracolumbar spontaneous pyogenic spondylodiscitis. Asian Spine J. 2016. 10: 465-71
6. Kadota Y, Nishida K, Hashizume K, Nasu Y, Nakahara R, Kanazawa T. Risk factors for surgical site infection and delayed wound healing after orthopedic surgery in rheumatoid arthritis patients. Mod Rheumatol. 2016. 26: 68-74
7. Manish K, Kasliwal , Lee A, Traynelis VC. Infection with spinal instrumentation: Review of pathogenesis, diagnosis, prevention and management. Surg Neurol Int. 2013. 4: 392-403
8. Marou K, Berven Sh. Outcome and treatment of postoperative spine surgical site infections: Predictors of treatment success and failure. J Orthop Sci. 2014. 19: 398-404
9. Quile A. Infection associated with spinal implants. Int Orthop (sicot). 2012. 36: 451-6
10. Salsgiver E, Crotty J, LaRussa SJ, Bainton NM, Matsumoto H, Demmer RT. Surgical Site Infections following Spine Surgery for Non-idiopathic Scoliosis. J Pediatr Orthop. 2016. p.