- Department of Orthopaedic Surgery, Osaka University Graduate School of Medicine, 2-2, Yamada-oka, Suita, Osaka, 565-0871, Japan
- Department of Orthopaedic Surgery, Osaka Police Hospital, 10-31 Kitayama, Tennouji, Osaka 543-0035, Japan
- Spine and Spinal Cord Center, Osaka Police Hospital, 10-31 Kitayama, Tennouji, Osaka 543-0035, Japan
Correspondence Address:
Daisuke Tateiwa
Spine and Spinal Cord Center, Osaka Police Hospital, 10-31 Kitayama, Tennouji, Osaka 543-0035, Japan
DOI:10.4103/sni.sni_280_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Daisuke Tateiwa, Ryoji Yamasaki, Kenta Ariga, Kenji Hayashida, Eiji Wada. An intraspinal extradural lipoma with spinal epidural lipomatosis: A case report and a review of literature. 23-Oct-2018;9:212
How to cite this URL: Daisuke Tateiwa, Ryoji Yamasaki, Kenta Ariga, Kenji Hayashida, Eiji Wada. An intraspinal extradural lipoma with spinal epidural lipomatosis: A case report and a review of literature. 23-Oct-2018;9:212. Available from: http://surgicalneurologyint.com/surgicalint-articles/9047/
Abstract
Background:Intraspinal extradural lipomas are very rare and should be differentiated from spinal epidural lipomatosis (SEL) and/or angiolipomas.
Case Description:A 76-year-old male presented with left lower extremity radiculopathy. The magnetic resonance imaging (MRI) revealed hyperplasia of epidural fat at the L2–3 and L3–4 levels accompanied by a lipomatous L4–5 mass. Following resection of this mass and hyperplastic epidural fat, the histological examination was consistent with an intraspinal extradural lipoma and SEL.
Conclusion:This case indicates that asymmetrical compression of the dural sac may be attributed to an intraspinal extradural lipoma vs. just SEL and/or an angiolipoma.
Keywords: Histological examination, intraspinal extradural lipoma, spinal epidural lipomatosis, spinal tumor
INTRODUCTION
An intraspinal extradural spinal lipoma without spinal dysraphism is very rare. It accounts for only 0.4%–0.8% of all intraspinal tumors.[
Herein, we present the clinical, radiographic, surgical, and pathological assessment of a patient with an intraspinal extradural lipoma and SEL.
CASE REPORT
History and examination
A 76-year-old male was presented with left lower extremity radiculopathy that had progressed over the last 2 years. Sixteen years before admission, an intracerebral hemorrhage left him hemiplegic on the left side, necessitating the use of a wheelchair.
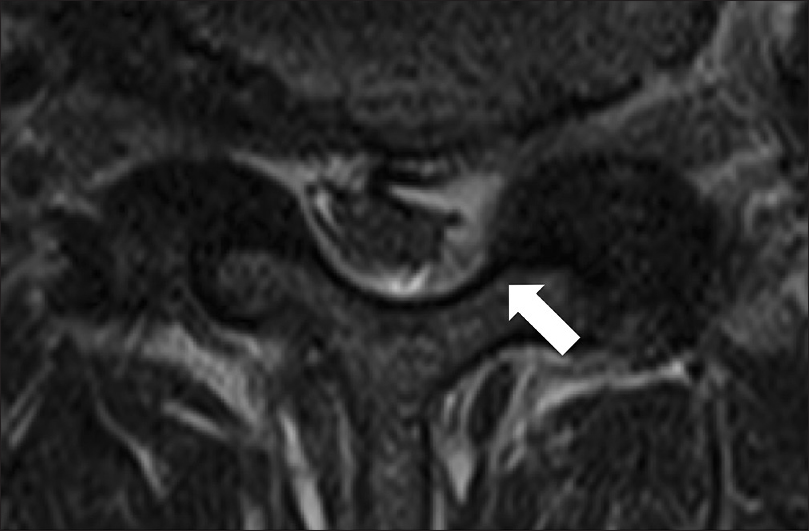
The magnetic resonance imaging (MRI) of the lumbar spine revealed spinal stenosis at the L2–3, 3–4, and 4–5 levels. Additionally, the T2-weighted images showed degenerative disc disease and hyperplastic epidural fat contributing to L2–3 and L3–4 stenosis [Figure
Operation and postoperative course
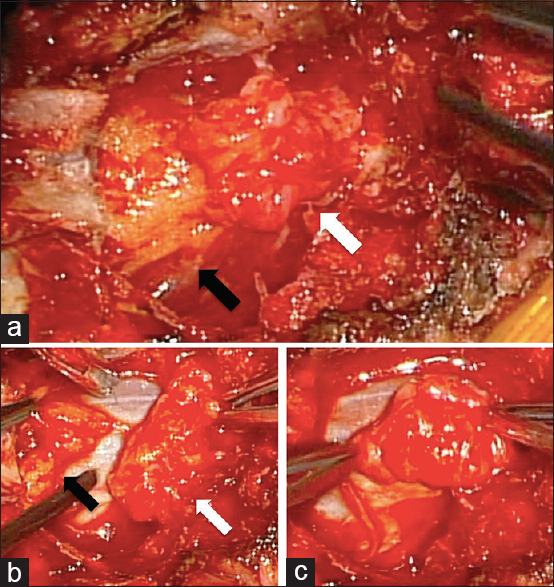
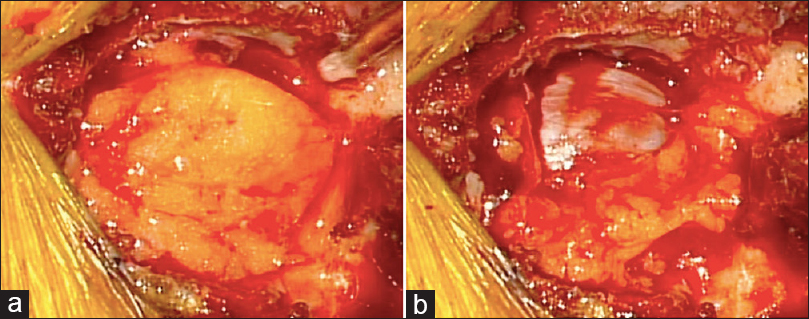
Seven months later due to persistent complaints, the patient underwent surgery consisting of fenestrations at the L2–3, 3–4, and 4–5 levels. At L4–5, a yellow, encapsulated, lobulated lipomatous mass with epidural fat filled the epidural space [Figure
Figure 3
(a) Fenestration at the L4–5 level was performed; a yellow, lobulated lipomatous mass (white arrow), and epidural fat (black arrow) were observed in the epidural space. (b) The mass (white arrow) was easily separated from epidural fat (black arrow). (c) Because the mass was enclosed by a fibrous capsule, we could resect it en bloc
Histologic analysis
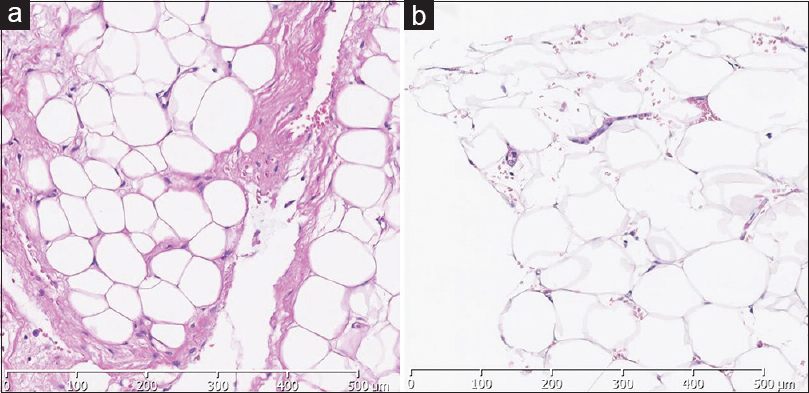
The histological examination of the encapsulated mass showed lobulated mature adipose tissue enclosed by fibrous tissue, compatible with a lipoma, while the histology of the L2–3 and L3–4 epidural fat was consistent with just mature adipose tissue; none of the slides demonstrated cellular atypia [Figure
DISCUSSION
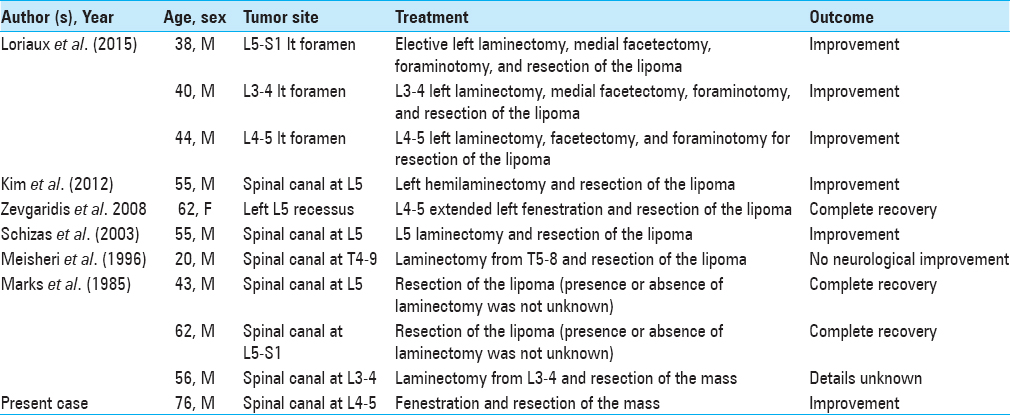
There are a few cases of intraspinal extradural lipoma without spinal dysraphism. Here, we reviewed 10 studies in the literature and summarized the diagnosis and surgical management of this 76-year-old male[
Intraspinal extradural lipomas typically occur in the lumbar spine (10 of 11 patients in the literature). Meisheri et al. reported a thoracic lipoma at the T4–9 level resulting in paraplegia.[
In the literature, the postoperative course for most patients was uneventful: three completely recovered (27%), six showed improvement (55%), one showed no improvement (9%), while one patient's status was unknown (9%).[
As these intraspinal extradural lipomas are rare, they may be easily overlooked,[
CONCLUSION
A 76-year-old male presented with a rare intraspinal extradural lipoma accompanied by SEL. These lesions are typically enclosed in a fibrous capsule, and present with asymmetric fatty compression of the lumbar dural sac on MRI.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Badami JP, Hinck VC. Symptomatic deposition of epidural fat in a morbidly obese woman. AJNR Am J Neuroradiol. 1982. 3: 664-5
2. Butti G, Gaetani P, Scelsi M, Pezzotta S. Extradural spinal lipomas. Report of two cases and review of the literature. Neurochirurgia. 1984. 27: 28-30
3. Kim HK, Koh SH, Chung KJ. Solitary epidural lipoma with ipsilateral facet arthritis causing lumbar radiculopathy. Asian Spine J. 2012. 6: 203-6
4. Loriaux DB, Adogwa O, Gottfried ON. Radiculopathy in the setting of lumbar nerve root compression due to an extradural intraforaminal lipoma: A report of 3 cases. J Neurosurg Spine. 2015. 23: 55-8
5. Marks SM, Miles JB, Shaw MD. Idiopathic spinal extradural lipomas: Three cases and review of the literature. Surg Neurol. 1985. 23: 153-6
6. Meisheri YV, Mehta S, Chattopadhyay K. Acute paraplegia due to an extradural spinal lipoma: Case report. Spinal cord. 1996. 34: 633-4
7. Rocchi G, Caroli E, Frati A, Cimatti M, Savlati M. Lumbar spinal angiolipomas: Report of two cases and review of the literature. Spinal Cord. 2004. 42: 313-6
8. Schizas C, Ballesteros C, Roy P. Cauda equina compression after trauma: An unusual presentation of spinal epidural lipoma. Spine. 2003. 28: E148-51
9. Zevgaridis D, Nanassis K, Zaramboukas T. Lumbar nerve root compression due to extradural, intraforaminal lipoma. An underdiagnosed entity?. J Neurosurg Spine. 2008. 9: 408-10