- Department of Neurosurgery, Kanto Rosai Hospital, Kawasaki, Japan
- Department of Neurology, Kanto Rosai Hospital, Kawasaki, Japan
Correspondence Address:
Motohiro Nomura
Department of Neurology, Kanto Rosai Hospital, Kawasaki, Japan
DOI:10.4103/sni.sni_126_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Motohiro Nomura, Eiichi Baba, Kazutaka Shirokane, Atsushi Tsuchiya. Aneurysm of lenticulostriate artery in a patient presenting with hemorrhage in the caudate nucleus and lateral ventricle-delayed appearance and spontaneous resolution. 21-Sep-2018;9:192
How to cite this URL: Motohiro Nomura, Eiichi Baba, Kazutaka Shirokane, Atsushi Tsuchiya. Aneurysm of lenticulostriate artery in a patient presenting with hemorrhage in the caudate nucleus and lateral ventricle-delayed appearance and spontaneous resolution. 21-Sep-2018;9:192. Available from: http://surgicalneurologyint.com/surgicalint-articles/9017/
Abstract
Background:An aneurysm of distal lenticulostriate artery is very rare. The natural course and management of this rare aneurysm are not clear.
Case Description:An 81-year-old woman developed consciousness disturbance. Computed tomography revealed hemorrhage in the right caudate nucleus and lateral ventricles. Three-dimensional computed tomographic angiography demonstrated only an aneurysm at the basilar artery. On angiography, on the sixth day, an aneurysm at the right lenticulostriate artery was demonstrated. Then, the aneurysm disappeared on three-dimensional computed tomographic angiography on the 15th day. Subsequent radiological examinations revealed no vascular anomaly in the right lenticulostriate artery.
Conclusion:An aneurysm at this location can show dynamic changes based on radiological findings. Close radiological observation is necessary.
Keywords: Cerebral aneurysm, delayed appearance, lenticulostriate artery, ruptured, spontaneous obstruction
INTRODUCTION
An aneurysm originating from the distal lenticulostriate artery is very rare, and it is difficult to treat by direct surgery or endovascular embolization due to its location.[
CASE REPORT
An 81-year-old woman suddenly developed consciousness disturbance. She was brought to our hospital by ambulance. Computed tomography (CT) revealed hemorrhage in the right caudate nucleus and ventricles, and hydrocephalus [
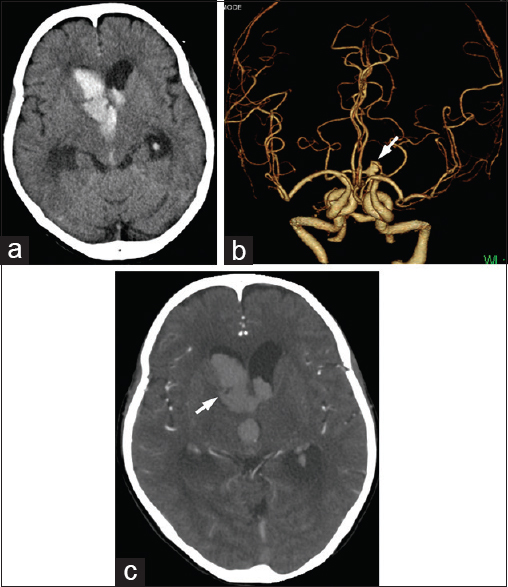
Figure 1
(a) Computed tomography demonstrating hemorrhage in the right caudate nucleus with ventricular rupture. (b) Three-dimensional computed tomographic angiography demonstrating an aneurysm only on basilar artery (arrow). (c) A raw image of three-dimensional computed tomographic angiography on admission showing no abnormal enhancement adjacent to the hematoma. A small low-density area is observed in the hematoma (arrow)
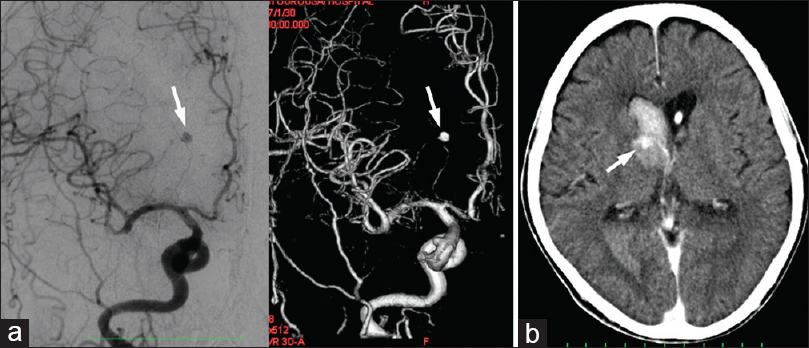
Figure 2
(a) Angiography performed on the sixth day showing an aneurysm originating from the right lenticulostriate artery (arrow). (b) Computed tomography after angiography showing an enhanced lesion in the hematoma (arrow). This portion appears identical to the low-density area indicated in Figure
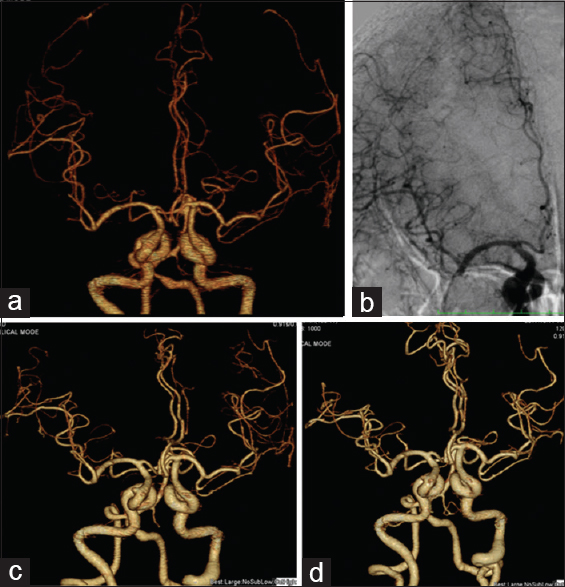
Figure 3
Three-dimensional computed tomographic angiography on the 15th (a) and angiography on the 23rd (b) day showing no aneurysm on the right lenticulostriate artery. (c) Three-dimensional computed tomographic angiography on the 42nd day also showing no lenticulostriate artery aneurysm. (d) Three-dimensional computed tomographic angiography at the 9th month showing no aneurysm on the right lenticulostriate artery
DISCUSSION
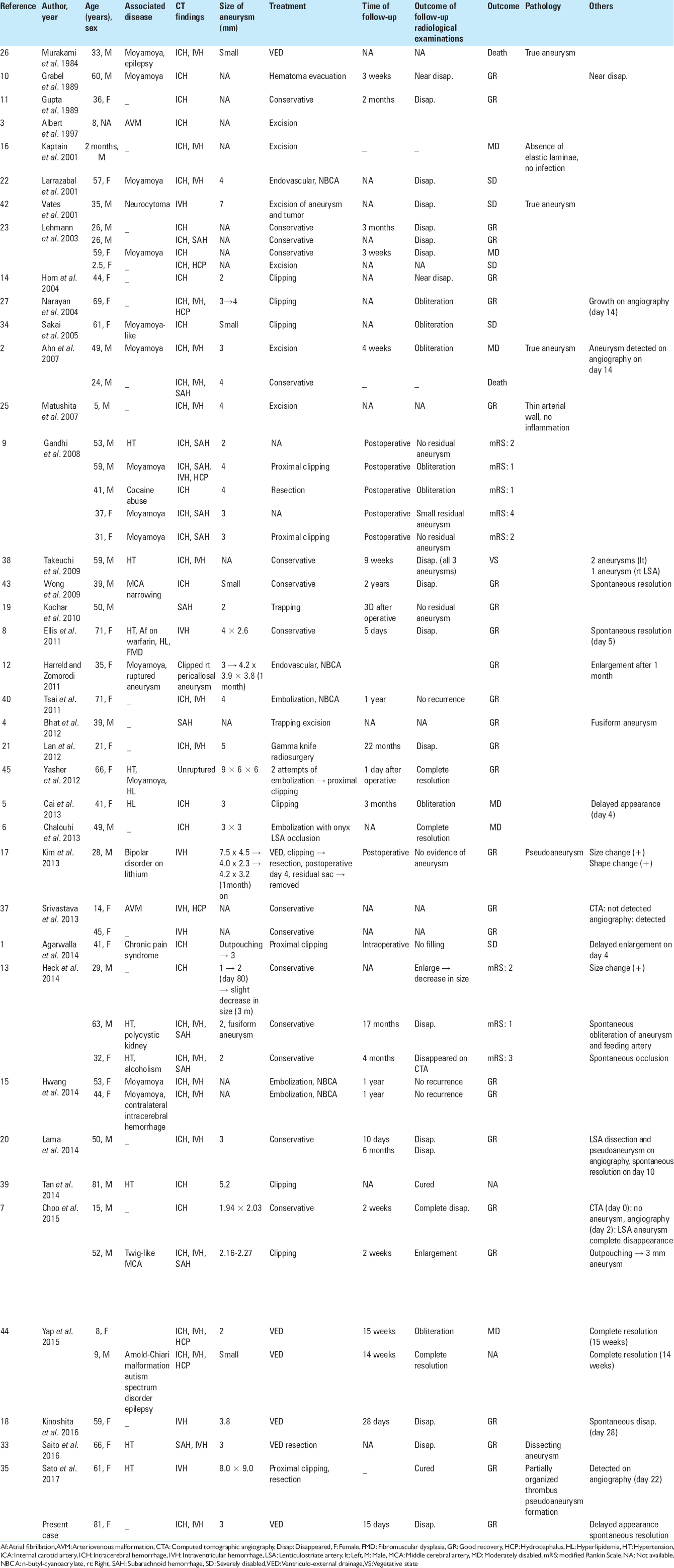
An aneurysm arising from the distal lenticulostriate artery is very rare. The natural course and management of an aneurysm on the distal lenticulostriate artery have not been fully clarified. To our knowledge, 62 cases have been reported in the literature.[
Regarding the natural course of the aneurysm on the distal lenticulostriate artery, there have been several reports describing the spontaneous disappearance of the lesion. Nearly half of the reported cases showed obstruction in their natural courses. Seventeen cases showed spontaneous disappearance or near disappearance in 20 cases of lenticulostriate artery aneurysms which were not radically treated [
This aneurysm may be a dissection or pseudoaneurysm rather than a saccular aneurysm on a main artery in other locations.[
If the aneurysm is not obstructed, the lesion is still associated with a risk of rerupture. In such a case, radical treatment should be considered. As for radical treatment, clipping, trapping, or resection was performed in 22 cases, and endovascular embolization in 6. For 1 case, stereotactic radiosurgery was performed, and the lesion disappeared.[
In our case, initial radiological examination as 3D-CTA on admission failed to demonstrate the lenticulostriate artery aneurysm. Angiography might not be commonly performed for cases with simple hemorrhage in the caudate nucleus, or intraventricular hemorrhage. We performed angiography for the purpose of evaluating a coincidentally developing BA aneurysm. As a result, the lenticulostriate artery aneurysm was unexpectedly identified. There is a possibility that a distal artery aneurysm such as a lenticulostriate artery aneurysm exists in cases of hemorrhage around the lateral ventricles. In fact, raw images of 3D-CTA obtained on admission showed a small low-density area in the hematoma. It was not clear whether this low-density area represented the obstructed aneurysm. Tan et al.[
CONCLUSION
An aneurysm originating from the lenticulostriate artery is rare. This aneurysm may show a delayed appearance and spontaneous resolution. Therefore, serial radiological examinations are mandatory. Also, radiological examinations focusing on a lenticulostriate artery aneurysm are necessary in cases with hemorrhage around the lateral ventricles, although the incidence is low, even though the hemorrhage is considered to be simple.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was supported by research funds to promote the hospital functions of Japan Organization of Occupational Health and Safety.
Conflicts of interest
There are no conflicts of interest.
References
1. Agarwalla PK, Walcott BP, Dunn IF, Thiex R, Frerichs K, Narang S. Fusiform aneurysms of the lenticulostriate artery. J Clin Neurosci. 2014. 21: 373-7
2. Ahn JY, Cho JH, Lee JW. Distal lenticulostriate artery aneurysm in deep intracerebral haemorrhage. J Neurol Neurosurg Psychiatry. 2007. 78: 1401-3
3. Albert FK, Wirtz CR, Forsting M, Jansen O, Polarz H, Mittermaier G. Image guided excision of a ruptured feeding artery “pedicle aneurysm”associated with an arteriovenous malformation in a child: Case report. Comput Aided Surg. 1997. 2: 5-10
4. Bhat DI, Shukla DP, Somanna S. Subarachnoid hemorrhage from a ruptured proximal lenticulostriate artery aneurysm. Neurol India. 2012. 60: 128-9
5. Cai X, Han S, Feske SK, Chou SH. Pearls and oy-sters: Small but consequential: Intracerebral hemorrhage caused by lenticulostriate artery aneurysm. Neurology. 2013. 80: e89-91
6. Chalouhi N, Tjoumakaris S, Gonzalez LF, Dumont AS, Shah Q, Gordon D. Onyx embolization of a ruptured lenticulostriate artery aneurysm in a patient with moyamoya disease. World Neurosurg. 2013. 80: 436.e7-10
7. Choo YS, Kim YB, Shin YS, Joo JY. Deep intracerebral hemorrhage caused by rupture of distal lenticulostriate artery aneurysm: A Report of two cases and a literature review. J Korean Neurosurg Soc. 2015. 58: 471-5
8. Ellis JA, D'Amico R, Altschul D, Leung R, Connolly ES, Meyers PM. Medial lenticulostriate artery aneurysm presenting with isolated intraventricular hemorrhage. Surg Neurol Int. 2011. 2: 92-
9. Gandhi CD, Gilad R, Patel AB, Haridas A, Bederson JB. Treatment of ruptured lenticulostriate artery aneurysms. J Neurosurg. 2008. 109: 28-37
10. Grabel JC, Levine M, Hollis P, Ragland R. Moyamoya-like disease associated with a lenticulostriate region aneurysm. Case report. J Neurosurg. 1989. 70: 802-3
11. Gupta AK, Rao VR, Mandalam KR, Kumar S, Joseph S, Unni M. Thrombosis of multiple aneurysms of a lateral lenticulostriate artery. An angiographic follow-up. Neuroradiology. 1989. 31: 193-5
12. Harreld JH, Zomorodi AR. Embolization of an unruptured distal lenticulostriate aneurysm associated with moyamoya disease. AJNR Am J Neuroradiol. 2011. 32: E42-3
13. Heck O, Anxionnat R, Lacour JC, Derelie AL, Ducrocq X, Richhard S. Rupture of lenticulostriate artery aneurysms. J Neurosurg. 2014. 120: 426-33
14. Horn EM, Zabramski JM, Feiz-Erfan I, Lanzino G, McDougall CG. Distal lenticulostriate artery aneurysm rupture presenting as intraparenchymal hemorrhage: Case report. Neurosurgery. 2004. 55: 708-
15. Hwang K, Hwang G, Kwon OK. Endovascular embolization of a ruptured distal lenticulostriate artery aneurysm in patients with moyamoya disease. J Korean Neurosurg Soc. 2014. 56: 492-5
16. Kaptain GJ, Sheehan JP, Kassell NF. Lenticulostriate artery aneurysm in infancy. Case illustration. J Neurosurg. 2001. 94: 538-
17. Kim T, Bang JS, Hwang G, Kwon OK, Oh CW, Nam KH. Idiopathic lenticulostriate artery pseudoaneurysm protruding into the lateral ventricle: A case report. J Cerebrovasc Endovasc Neurosurg. 2013. 15: 246-50
18. Kinoshita K, Azumi M, Hirai S, Matsushita N, Toi H, Matsubara S. A case of ruptured distal lenticulostriate artery aneurysm presenting with intraventricular hemorrhage. Jpn J Neurosurg (Tokyo). 2016. 25: 252-7
19. Kochar PS, Morrish WF, Hudon ME, Wong JH, Goyal M. Fusiform lenticulostriate artery aneurysm with subarachnoid hemorrhage: The role for super selective angiography in treatment planning. Interv Neuroradiol. 2010. 16: 259-63
20. Lama S, Dolati P, Sutherland GR. Controversy in the management of lenticulostriate artery dissecting aneurysm: A case report and review of the literature. World Neurosurg. 2014. 81: 441.e1-7
21. Lan Z, Li J, You C, Chen J. Successful use of gamma knife surgery in a distal lenticulostriate artery aneurysm intervention. Br J Neurosurg. 2012. 26: 89-90
22. Larrazabal R, Pelz D, Findlay JM. Endovascular treatment of a lenticulostriate artery aneurysm with N-butyl cyanoacrylate. Can J Neurol Sci. 2001. 28: 256-9
23. Lehmann P, Toussaint P, Depriester C, Legars D, Deramond H. Lenticulostriate aneurysms. Radioclinical study. J Neuroradiol. 2003. 30: 115-20
24. Ma N, Tomancok B, Jiang P, Yang XJ, Ojar D, Jia W. Endovascular coiling for a ruptured proximal lenticulostriate artery aneurysm. Chin Med J (Engl). 2016. 129: 606-8
25. Matushita H, Amorim RL, Paiva WS, Cardeal DD, Pinto FC. Idiopathic distal lenticulostriate artery aneurysm in a child. J Neurosurg. 2007. 107: 419-24
26. Murakami H, Mine T, Nakamura T, Aki T, Suzuki K. Intracerebral hemorrhage due to rupture of true aneurysms of the lenticulostriate artery in moyamoya disease. Case report. Neurol Med Chir (Tokyo). 1984. 24: 794-9
27. Narayan P, Workman MJ, Barrow DL. Surgical treatment of a lenticulostriate artery aneurysm. Case report. J Neurosurg. 2004. 100: 340-2
28. Nomura M, Kida S, Uchiyama N, Yamashima T, Yoshikawa J, Yamashita J. Ruptured irregularly shaped aneurysms: Pseudoaneurysm formation in a thrombus located at the ruptured site. J Neurosurg. 2000. 93: 998-1002
29. Nomura M, Mori K, Tamase A, Kamide T, Seki S, Iida Y. Pseudoaneurysm formation due to rupture of intracranial aneurysms: Case series and literature review. Neuroradiol J. 2017. 30: 129-37
30. Nomura M, Tamase A, Kamide T, Mori K, Seki S, Yanagimoto K. Pseudoaneurysm formation in intracerebral hematoma due to ruptured middle cerebral artery aneurysm. Surg J (N Y). 2015. 1: e47-9
31. Oka K, Maehara F, Tomonaga M. Aneurysm of the lenticulostriate artery – Report of four cases. Neurol Med Chir (Tokyo). 1991. 31: 582-5
32. Petrela M, Xhumari A, Azdurian E, Vreto G. Aneurysm of the terminal part of the lenticulostriate artery. Neurochirurgie. 1992. 38: 50-2
33. Saito A, Kon H, Nakamura T, Sasaki T. A dissecting aneurysm of the distal medial lenticulostriate artery: Case report. World Neurosurg. 2016. 89: 725.e1-4
34. Sakai K, Mizumatsu S, Terasaka K, Sugatani H, Higashi T. Surgical treatment of a lenticulostriate artery aneurysm. Case report. Neurol Med Chir (Tokyo). 2005. 45: 574-7
35. Sato Y, Ando K, Kawaguchi M, Kakinuma K. Successful resection of a growing distal medial lenticulostriate artery pseudoaneurysm presenting with isolated intraventricular hemorrhage. J Stroke Cerebrovasc Dis. 2017. 26: e206-9
36. Schürmann K, Brock M, Samii M. Circumscribed hematoma of the lateral ventricle following rupture of an intraventricular saccular arterial aneurysm. Case report. J Neurosurg. 1968. 29: 195-8
37. Srivastava T, Sannegowda RB, Sharma B, Tejwani S. Lenticulostriate artery aneurysm presenting as primary intraventricular haemorrhage. BMJ Case Rep 2013. 2013. p.
38. Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y. Bilateral lenticulostriate artery aneurysms. Br J Neurosurg. 2009. 23: 543-4
39. Tan LA, Kasliwal MK, Johnson AK, Lopes DK. The “Spot sign” secondary to a ruptured lenticulostriate artery aneurysm. Clin Imaging. 2014. 38: 508-9
40. Tsai YH, Wang TC, Weng HH, Wong HF. Embolization of a ruptured lenticulostriate artery aneurysm. J Neuroradiol. 2011. 38: 242-5
41. Vargas J, Walsh K, Turner R, Chaudry I, Turk A, Spiotta A. Lenticulostriate aneurysms: A case series and review of the literature. J Neurointerv Surg. 2015. 7: 194-201
42. Vates GE, Arthur KA, Ojemann SG, Williams F, Lawton MT. A neurocytoma and an associated lenticulostriate artery aneurysm presenting with intraventricular hemorrhage: Case report. Neurosurgery. 2001. 49: 721-5
43. Wong GK, Chou HL, Poon WS, Zhu XL, Yu SC, Ahuja AT. Spontaneous resolution of an aneurysm arising from a penetrating branch of the middle cerebral artery. J Clin Neurosci. 2009. 16: 601-2
44. Yap L, Patankar T, Pysden K, Tyagi A, Goddard T. Spontaneous dissecting lenticulostriate artery aneurysm in children: Radiologic findings and clinical management. J Child Neurol. 2015. 30: 1060-4
45. Yasher M, Kalani MY, Martirosyan NL, Nakaji P, Spetzler RF. Microsurgical clipping of an unruptured lenticulostriate aneurysm. J Clin Neurosci. 2012. 19: 1578-80