- Department of Neurosurgery, National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru, Karnataka, India
Correspondence Address:
K. V. L. N. Rao
Department of Neurosurgery, National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru, Karnataka, India
DOI:10.4103/sni.sni_448_17
Copyright: © 2019 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Manish Beniwal, V. Vikas, K. V. L. N. Rao, Dwarkanath Srinivas, S. Sampath. An unusual site of metastasis from carcinoma of tongue – metastasis to lumbar vertebrae: A case report and review of literature. 15-Mar-2019;10:33
How to cite this URL: Manish Beniwal, V. Vikas, K. V. L. N. Rao, Dwarkanath Srinivas, S. Sampath. An unusual site of metastasis from carcinoma of tongue – metastasis to lumbar vertebrae: A case report and review of literature. 15-Mar-2019;10:33. Available from: http://surgicalneurologyint.com/surgicalint-articles/9250/
Abstract
Background:Carcinoma of tongue is a common site of oral cancer. It usually occurs at mean age of 61.1 years and is more common in males when compared with females. It commonly spreads directly and through lymphatics to the surrounding structures. It has a low incidence of hematogenous metastasis. Lung is the usual distant metastasis site for carcinoma of tongue and other head and neck cancers. Metastases to vertebrae are rare and very few cases have been reported.
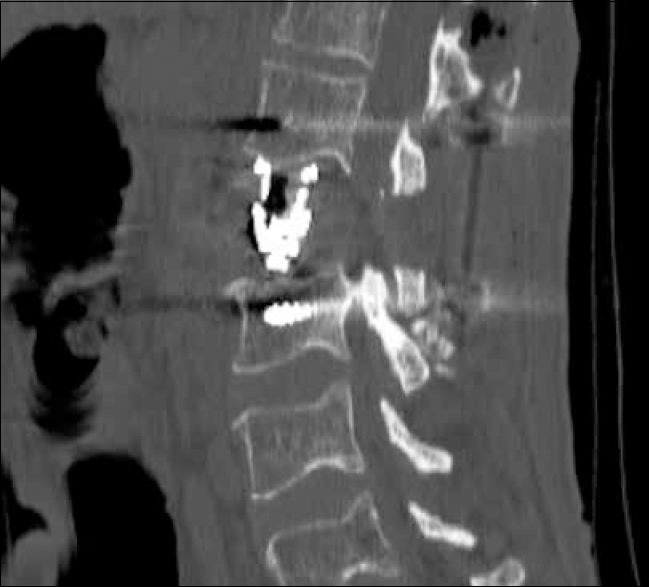
Case Description:We report a rare case of carcinoma of tongue spreading to lumbar vertebrae causing destruction of the body and thecal sac compression. A patient underwent posterior transpedicular approach, tumor decompression, and titanium cage placement. The patient had good relief of symptoms and could be mobilized on first postoperative day.
Conclusion:Hematogenous spread to the spine is a rare phenomenon but should be kept in mind particularly in advanced stage of oral cancers.
Keywords: Carcinoma of tongue, lumbar, metastasis, vertebrae
INTRODUCTION
One of the common site of oral cancer is tongue and accounts for 2% of all cancer deaths.[
Approximately 5%–10% of all cancer patients develop spinal metastasis;[
CASE REPORT
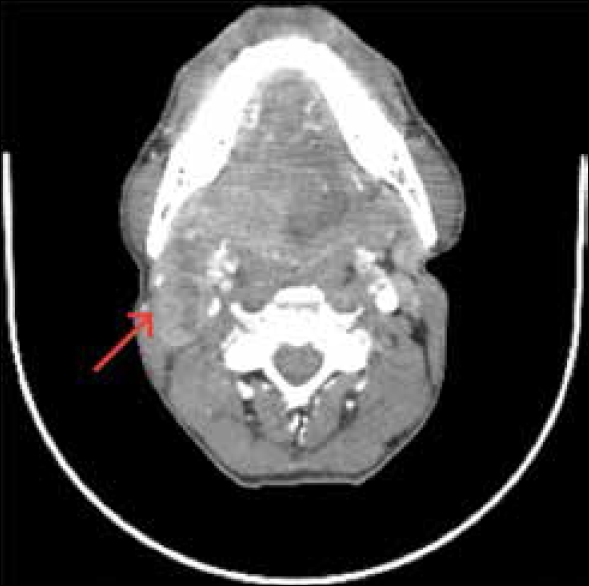
A 50-year-old patient, chronic smoker, presented to us with a non-healing ulcer on tongue with restricted mouth opening (around 2 fingerbreadth) for 3 months. Examination of oral cavity revealed non-healing ulcer on right lateral border of tongue with palpable neck nodes [
On examination, patient was bed-bound and unable to move out of bed due to severe pain which localized to lumbar region, with tenderness and restriction of movements. Tone, bulk, and power were normal in both lower limbs; however, he had sensory loss of 60%–70%, in L2 and L3 dermatomes in bilateral lower limbs.
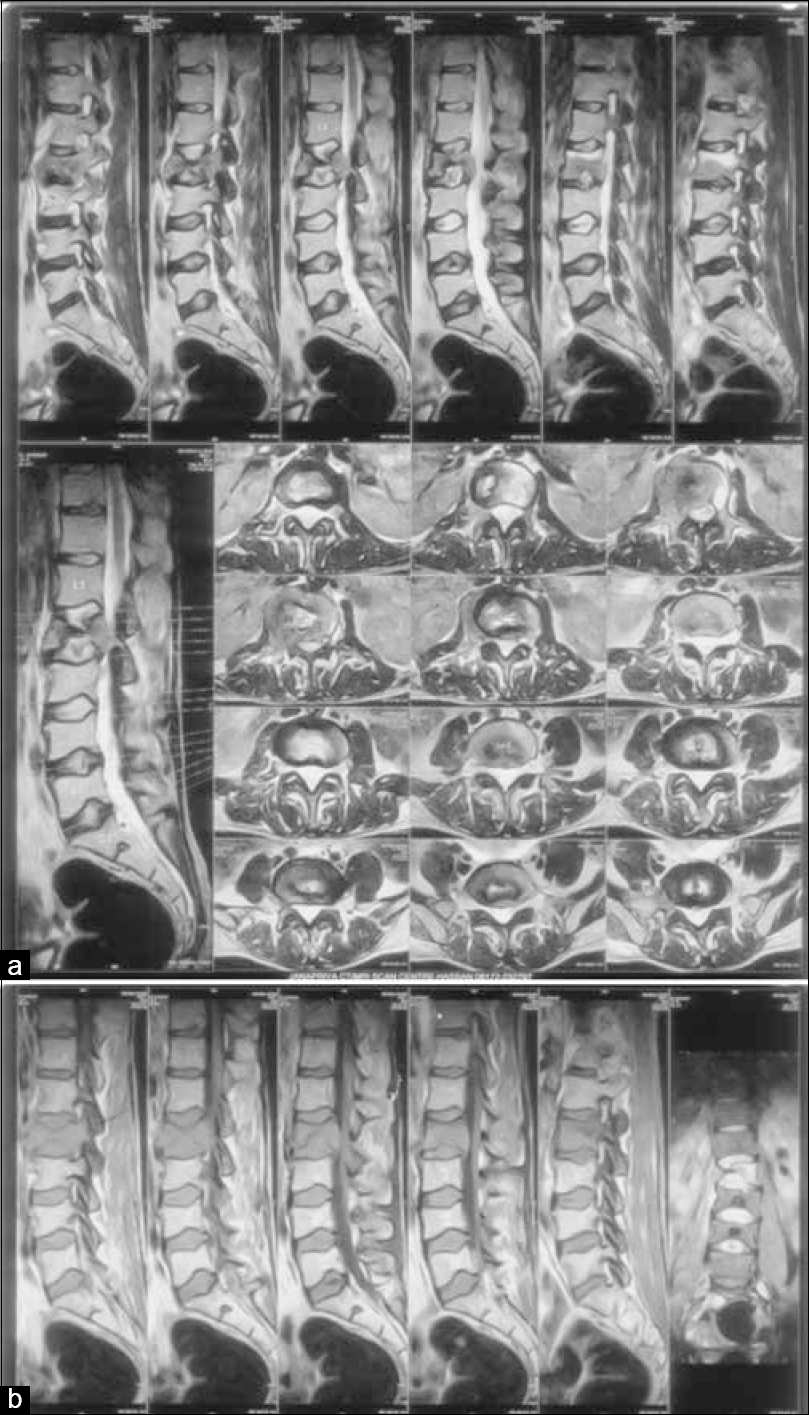
He was evaluated with magnetic resonance imaging (MRI) and CT of lumbar spine with whole-spine screening. On MRI imaging, there was destruction of L2 vertebral body with hypointense signal on T1WI and heterogeneous signal on T2WI. There was relative preservation of disc space, but vertebral body was collapsed causing a focal kyphosis with compression of thecal sac, predominantly on the right side [Figure
Figure 7
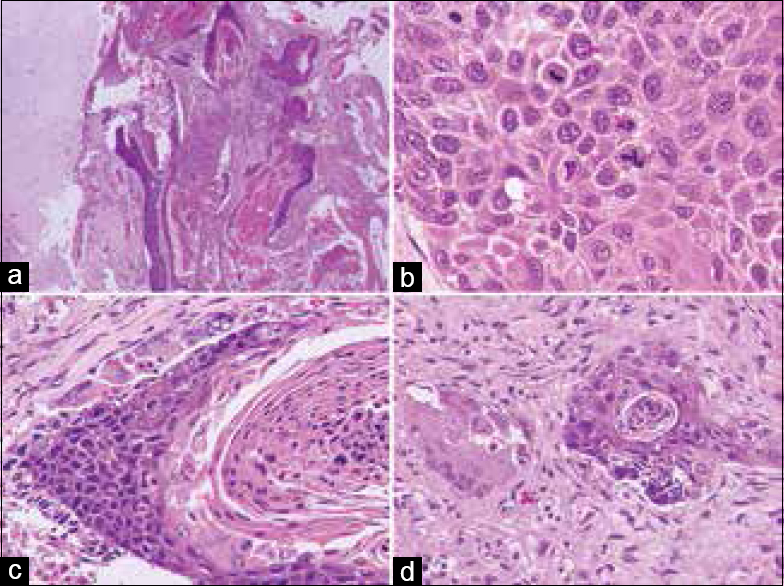
Spinal metastasis of squamous cell carcinoma. (a) Large irregular deposits of neoplastic epithelial cells in fibrocollagenous soft tissue (right) adjacent to normal disc cartilage (left). (b) A cohesive cluster of malignant squamous epithelial cells with brisk mitoses. (c) Keratinizing neoplastic tumor cells partially rimmed at the top by foreign body giant cell reaction against keratin material. (d) Closer view of a foreign body giant cell (left) with neoplastic cells and keratin (right). [Stain: a–d: H and E; magnification – a: 20×, c, d: band 80×)
The patient was discharged from the hospital on postoperative day 5 and sent for continuation radiotherapy again. At 5 months of follow-up, the patient had completed adjuvant therapy and was ambulatory.
DISCUSSION
Carcinoma of tongue is one of the most common carcinoma of all oral cavity, and about half of them involve the base of the tongue.[
The treatment offered in advanced cases of head and neck malignancy is often palliative. As our patient was in stage IV B, he was started on chemoradiotherapy by oncologist. During treatment, he developed severe back pain after a trivial fall.
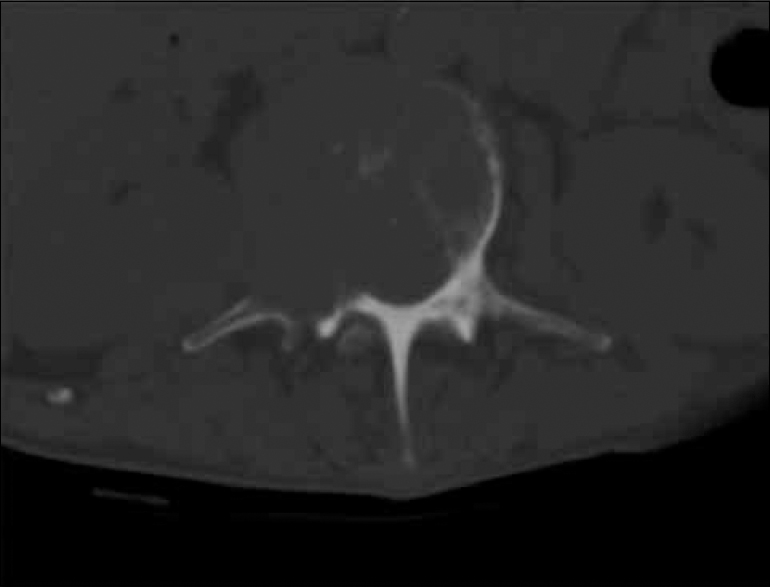
We evaluated him with MRI lumbosacral spine, which showed destructive lesion in the L2 vertebral body. As tuberculosis is more common in our country, we considered tuberculosis spine as the first possible diagnosis; however, there was no significant paravertebral collection and no involvement of adjacent disc spaces which were odd points. This made us to consider diagnosis of metastasis from tongue carcinoma, although it is rare from this primary site. CT scan lumbosacral region revealed destruction of vertebral body with involvement of right pedicle, favoring diagnosis of metastasis.
It is very well known that if metastatic vertebral disease is left untreated, it may lead to paraplegia,[
Prognosis for metastatic spine disease is dependent on several factors. Patients with single-level involvement have a better survival rate (average survival, 12.9 months) than patients with multiple-level involvement (average, 7.9 months).[
As our patient is 50 years of age and had only single vertebral body (L2) involvement, prognosis is likely to be good.
CONCLUSION
Our case report substantially adds to the existing case reports of carcinoma of tongue with metastasis to spine which is a rare event. Advanced cases of oral carcinoma can be very aggressive and metastatic spread to spine should be considered as a possibility though it is rare, especially when patient presents persistent back pain. Vertebral metastasis from oral cancer is due to hematogenous spread which usually occurs in advanced stage of oral cancers.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barron KD, Hirano A, Araki S, Terry RD. Experiences with metastatic neoplasms involving the spinal cord. Neurology. 1959. 9: 91-106
2. Carlson ER, Ord RA. Vertebral metastases from oral squamous cell carcinoma. J Oral Maxillofac Surg. 2002. 60: 858-62
3. Feng H, Wang J, Guo P, Xu J, Feng J. C3 vertebral metastases from tongue adenoid cystic carcinoma: A rare case report. Medicine. 2015. 94: e1135-
4. Gilbert RW, Kim JH, Posner JB. Epidural spinal cord compression from metastatic tumor: Diagnosis and treatment. Ann Neurol. 1978. 3: 40-51
5. Gorsky M, Epstein JB, Oakley C, Le ND, Hay J, Stevenson-Moore P. Carcinoma of the tongue: A case series analysis of clinical presentation, risk factors, staging, and outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004. 98: 546-52
6. Gourin CG, Johnson JT. Surgical treatment of squamous cell carcinoma of the base of tongue. Head Neck. 2001. 23: 653-60
7. Greenberg HS, Kim JH, Posner JB. Epidural spinal cord compression from metastatic tumor: Results with a new treatment protocol. Ann Neurol. 1980. 8: 361-6
8. Harrington KD. Metastatic disease of the spine. J Bone Joint Surg Am. 1986. 68: 1110-5
9. Jaffe HL.editors. Tumors and tumorous conditions of the bones and joints. Philadelphia: Lea and Febinger; 1958. p.
10. Lee KH, Halfpenny W, Thiruchelvam JK. Spinal cord compression in patients with oral squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. 103: e16-8
11. Mones RJ, Dozier D, Berrett A. Analysis of medical treatment of malignant extradural spinal cord tumors. Cancer Metastasis Rev. 1842. p. 19-
12. Patel SC, Carpenter WR, Tyree S, Couch ME, Weissler M, Hackman T. Increasing incidence of oral tongue squamous cell carcinoma in young white women, age 18 to 44 years. J Clin Oncol. 2011. 29: 1488-94
13. Sano D, Myers JN. Metastasis of squamous cell carcinoma of the oral tongue. Cancer Metastasis Rev. 2007. 26: 645-62
14. Shimizu K, Shikata J, Iida H, Iwasaki R, Yoshikawa J, Yamamuro T. Posterior decompression and stabilization for multiple metastatic tumors of the spine. Spine (Phila Pa. 1976. 1992;17: 1400-4
15. Tornwall J, Snall J, Mesimaki K. A rare case of spinal cord metastases from oral SCC. Br J Oral Maxillofac Surg. 2008. 46: 594-5
16. Weigel B, Maghsudi M, Neumann C, Kretschmer R, Muller FJ, Nerlich M. Surgical management of symptomatic spinal metastases. Postoperative outcome and quality of life. Spine (Phila Pa 1976). 1999. 24: 2240-6