- Department of Biomedical and Dental Sciences, Morphological and Functional Images, University Hospital of Messina, Italy.
- Department of Clinical and Experimental Medicine, University of Messina, Messina, Italy.
- Department of Biomedicine, Neurosciences and Advanced Diagnostics, University of Palermo, Palermo, Italy.
Correspondence Address:
Giovanni Grasso
Department of Biomedical and Dental Sciences, Morphological and Functional Images, University Hospital of Messina, Italy.
DOI:10.25259/SNI_317_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Karol Galletta, Francesca Granata, Marcello Longo, Concetta Alafaci, Francesco S. De Ponte, Domenico Squillaci, Jolanda De Caro, Francesco Grillo, Filippo Benedetto, Rosa Musolino, Giovanni Grasso, Enrico Nastro Siniscalchi. An unusual internal carotid artery compression as a possible cause of Eagle syndrome – A novel hypothesis and an innovative surgical technique. 10-Sep-2019;10:174
How to cite this URL: Karol Galletta, Francesca Granata, Marcello Longo, Concetta Alafaci, Francesco S. De Ponte, Domenico Squillaci, Jolanda De Caro, Francesco Grillo, Filippo Benedetto, Rosa Musolino, Giovanni Grasso, Enrico Nastro Siniscalchi. An unusual internal carotid artery compression as a possible cause of Eagle syndrome – A novel hypothesis and an innovative surgical technique. 10-Sep-2019;10:174. Available from: http://surgicalneurologyint.com/surgicalint-articles/9620/
Abstract
Background: Eagle syndrome (ES) is a rare symptomatic condition generally caused by an elongated styloid process (SP) or calcification of the stylohyoid complex. On the diagnosis is made, its treatment remains subjective since the indications for surgical intervention are still not standardized. Although styloidectomy is the surgical treatment of choice, no consensus exists regarding the transcervical or/and transoral route. Here, we report our experience in a patient with bilateral internal carotid artery (ICA) dissection caused by ES, who underwent innovative surgical technique.
Case Description: A 53-year-old man, with the right-sided middle cerebral artery acute stroke, underwent computed tomography angiography 3 days after a successful endovascular treatment. The study showed a bilateral ICA dissection with bilateral hypertrophic SPs and a close relationship of ICAs with both SPs anteriorly and C1 transverse process posteriorly. Considering the occurrence of ICA compression by a styloid/C1 transverse process juxtaposition, the patient underwent the left partial C1 transversectomy by an extraoral approach. A temporary paresis of the ipsilateral lower lip lasted 1 month, with a partial remission after 3 months. The patient reported significant improvement of symptoms with a good esthetics and functional outcome.
Conclusion: A styloid/C1 transverse process juxtaposition should be considered as an alternative pathogenetic mechanism in vascular ES. When a posterior ICA compression by C1 transverse process is present, a bone reshaping of C1 rather than a conventional styloidectomy can be considered an efficacious treatment which allows a good preservation of the styloid muscles and ligaments.
Keywords: Eagle syndrome, Styloidectomy, Surgical treatment
INTRODUCTION
Eagle syndrome (ES) is a rare symptomatic condition generally caused by an elongated styloid process (SP) or calcification of the stylohyoid complex.[
Since the syndrome was first described by Eagle, in 1937,[
Here, we report on a patient with bilateral CAD caused by ES successfully treated by a partial surgical removal of C1 transverse process.
CASE REPORT
Clinical presentation
A 53-year-old man was admitted with a history of a left- sided weakness and facial drooping 3 h before the arrival. On neurologic examination, left hemiparesis, dysarthria, and facial palsy were noted at the admission (National Institutes of Health Stroke Scale [NIHSS]: 11).
A noncontrast computed tomography (CT) scan showed an acute thrombus extending from the right ICA bifurcation into the ipsilateral middle cerebral artery (MCA). Magnetic resonance (MR) imaging demonstrated an infarct involving the right basal ganglia and the insula (Alberta stroke programme early CT score: 7) along with an eccentric hyperintensity extended within the cervical segment of the right ICA wall, suggestive of an intramural hematoma. At the MR angiography, ICA terminus (ICA-T), MCA, and A1 segment of the anterior cerebral artery of the right side were absent. Fluid-attenuated inversion recovery and susceptibility-weighted imaging images showed good collaterals and a large thrombus (27 mm length) on the right ICA-MCA, respectively.
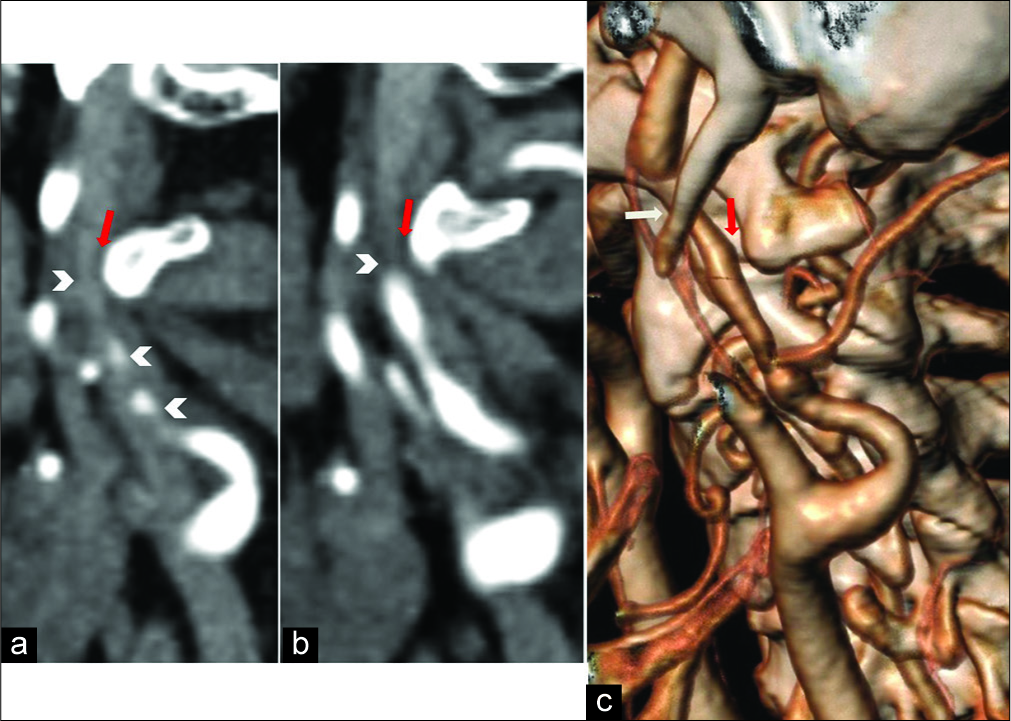
The patient underwent dynamic cerebral angiography for endovascular treatment. The right carotid angiogram showed a severe stenosis of ICA in the cervical segment and an ICA-T occlusion. After three attempts of direct thrombus aspiration (ADAPT technique) at the ICA-T and MCA, a successful revascularization of the vessels was obtained. After 12 h, his NIHSS improved to 3. Three days later, a CTA showed a bilateral ICA dissection with bilateral elongated SPs (35 mm) and a close proximity of ICA with both SPs anteriorly and C1 transverse process posteriorly [
Figure 1:
Computed tomography angiography examination. (a and b) Sagittal multiplanar reconstruction showing the left internal carotid artery (ICA) dissection with severe vessel stenosis (arrowheads). The close proximity between C1 transverse process and the posterior aspect of the dissected vessel is shown (red arrows). (c) Oblique volume rendering technique reconstruction technique depicts an unusual ICA compression by styloid process anteriorly (white arrow) and C1 transverse process posteriorly (red arrow).
Treatment
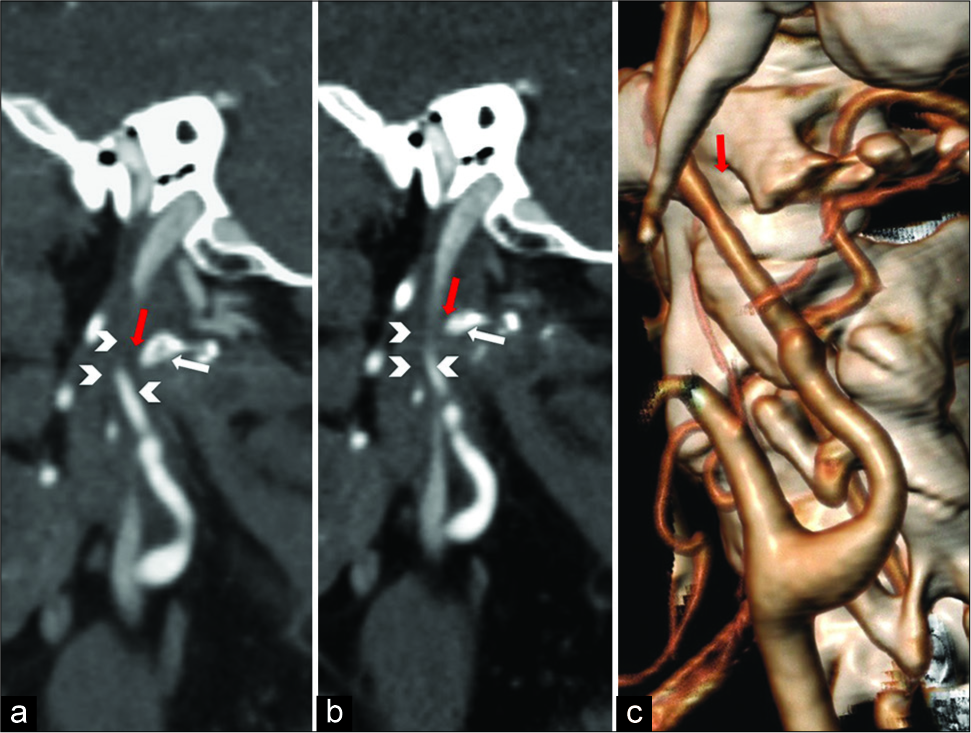
A surgical treatment was planned to free the left ICA. The patient underwent surgical treatment by an extraoral approach. A vertical skin incision of 4 cm in length was performed from the posterior border of the mandibular angle along with the anterior edge of sternocleidomastoid muscle (SCM). Once the platysma was opened, the superficial layer of deep cervical fascia was then excided. The head of the submandibular gland was mobilized superiorly while the SCM and posterior digastric muscle belly were retracted posteriorly to expose the SP. The SP was medially directed and the left ICA compressed by both SPs anteriorly and C1 transverse process posteriorly, with a direct impingement by the latter. To decompress the left ICA and at the same time, preserve the main muscular and ligamentous connections of the styloid chain, a portion of the left C1 transverse process was removed using a piezosurgical device [
Figure 2:
Postoperative computed tomography angiography examination. (a and b) Sagittal multiplanar reconstruction demonstrating the surgically generated distance (red arrows) between the reshaped C1 transverse process (white arrows) and internal carotid artery (ICA) (arrowheads). (c) Volume rendering technique reconstruction image showing the new anatomical relationship between ICA and C1 transverse process (red arrows).
A temporary paresis of the ipsilateral lower lip lasted 1 month, with a partial remission after 3 months. Overall, the patient reported significant improvement of symptoms with a good esthetics and functional outcome.
DISCUSSION
The SP is a bony projection located anterior to the stylomastoid foramen. Its normal length is individually variable, but in the majority of the people, it is between 20 and 30 mm.[
The classic type is related to trauma, with or without fracture, developing a locoregional compressive neuropathy. Symptoms may include neck and back throat, tongue base and tonsillar pain, odynophagia, otalgia, tinnitus, and sensation of having a foreign object in the throat.[
The role of the styloid/C1 transverse process juxtaposition as an effective cause of “vascular type” ES, even in the setting of a normal length styloid process, has been already reported.[
Styloidectomy is the surgical treatment of choice for ES and involves shortening the styloid process. However, to date, the indications for surgical intervention are not consistent and there is no definitive agreement on whether the transoral or transcervical approach is superior.[
In our case, a partial surgical removal of C1 transverse process rather than the classic styloidectomy was performed. Such an approach provided with an optimal ICA decompression and a good preservation of the styloid muscles and ligaments.
CONCLUSION
A styloid/C1 transverse process juxtaposition should be considered as an alternative pathogenetic mechanism in vascular ES. When a posterior ICA compression by C1 transverse process is present, a bone reshaping of C1 rather than a conventional styloidectomy can be considered an efficacious treatment since it provides with a good preservation of the styloid muscles and ligaments. Further studies are necessary to assess the effectiveness of such new surgical approach.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al Weteid AS, Miloro M. Transoral endoscopic-assisted styloidectomy: How should eagle syndrome be managed surgically?. Int J Oral Maxillofac Surg. 2015. 44: 1181-7
2. Bafaqeeh SA. Eagle syndrome: Classic and carotid artery types. J Otolaryngol. 2000. 29: 88-94
3. Callahan B, Kang J, Dudekula A, Eusterman V, Rabb CH. New eagle’s syndrome variant complicating management of intracranial pressure after traumatic brain injury. Inj Extra. 2010. 41: 41-4
4. Chase DC, Zarmen A, Bigelow WC, McCoy JM. Eagle’s syndrome: A comparison of intraoral versus extraoral surgical approaches. Oral Surg Oral Med Oral Pathol. 1986. 62: 625-9
5. Choudhari SY, Sangavi AB. A clinical study of the patients with elongated styloid process. Int J Otorhinolaryngol Head Neck Surg. 2017. 3: 400-3
6. Cullu N, Deveer M, Sahan M, Tetiker H, Yilmaz M. Radiological evaluation of the styloid process length in the normal population. Folia Morphol (Warsz). 2013. 72: 318-21
7. David J, Lieb M, Rahimi SA. Stylocarotid artery syndrome. J Vasc Surg. 2014. 60: 1661-3
8. Demirtaş H, Kayan M, Koyuncuoğlu HR, Çelik AO, Kara M, Şengeze N. Eagle syndrome causing vascular compression with cervical rotation: Case report. Pol J Radiol. 2016. 81: 277-80
9. Eagle WW. Elongated styloid process; symptoms and treatment. AMA Arch Otolaryngol. 1958. 67: 172-6
10. Eagle WW. The symptoms, diagnosis and treatment of the elongated styloid process. Am Surg. 1962. 28: 1-5
11. Farhat HI, Elhammady MS, Ziayee H, Aziz-Sultan MA, Heros RC. Eagle syndrome as a cause of transient ischemic attacks. J Neurosurg. 2009. 110: 90-3
12. Fini G, Gasparini G, Filippini F, Becelli R, Marcotullio D. The long styloid process syndrome or eagle’s syndrome. J Craniomaxillofac Surg. 2000. 28: 123-7
13. Galletta K, Siniscalchi EN, Cicciù M, Velo M, Granata F. Eagle syndrome: A wide spectrum of clinical and neuroradiological findings from cervico-facial pain to cerebral ischemia. J Craniofac Surg. 2019. 30: e424-8
14. Hardin FM, Xiao R, Burkey BB. Surgical management of patients with eagle syndrome. Am J Otolaryngol. 2018. 39: 481-4
15. Ho S, Luginbuhl A, Finden S, Curry JM, Cognetti DM. Styloid/ C1 transverse process juxtaposition as a cause of eagle’s syndrome. Head Neck. 2015. 37: E153-6
16. Jalisi S, Jamal BT, Grillone GA. Surgical management of long-standing eagle’s syndrome. Ann Maxillofac Surg. 2017. 7: 232-6
17. Kazmierski R, Wierzbicka M, Kotecka-Sowinska E, Banaszewski J, Pawlak MA. Expansion of the classification system for eagle syndrome. Ann Intern Med. 2018. 168: 746-7
18. Keur JJ, Campbell JP, McCarthy JF, Ralph WJ. The clinical significance of the elongated styloid process. Oral Surg Oral Med Oral Pathol. 1986. 61: 399-404
19. Koshy JM, Narayan M, Narayanan S, Priya BS, Sumathy G. Elongated styloid process: A study. J Pharm Bioallied Sci. 2015. 7: S131-3
20. Lindeman P. The elongated styloid process as a cause of throat discomfort. Four case reports. J Laryngol Otol. 1985. 99: 505-8
21. Lorman JG, Biggs JR. The eagle syndrome. AJR Am J Roentgenol. 1983. 140: 881-2
22. Mendelsohn AH, Berke GS, Chhetri DK. Heterogeneity in the clinical presentation of eagle’s syndrome. Otolaryngol Head Neck Surg. 2006. 134: 389-93
23. Ogura T, Mineharu Y, Todo K, Kohara N, Sakai N. Carotid artery dissection caused by an elongated styloid process: Three case reports and review of the literature. NMC Case Rep J. 2015. 2: 21-5
24. Öztaş B, Orhan K. Investigation of the incidence of stylohyoid ligament calcifications with panoramic radiographs. J Investig Clin Dent. 2012. 3: 30-5
25. Pokharel M, Karki S, Shrestha I, Shrestha BL, Khanal K, Amatya RC. Clinicoradiologic evaluation of eagle’s syndrome and its management. Kathmandu Univ Med J (KUMJ). 2013. 11: 305-9
26. Smoot TW, Taha A, Tarlov N, Riebe B. Eagle syndrome: A case report of stylocarotid syndrome with internal carotid artery dissection. Interv Neuroradiol. 2017. 23: 433-6
27. Valerio CS, Peyneau PD, de Sousa AC, Cardoso FO, de Oliveira DR, Taitson PF. Stylohyoid syndrome: Surgical approach. J Craniofac Surg. 2012. 23: e138-40