- Department of Neurosurgery, Riverside University Health System, Riverside, California, USA
Correspondence Address:
Samir Kashyap
Department of Neurosurgery, Riverside University Health System, Riverside, California, USA
DOI:10.4103/sni.sni_142_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Samir Kashyap, Gohar Majeed, Shokry Lawandy. A rare case of Brown-Sequard syndrome caused by traumatic cervical epidural hematoma. 23-Oct-2018;9:213
How to cite this URL: Samir Kashyap, Gohar Majeed, Shokry Lawandy. A rare case of Brown-Sequard syndrome caused by traumatic cervical epidural hematoma. 23-Oct-2018;9:213. Available from: http://surgicalneurologyint.com/surgicalint-articles/9048/
Abstract
Background:Brown-Sequard syndrome (BSS) is a well-known entity that is most commonly caused by a penetrating injury to the spinal cord (e.g., stab wound or gunshot wound). It is characterized by an ipsilateral weakness (damage to corticospinal tracts) and contralateral loss of pain and temperature two levels below the lesion (damage to lateral spinothalamic tracts). Although, rarely non-penetrating injuries, tumors, disc herniations, infections, autoimmune diseases, and epidural hematomas (non-penetrating trauma and spontaneous) have contributed to BSS syndromes, there are only four cases of BSS in the literature attributed to traumatic spinal epidural hematomas. Here, we add an additional case involving a 59-year-old male.
Case Description:A 59-year-old male presented with a Brown-Sequard syndrome (BSS) after a motor vehicle accident. The magnetic resonance imaging (MRI) demonstrated a cervical epidural hematoma at the C7–T1 level. Following a T1 laminectomy and C6–T1 fusion, his neurological deficit markedly improved. Within six postoperative months, he regained full motor function.
Conclusion:For this patient and others with a traumatic cervical epidural hematoma (C7T1) resulting in a BSS, early decompression (within 48 hours) should result in marked postoperative neurological improvement.
Keywords: Brown-Sequard, cervical epidural hematoma, spinal trauma
BACKGROUND
Brown-Sequard syndrome (BSS) is a well-known entity that is most commonly caused by a penetrating injury to the spinal cord (e.g., stab wound or gunshot wound).First described in 1850, it is characterized by ipsilateral weakness (damage to corticospinal tracts) and contralateral loss of pain and temperature (e.g., two levels below the lesion reflecting damage to lateral spinothalamic tracts).[
CASE DESCRIPTION
Presentation
A 59-year-old Caucasian male was involved in a rollover motor vehicle accident. He was immediately reported to have paresthesias in the both upper extremities accompanied by profound weakness in his left lower extremity.
Clinical examination
Upon arrival to the Emergency Department, his Glasgow Coma Score was 15, but he was complaining of severe cervicothoracic midline tenderness. The motor examination revealed a left hemiparesis (4/5 in distal upper extremity and 2/5 lower extremity) with no right-sided weakness. The sensory examination demonstrated allodynia at the right C7 dermatome, and diminished light touch and pinprick sensation below T1. Rectal tone was present. There was no hyperreflexia or clonus, but he had bilateral Babinski signs.
Imaging
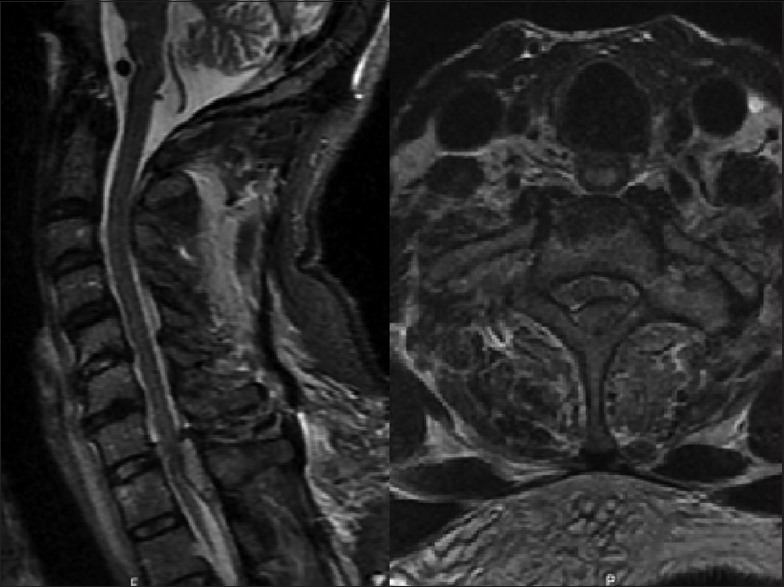
The initial CT of the cervical spine showed multiple areas of chronic degenerative changes without any fractures. However, the STAT MRI revealed a left paramedian dorsal epidural hematoma at the C7–T1 level causing cord compression along with complete disruption of the ligamentum flavum and C7T1 interspinous ligament [
Clinical course
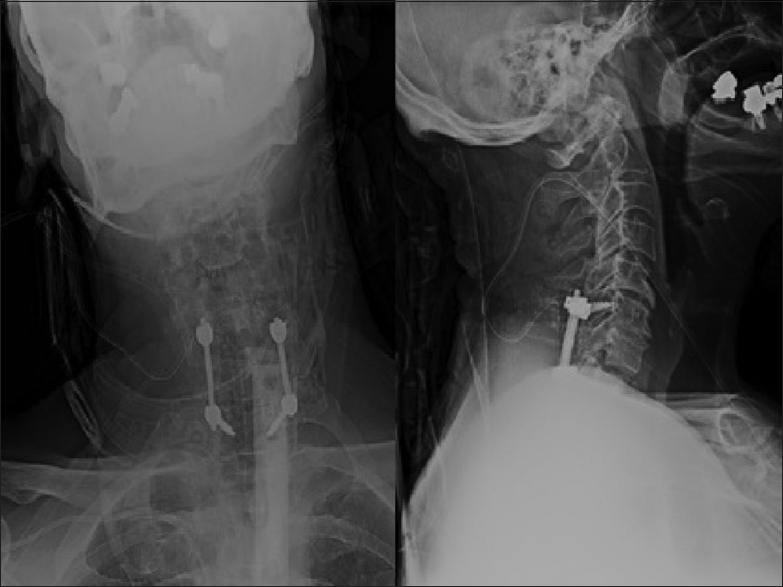
The patient taken to the operating room emergently for a T1 laminectomy, evacuation of the C7T1 epidural hematoma, and a C6–T1 instrumented fusion [
DISCUSSION
BSS secondary to a spinal epidural hematomas (SEDH) are extremely rare. In a meta-analysis conducted by Kreppel et al.[
Although non-surgical management may be feasible without a neurological deficit, for those with neurological dysfunction, urgent surgical decompression is warranted.[
The incidence of spontaneous SEDH is rare, reported in 0.1 per 100,000 people.[
In the setting of high-impact trauma, such as that experienced by our patient; development of a SEDH at the lower cervical levels was likely related to the rotatory/whiplash mechanism of injury most pronounced at these levels. Some controversy exists regarding whether the etiology of bleeding is arterial or venous in this condition.
There are a number of surgical approaches to posterior cervicothoracic epidural hematomas such as laminectomy, hemilaminectomy, and laminoplasty. Alternatively, for a symptomatic anterior SEDH, a direct approach such as a discectomy or corpectomy would likely be utilized.
We believe that urgent surgical decompression and evacuation of the hematoma played a vital role in our patient's neurological recovery. Yoon et al.[
CONCLUSION
Penetrating spinal trauma rarely results in a BSS attributed to a posterior cervicothoracic epidural hematoma. Immediate surgical management should be pursued if the patient has a significant neurological deficit (e.g., incomplete spinal cord injury) to avoid further irreversible symptoms progression.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Beatty RM, Winston KR. Spontaneous cervical epidural hematoma. A consideration of etiology. J Neurosurg. 1984. 61: 143-8
2. Borges LF, Zervas N, Lehrich J. Idiopathic Spinal Cord Herniation: A Treatable Cause of the Brown-Sequard Syndrome-Case Report. Neurosurgery. 1995. 36: 1028-33
3. Cai H-X, Liu C, Zhang J-F, Wan S-L, Uchida K, Fan S-W. Spontaneous epidural hematoma of thoracic spine presenting as Brown-Séquard syndrome: Report of a case with review of the literature. J Spinal Cord Med. 2011. 34: 432-6
4. Egido Herrero JA, Saldanã C, Jiménez A, Vázquez A, Varela de Seijas E, Mata P. Spontaneous cervical epidural hematoma with Brown-Séquard syndrome and spontaneous resolution. Case report. J Neurosurg Sci. 1992. 36: 117-9
5. Ehsan T, Henderson JM, Manepalli AN. Epidural Hematoma Producing Brown-Sequard Syndrome: A Case Due to Ruptured Hemangioma with Magnetic Resonance Imaging Findings. J Neuroimaging. 1996. 6: 62-3
6. Groen RJ, van Alphen HA. Operative treatment of spontaneous spinal epidural hematomas: A study of the factors determining postoperative outcome. Neurosurgery. 1996. 39: 494-508
7. Hancock JB, Field EM, Gadam R. Spinal epidural hematoma progressing to Brown-Sequard syndrome: Report of a case. J Emerg Med. 1997. 15: 309-12
8. Kobayashi N, Asamoto S, Doi H, Sugiyama H. Brown-Sèquard syndrome produced by cervical disc herniation: Report of two cases and review of the literature. Spine J. 2003. 3: 530-3
9. Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: A literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003. 26: 1-49
10. Kulkarni AG, Nag K, Shah S. Cervical epidural haematoma causing Brown-Sequard syndrome: A case report. J Orthop Surg (Hong Kong). 2013. 21: 372-4
11. Lawton MT, Porter RW, Heiserman JE, Jacobowitz R, Sonntag VK, Dickman CA. Surgical management of spinal epidural hematoma: Relationship between surgical timing and neurological outcome. J Neurosurg. 1995. 83: 1-7
12. Matsumura A, Namikawa T, Hashimoto R, Okamoto T, Yanagida I, Hoshi M. Clinical management for spontaneous spinal epidural hematoma: Diagnosis and treatment. Spine J. 2008. 8: 534-7
13. Mustafa MH. Spontaneous Spinal Epidural Hematoma, Brown-Séquard Syndrome, and Factor Xl Deficiency. Ann Intern Med. 1987. 106: 477-
14. Narberhaus B, Rivas I, Vilalta J, Abós J, Ugarte A. [Transient Brown-Séquard syndrome due to spontaneous spinal epidural hematoma]. Neurologia. 2002. 17: 384-7
15. Ofluoğlu E, Ozdemir A, Toplamaoğlu H, Sofuoğlu E. Spontaneous cervical epidural hematoma causing Brown-Sequard syndrome: Case report. Turk Neurosurg. 2009. 19: 99-102
16. Riaz S, Jiang H, Fox R, Lavoie M, Mahood JK. Spontaneous spinal epidural hematoma causing Brown-Sequard syndrome: Case report and review of the literature. J Emerg Med. 2007. 33: 241-4
17. Roy SP, Agrawal N. Brown Sequard Syndrome Secondary to a Spontaneous Cervical Epidural Hematoma-A Rare Entity. J Orthop Case Rep. 2012. 2: 23-5
18. Russman BS, Kazi KH. Spinal epidural hematoma and the Brown-Séquard syndrome. Neurology. 1971. 21: 1066-8
19. Segal DH, Lidov MW, Camins MB. Cervical epidural hematoma after chiropractic manipulation in a healthy young woman: Case report. Neurosurgery. 1996. 39: 1043-5
20. Seon H-J, Song M-K, Han J-Y, Choi I-S, Lee S-G. Spontaneous cervical epidural hematoma presenting as Brown-Sequard syndrome following repetitive Korean traditional deep bows. Ann Rehabil Med. 2013. 37: 123-6
21. Yoon BH, Park KS, Jung SS, Park MS, Kim S-M, Chung S-Y. Spontaneous cervical epidural hematoma causing Brown-Sequard syndrome. Korean J Spine. 2012. 9: 297-9
22. Zupruk GM, Mehta Z. Brown-Séquard syndrome associated with posttraumatic cervical epidural hematoma: Case report and review of the literature. Neurosurgery. 1989. 25: 278-80






John B Harris, MD FACS
Posted November 4, 2018, 8:07 am
Nice job!
I didn’t get the feeling that the joint was unstable ….
Could it have been done, without the instrumentation?