- Department of Neurosurgery, Head and Neck Surgery, Keio University School of Medicine, Shinjuku, Tokyo, Japan
- Department of Otorhinolaryngology, Head and Neck Surgery, Keio University School of Medicine, Shinjuku, Tokyo, Japan
Correspondence Address:
Ryogo Kikuchi
Department of Neurosurgery, Head and Neck Surgery, Keio University School of Medicine, Shinjuku, Tokyo, Japan
DOI:10.4103/2152-7806.168313
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kikuchi R, Toda M, Tomita T, Ogawa K, Yoshida K. Analysis of sphenoid sinus lateral pneumatization for endonasal endoscopic surgery. Surg Neurol Int 27-Oct-2015;6:166
How to cite this URL: Kikuchi R, Toda M, Tomita T, Ogawa K, Yoshida K. Analysis of sphenoid sinus lateral pneumatization for endonasal endoscopic surgery. Surg Neurol Int 27-Oct-2015;6:166. Available from: http://surgicalneurologyint.com/surgicalint_articles/analysis-of-sphenoid-sinus-lateral-pneumatization-for-endonasal-endoscopic-surgery/
Abstract
Background:The purpose of this study was to analyze sphenoid sinus lateral pneumatization (SSLP), especially in Asian populations, and to identify cautionary items when using the endoscopic endonasal approach (EEA) for parasellar/lateral lesions.
Methods:We analyzed SSLP and the width of SS (SSW) in 121 patients who had undergone EEA from 2008 to 2013 at the Division of Neurosurgery, Keio University Hospital. SSLP was defined as the distance between the SS lateral edge and the medial aspect of the pterygoid process on coronal reconstruction computed tomography. SSW was defined as the distance between the midline and lateral wall. We recorded SSLP and SSW for 242 sides. Further, we present two characteristic cases.
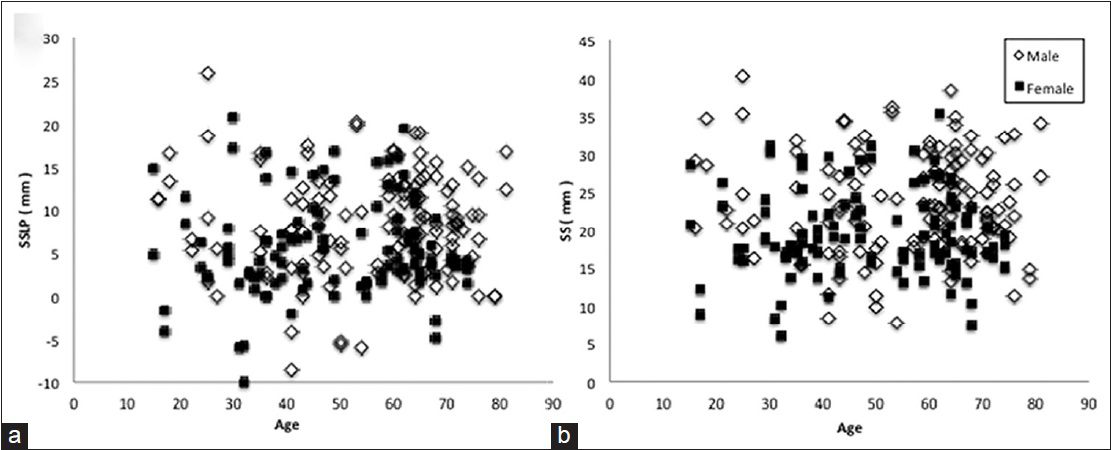
Results:The average SSLP and SSW were 7.0 mm (−10.0–25.8 mm) and 21.8 mm (6.0–40.2 mm), respectively. No correlation between pneumatization and age was observed at age 15 or more. Sphenoid pneumatization was significantly wider in male than in female patients. There was no relationship between lateral and sagittal plane pneumatization. In a patient with recurrent chordoma who had an undeveloped SSLP, the tumor was removed via the medial space in the internal carotid artery. In another patient who had a giant pituitary adenoma and average SSLP, the tumor was located in the middle cranial fossa and was removed via the lateral internal carotid space through the left SSLP.
Conclusions:Wide variations were observed in SSLP and SSW. For EEA, pneumatization is an instrument corridor. Preoperative assessment of SSLP is important, especially for parasellar lesions.
Keywords: Endoscopic endonasal surgery, pneumatization, sphenoid sinus
INTRODUCTION
Consequent to recent developments in endoscopic techniques and instruments, the endoscopic endonasal approach (EEA) has evolved to provide access to lateral cavernous sinus lesions. Due to expanded indications, numerous studies have focused on the endoscopic anatomy of the sphenoid sinus (SS), which is the platform for EEA.[
MATERIALS AND METHODS
Radiological measurements
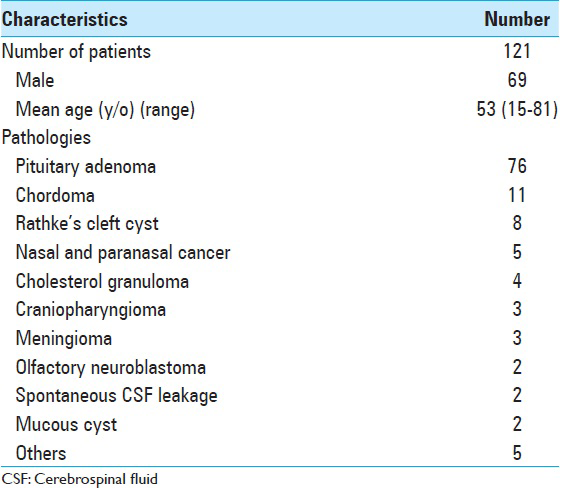
We collected data from consecutive patients who underwent the EEA between 2008 and 2013 in the Division of Neurosurgery at Keio University Hospital. Patients with pathological legions involving the SSLP were excluded. We assessed the SS in 69 men and 52 women, with an average age of 53 years (15–81 years). Patient characteristics are shown in
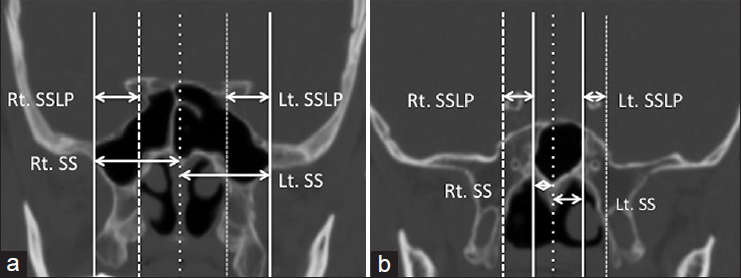
SSLP was defined as the distance from the lateral SS to the medial aspect of the pterygoid process, which is the anatomical limitation for the EEA, on coronal reconstruction images. The width of SS (SSW) was defined as the distance between the midline and the lateral aspect of the SS as shown in
Illustrative case presentation
We reviewed clinical data and radiological assessments of SSLP in 2 patients who underwent the EEA for parasellar and lateral lesions in the Division of Neurosurgery at Keio University Hospital.
RESULTS
Radiological results
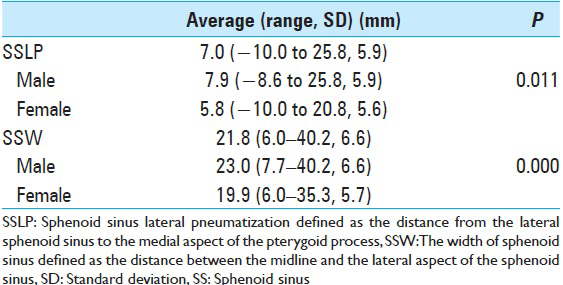
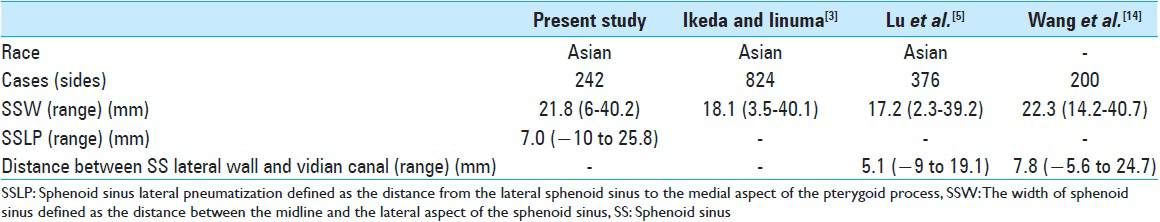
SSW averaged 21.7 mm (7.7–36.1 mm) on the right side and 21.9 mm (6.0–40.2 mm) on the left. The average SSW for both sides was 21.8 mm (6.0–40.2 mm) as shown in
Case presentation
Characteristic cases are shown in Figures
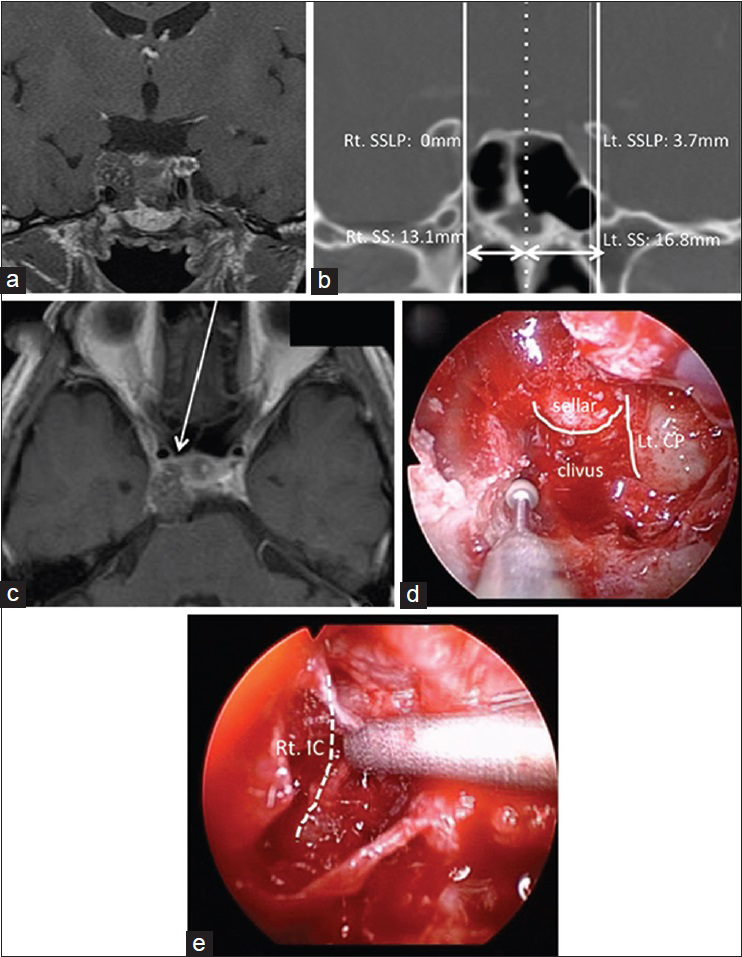
Figure 3
Case 1: A case of recurrent chordoma. (a) Preoperative coronal contrast enhanced MRI revealing a right parasellar tumor. (b) Preoperative coronal CT scan showing the left SSLP is 3.7 mm and the right SSLP is 0.0 mm. (c) Preoperative axial contrast enhanced MRI showing the tumor is located behind the right IC. The arrow shows the approach via the space medial to the IC. (d) Intraoperative view showing the sella turcica and left carotid prominence after removal of the anterior wall of the SS during endoscopic endonasal surgery. The right carotid prominence was unclear. (e) Intraoperative view showing the right IC and removal of tumor behind the artery. CT, computed tomography; IC, internal carotid artery; Lt, left; MRI, magnetic resonance imaging; Rt, right; SSW, the width of sphenoid sinus; SSLP, sphenoid sinus lateral pneumatization
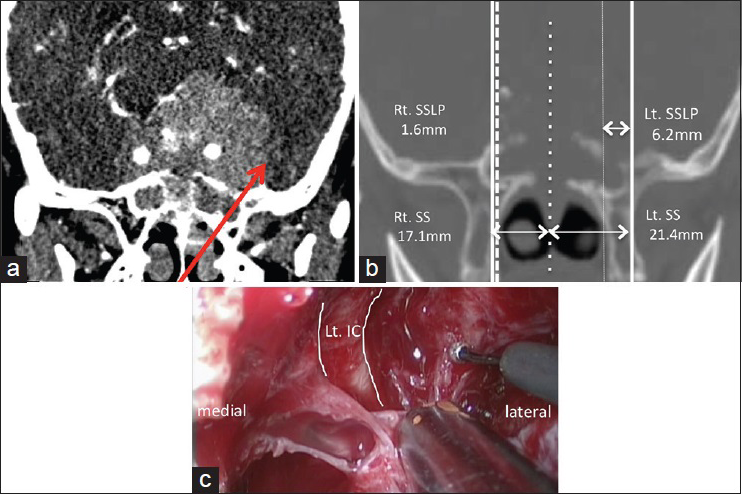
Figure 4
Case 2: A case of giant pituitary adenoma. (a) Preoperative oblique-coronal contrast enhanced CT showing a giant pituitary adenoma that encases the bilateral internal carotid arteries (ICs). The arrow shows the approach to the middle fossa via left SSLP. (b) Preoperative coronal CT scan showing the right SSLP is 1.6 mm and the left is 6.2 mm. (c) Intraoperative view showing the left middle fossa tumor through the space lateral to the left IC. CT, computed tomography; IC, internal carotid artery; Lt, left; MT, middle turbinate; MRI, magnetic resonance imaging; NS, nasal septum; SPF, sphenopalatine foramen; SS, the width of sphenoid sinus; SSLP, sphenoid sinus lateral pneumatization.
Case 1
A 43-year-old male was presented with double vision. Contrast-enhanced magnetic resonance imaging (MRI) showed a right parasellar tumor located behind the right internal carotid artery [Figure
Case 2
A 77-year-old female with almost complete left eye blindness noticed worsening right eye hemianopia. Contrast-enhanced MRI showed a giant pituitary adenoma extending to the left middle fossa beyond the internal carotid artery [
DISCUSSION
We measured SSW and SSLP in 121 patients, totaling 242 sides. There were wide variations in SSLP and SSW. No relationship was observed between the lateral and sagittal plane pneumatization or patient age.
SSLP did not develop in Case 1. In this case, we could remove the tumor, but it was very difficult because of a limited operation field. In Case 2, we could find the space lateral to the internal carotid artery through SSLP, and optic nerve decompression was successfully achieved.
In endoscopic endonasal surgery, working space is very important, even if the field of view can be secured. SSLP is an important corridor to reach the lateral lesions of the cavernous sinus. If SSLP is not developed, we have to drill bone around the internal carotid artery to approach lateral lesions of the cavernous sinus, which is not an easy endoscopic operation field. Therefore, the preoperative assessment of SS pneumatization is important in choosing an approach for operations of parasellar and lateral lesions.
CONCLUSIONS
Wide variations of SSLP were observed. SSLP and SSW in Asians are possibly smaller than in Euro-Americans. In endoscopic endonasal surgery, SS pneumatization is an important instrument corridor. With undeveloped SSLP, it is difficult to reach lateral lesions of the internal carotid artery and the operation field is restricted. Therefore, preoperative assessment of SSLP is important for using the EEA, especially for parasellar and lateral lesions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Amin SM, Nasr AY, Saleh HA, Foad MM, Herzallah IR. Endoscopic orientation of the parasellar region in sphenoid sinus with ill-defined bony landmarks: An anatomic study. Skull Base. 2010. 20: 421-8
2. Elkammash TH, Enaba MM, Awadalla AM. Variability in sphenoid sinus pneumatization and its impact upon reduction of complications following sellar region surgeries. Egypt J Radiol Nucl Med. 2014. 45: 705-14
3. Ikeda T, Iinuma T. Surgical anatomy of the sphenoid sinus - Development and intersinus septum. Nihon Jibiinkoka Gakkai Kaiho. 1992. 95: 214-23
4. Kassam AB, Vescan AD, Carrau RL, Prevedello DM, Gardner P, Mintz AH. Expanded endonasal approach: Vidian canal as a landmark to the petrous internal carotid artery. J Neurosurg. 2008. 108: 177-83
5. Lu Y, Pan J, Qi S, Shi J, Zhang X, Wu K. Pneumatization of the sphenoid sinus in Chinese: The differences from Caucasian and its application in the extended transsphenoidal approach. J Anat. 2011. 219: 132-42
6. Magro F, Solari D, Cavallo LM, Samii A, Cappabianca P, Paternò V. The endoscopic endonasal approach to the lateral recess of the sphenoid sinus via the pterygopalatine fossa: Comparison of endoscopic and radiological landmarks. Neurosurgery. 2006. 59: 237-42
7. Mato D, Y okota H, Hirono S, Martino J, Saeki N. The vidian canal: Radiological features in Japanese population and clinical implications. Neurol Med Chir (Tokyo). 2015. 55: 71-6
8. Peris-Celda M, Kucukyuruk B, Monroy-Sosa A, Funaki T, Valentine R, Rhoton AL. The recesses of the sellar wall of the sphenoid sinus and their intracranial relationships. Neurosurgery. 2013. 73: 117-31
9. Renn WH, Rhoton AL. Microsurgical anatomy of the sellar region. J Neurosurg. 1975. 43: 288-98
10. Tomovic S, Esmaeili A, Chan NJ, Shukla PA, Choudhry OJ, Liu JK. High-resolution computed tomography analysis of variations of the sphenoid sinus. J Neurol Surg B Skull Base. 2013. 74: 82-90
11. Vaezi A, Cardenas E, Pinheiro-Neto C, Paluzzi A, Branstetter BF, Gardner PA.editors. Classification of sphenoid sinus pneumatization: Relevance for endoscopic skull base surgery. Laryngoscope. 2015. 125: 577-81
12. Vescan AD, Snyderman CH, Carrau RL, Mintz A, Gardner P, Branstetter B. Vidian canal: Analysis and relationship to the internal carotid artery. Laryngoscope. 2007. 117: 1338-42
13. Wakuta N, Ueba T, Abe H, Inoue T, Tschabitscher M. Endoscopic endonasal surgical approach to the oculomotor trigone from the cavernous sinus. Neurol Med Chir (Tokyo). 2014. 54: 612-6
14. Wang J, Bidari S, Inoue K, Yang H, Rhoton A. Extensions of the sphenoid sinus: A new classification. Neurosurgery. 2010. 66: 797-816