- Professor of Clinical Neurosurgery, School of Medicine, State University of New York at Stony Brook, New York, and Chief of Neurosurgical Spine and Education, NYU Winthrop Hospital, NYU Winthrop NeuroScience/Neurosurgery, Mineola, New York 11501, United States
Correspondence Address:
Nancy E. Epstein
Professor of Clinical Neurosurgery, School of Medicine, State University of New York at Stony Brook, New York, and Chief of Neurosurgical Spine and Education, NYU Winthrop Hospital, NYU Winthrop NeuroScience/Neurosurgery, Mineola, New York 11501, United States
DOI:10.25259/SNI-123-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. A Comparison of Kyphoplasty, Vertebroplasty, or Non-Surgical Treatment of Traumatic/Atraumatic Osteoporotic Vertebral Compression Fractures: A Short Review. 24-Apr-2019;10:54
How to cite this URL: Nancy E. Epstein. A Comparison of Kyphoplasty, Vertebroplasty, or Non-Surgical Treatment of Traumatic/Atraumatic Osteoporotic Vertebral Compression Fractures: A Short Review. 24-Apr-2019;10:54. Available from: http://surgicalneurologyint.com/surgicalint-articles/9300/
Abstract
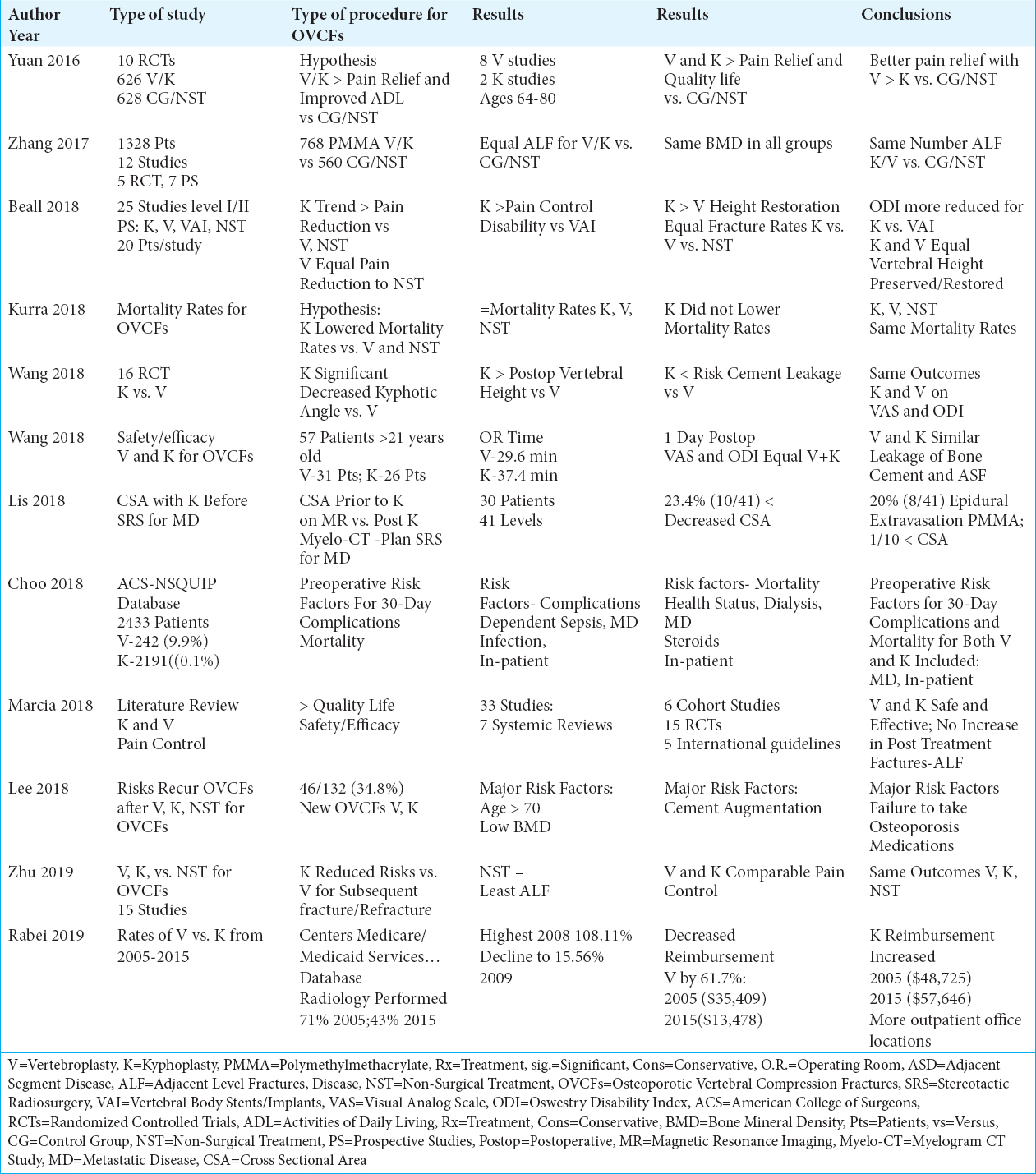
Background:Although the majority of patients with traumatic/atraumatic osteoporotic vertebral compression fractures (OVCFs) may be managed with non-surgical treatment (NST), a subset (e.g. 40%) with significant pain, loss of vertebral height, and other factors may warrant percutaneous vertebroplasty (V), or percutaneous kyphoplasty (K).
Methods:We compared the impact of these three treatment modalities, V, K, or NST, for managing OVCFs.
Results:In several studies, both V and K resulted in comparable improvement in pain relief, postoperative kyphotic angles, increased anterior vertebral heights, and frequency of leakage of bone cement. One study evaluating 16 RCT’s (Randomized Controlled Studies), however, observed K significantly; “decreased the kyphotic wedge angle, increased the postoperative vertebral body height, and decreased the risk of cement leakage vs. V”. Further, in some series, both V and K resulted in higher quality of life scores and better pain relief vs. NST, while other studies showed V was superior to K. Further, although the risk of adjacent level fractures (ALF) following V, K, and NST were comparable in most studies, one clearly demonstrated NST had the lowest incidence of ALF. Despite all these findings, most studies concluded outcomes were comparable for all 3 groups.
Conclusions:Although most OVCFs are still managed with non-surgical treatment (NST), a subset (e.g. about 40%) may warrant V or K. Although both V and K have been shown to result in significantly better pain relief, higher quality of life scores, increased postoperative vertebral body height compared with NST, outcomes for all 3 groups remained the same.
Keywords: Kyphoplasty, vertebroplasty, conservative management, osteoporotic, compression fractures, optimal treatment
INTRODUCTION
Traumatic/atraumatic osteoporotic vertebral compression fractures (OVCFs) attributed to osteoporosis cost the US health care industry over $1 billion dollars/year. Although the majority of OVCFs may be managed with non-surgical treatment (NST), a subset (e.g. 40%) with significant loss of vertebral height, pain, and other factors may warrant percutaneous kyphoplasty (K) or percutaneous vertebroplasty (V).[
Frequency of Traumatic Osteoporotic Vertebral Compression Fractures (OVCFs)
Goldstein et al. in 2015 observed that vertebral compression fractures (VCFs) most commonly were attributed to osteoporosis [
Different Conclusions Regarding the Impact of V vs. K on Kyphotic Angles, Vertebral Body Heights and Risks of Cement Leakage
Two 2018 studies came to different conclusions regarding the relative impact of V vs. K on post-procedural; kyphotic angles, vertebral body heights, and risks of cement leakage. Wang et al. in 2018 radiographically evaluated the outcomes for 57 patients over a 2-year period undergoing V (31 patients) vs. K (26 patients) for OVCFs [
Similar Risks of Adjacent Level Fractures (ALF) After V, K, and NST With One Exception
Multiple studies looked at whether V, K, or NST correlated with higher rates of adjacent level fractures (ALF). In a meta-analysis in 2017, Zhang et al. identified 12 studies (5 randomized clinical trials (RCT); 7 prospective studies) that involved 1,328 patients; 768 underwent V/K with PMMA (polymethylmethacrylate) vs. 560 treated non-surgically (NST) [
Similar or Better Pain Relief with V vs. K, With Both Typically Superior to NST
Several studies showed similar or better pain relief with V or K, with both procedures proving superior to NST [
Shift from V to K for Treating OVCFs in the Medicare Population (2005-2015) Reflected Changes in Reimbursement
Utilizing the Centers for Medicare and Medicaid Services annual Medicare Physician Supplier Procedure Summary database, Rabei et al. (2019) retrospectively evaluated Medicare data (2005-2015) regarding the impact of decreased reimbursement rates for V and increased reimbursement for K for OVCFs [
Thecal Sac Area After K for Pathological/Metastatic OVCFs Prior to Stereotactic Radiosurgery (SRS)
Lis et al. In 2018 assessed changes in the cross-sectional thecal sac volume after K but prior to single-fraction stereotactic radiosurgery for symptomatic vertebral compression fractures due to metastatic disease [
Relatively Low Complication Rates for V and K to Treat OVCFs
Marcia et al. in 2018 identified 33 patients undergoing V and K from 7 systematic reviews, 6 cohort studies, 15 randomized clinical trials, and 5 international guidelines; based upon this review, they concluded these procedures were safe, with relatively low complication rates [
30-Day Complication, and Mortality Rates for V/K
Utilizing the 2012-2014 ACS-NSQIP (American College of Surgeons – National Surgical Quality Improvement Program) database of 2433 patients, Choo et al. in 2018 looked at the frequency of 30-day complications, readmissions, and mortality rates following V 242(9.9%) vs. K 2191(90.1%) [
Risk for Recurrent OVCFs
In a retrospective study, Lee et al. in 2018 evaluated the risk factors for patients likely to develop recurrent OVCFs after V and K vs. NST [
CONCLUSIONS
Although the majority of OVCFs are managed with non-surgical treatment (NST), up to 40% with persistent pain and other complaints/symptoms/signs may warrant vertebroplasty (V) or kyphoplasty (K). Both V and K have been shown, in most studies, to result in significantly better pain relief, higher quality of life scores, and increased postoperative vertebral body height when compared with NST. A subset of series demonstrated the superiority of K over V or V over K compared with NST. Nonetheless, most studies documented comparable long-term outcomes utilizing all 3 treatment modalities (V, K, and NST).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Beall D, Lorio MP, Yun BM, Runa MJ, Ong KL, Warner CB. Review of Vertebral Augmentation:An Updated Meta-analysis of the Effectiveness. Int J Spine Surg. 2018. 12: 295-321
2. Choo S, Malik AT, Jain N, Yu E, Kim J, Khan SN. 30-day adverse outcomes, re-admissions and mortality following vertebroplasty/kyphoplasty. Clin Neurol Neurosurg. 2018. 174: 129-133
3. Goldstein CL, Chutkan NB, Choma TJ, Orr RD. Management of the Elderly With Vertebral Compression Fractures. Neurosurgery. 2015. 77: S33-45
4. Kurra S, Metkar U, Lieberman IH, Lavelle WF. The Effect of Kyphoplasty on Mortality in Symptomatic Vertebral Compression Fractures:A Review. Int J Spine Surg. 2018. 12: 543-548
5. Lee BG, Choi JH, Kim DY, Choi WR, Lee SG, Kang CN. Risk factors for newly developed osteoporotic vertebral compression fractures following treatment for osteoporotic vertebral compression fractures. Spine J. 2018. p. ii:S1529-
6. Lis E, Laufer I, Barzilai O, Yamada Y, Karimi S, McLaughlin L. Change in the cross-sectional area of the thecal sac following balloon kyphoplasty for pathological vertebral compression fractures prior to spine stereotactic radiosurgery. J Neurosurg Spine. 2018. p. 1-8
7. Marcia S, Muto M, Hirsch JA, Chandra RV, Carter N, Crivelli P. What is the role of vertebral augmentation for osteoporotic fractures?A review of the recent literature. Neuroradiology. 2018. 60: 777-783
8. Rabei R, Patel K, Ginsburg M, Patel MV, Turba UC, Arslan B. Percutaneous Vertebral Augmentation for Vertebral Compression Fractures:National Trends in the Medicare Population (2005-2015). Spine (Phila Pa 1976). 2019 J. 44: 123-133
9. Wang B, Zhao CP, Song LX, Zhu L. Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture:a meta-analysis and systematic review. J Orthop Surg Res. 2018. 13: 264-
10. Wang F, Wang LF, Miao DC, Dong Z, Shen Y. Which one is more effective for the treatment of very severe osteoporotic vertebral compression fractures:PVP or PKP?. J Pain Res. 2018. 11: 2625-2631
11. Yuan WH, Hsu HC, Lai KL. Vertebroplasty and balloon kyphoplasty versus conservative treatment for osteoporotic vertebral compression fractures:A meta-analysis. Medicine (Baltimore). 2016. 95: e4491-
12. Zhang H, Xu C, Zhang T, Gao Z, Zhang T. Does Percutaneous Vertebroplasty or Balloon Kyphoplasty for Osteoporotic Vertebral Compression Fractures Increase the Incidence of New Vertebral Fractures?. A Meta-Analysis. Pain Physician. 2017. 20: E13-E28
13. Zhu RS, Kan SL, Ning GZ, Chen LX, Cao ZG, Jiang ZH. Which is the best treatment of osteoporotic vertebral compression fractures:balloon kyphoplasty, percutaneous vertebroplasty, or non-surgical treatment?A Bayesian network meta-analysis. Osteoporos Int. 2019. p.