- Department of Neurosurgery, Fujita Health University Hospital, Toyoake, Japan
- Department of Diagnostic Radiology, Fujita Health University Hospital, Toyoake, Japan
Correspondence Address:
Joji Inamasu
Department of Diagnostic Radiology, Fujita Health University Hospital, Toyoake, Japan
DOI:10.4103/2152-7806.196765
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Natsuki Hattori, Joji Inamasu, Shunsuke Nakae, Yuichi Hirose, Kazuhiro Murayama. Application of time-spatial labeling inversion pulse magnetic resonance imaging in the diagnosis of spontaneous intracranial hypotension due to high-flow cerebrospinal fluid leakage at C1-2. 26-Dec-2016;7:
How to cite this URL: Natsuki Hattori, Joji Inamasu, Shunsuke Nakae, Yuichi Hirose, Kazuhiro Murayama. Application of time-spatial labeling inversion pulse magnetic resonance imaging in the diagnosis of spontaneous intracranial hypotension due to high-flow cerebrospinal fluid leakage at C1-2. 26-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/application-of-time%e2%80%91spatial-labeling-inversion-pulse-magnetic-resonance-imaging-in-the-diagnosis-of-spontaneous-intracranial-hypotension-due-to-high%e2%80%91flow-cerebrospinal-fluid-leakage-at/
Abstract
Background:Spontaneous intracranial hypotension (SIH) due to cerebrospinal fluid (CSF) leakage at C1-2 poses diagnostic and therapeutic challenges to spine surgeons. Although computed tomography (CT) myelography has been the diagnostic imaging modality of choice for identifying the CSF leakage point, extradural CSF collection at C1-2 on conventional CT myelography or magnetic resonance imaging (MRI) may often be a false localizing sign.
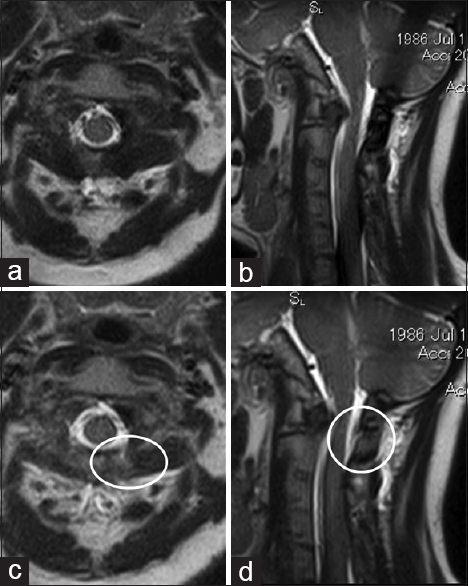
Case Description:The present study reports the successful application of time-spatial labeling inversion pulse (T-SLIP) MRI, which enabled the precise identification of the CSF leakage point at C1-2 in a 28-year-old woman with intractable SIH. After identifying the leakage point using both CT myelography and T-SLIP MRI, surgery was performed to seal the CSF leak. Intraoperatively, a pouch suggestive of an extradural arachnoid cyst around the left C2 nerve root was found, which was repaired by packing the pouch with muscle and fibrin glue. Clinical improvement was observed shortly after surgery, and postoperative imaging revealed the disappearance of the CSF leakage.
Conclusions:T-SLIP MRI may provide useful information on the flow dynamics of CSF in SIH patients due to high-flow leakage. However, further experience is required to assess its sensitivity and specificity as an imaging modality for identifying CSF leakage points.
Keywords: C1-2, cerebrospinal fluid leakage, CT myelography, spontaneous intracranial hypotension, time-spatial labeling inversion pulse (T-SLIP) MRI
INTRODUCTION
Spontaneous intracranial hypotension (SIH) is a syndrome in which hypovolemia of the cerebrospinal fluid (CSF) results in various clinical symptoms.[
CASE REPORT
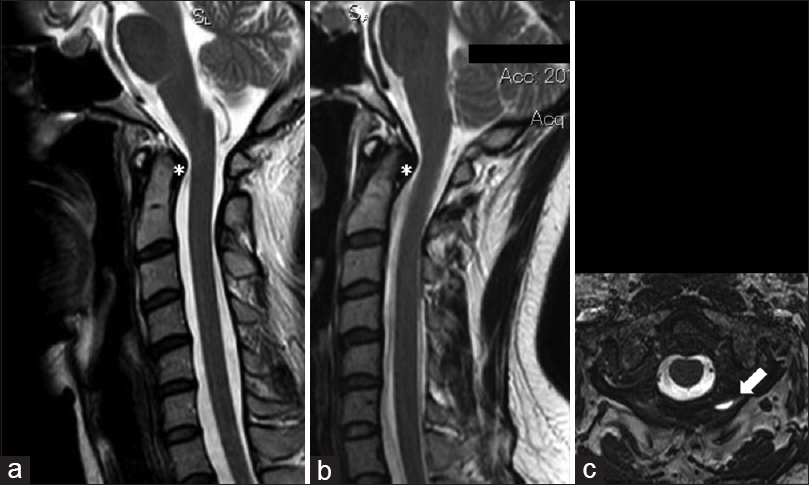
A 28-year-old woman visited our clinic with a complaint of headache, which was aggravated by standing and relieved on lying down. She had been involved in a road traffic accident (RTA) approximately 1 year previously (she was a restrained driver at the time of a rear-end collision). MRI of the cervical spine (T2-weighted sagittal image) obtained shortly after the injury was considered within the normal range [
Figure 1
(a) Magnetic resonance imaging (MRI) of the cervical spine (T2-weighted sagittal image) obtained shortly following neck injury, which was considered within the normal range. (b) MRI of the cervical spine (T2-weighted sagittal image) at the time of admission, showing decreased cerebrospinal fluid (CSF) space. The increase in the thickness of the retro-odontoid tissue was also noted (asterisk). (c) Heavily T2-weighted MRI showing the accumulation of extradural CSF in the paraspinal tissue at C1-2 (arrow)
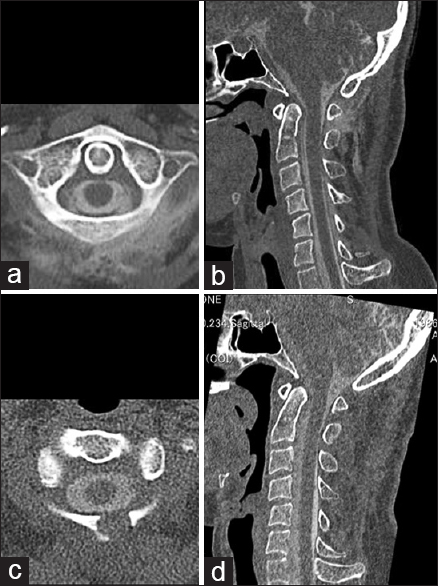
To identify the CSF leakage point in the spinal dura, CT myelography was performed. There was no spontaneous CSF outflow following spinal needle insertion, indicating negative CSF pressure. A CT myelogram, obtained 1 hour following the intrathecal injection of contrast material, revealed a massive CSF leakage at C1-2 [Figure
DISCUSSION
Although SIH due to CSF leakage at C1-2 is less frequent than leakage occurring in the lower cervical or thoracolumbar spine,[
With regard to therapeutics, there has been no consensus on the treatment algorithm for patients with CSF leakage at C1-2 who do not respond to conservative management. The use of conventional blood patch therapy administered from the lower lumbar spine may not be effective,[
There are several limitations to the present case report. First, no data have been previously reported on the sensitivity/specificity of T-SLIP MRI for identifying the CSF leakage point in SIH patients. Low-flow CSF leakage may not be detectable with T-SLIP MRI; therefore, the examination may have low sensitivity and high specificity. Further, clinical experience will be required to make such a conclusion. Second, unlike dynamic CT myelography or digital subtraction myelography, T-SLIP MRI is not a real-time imaging modality, and at present, it can only be performed using MRI equipped with specific software.[
Financial support and sponsorship
Nil.
Conflicts of interest
On behalf of all authors, the corresponding author declares no conflict of interest.
References
1. Cohen-Gadol AA, Mokri B, Piepgras DG, Meyer FB, Atkinson JL. Surgical anatomy of dural defects in spontaneous spinal cerebrospinal fluid leaks. Neurosurgery. 2006. 58: 238-45
2. Inamasu J, Guiot BH. Intracranial hypotension with spinal pathology. Spine J. 2006. 6: 591-9
3. Inamasu J, Nakamura Y, Orii M, Saito R, Kuroshima Y, Mayanagi K, Ichikizaki K, Doi H. Treatment of spontaneous intracranial hypotension secondary to C-2 meningeal cyst by surgical packing: Case report. Neurol Med Chir. 2004. 44: 326-30
4. Inamasu J, Nakatsukasa M. Blood patch for spontaneous intracranial hypotension caused by cerebrospinal fluid leak at C1-2. Clin Neurol Neurosurg. 2007. 109: 716-9
5. Ishibe T, Senzoku F, Kamba Y, Ikeda N, Mikawa Y. Time-spatial labeling inversion pulse magnetic rresonance imaging of cystic lesions of the spinal cord. World Neurosurg. 2016. 88: 693.e13-21
6. Kranz PG, Luetmer PH, Diehn FE, Amrhein TJ, Tanpitukpongse TP, Gray L. Myelographic Techniques for the Detection of Spinal CSF Leaks in Spontaneous Intracranial Hypotension. AJR Am J Roentgenol. 2016. 206: 8-19
7. Kuramae T, Inamasu J, Nakagawa Y, Nakatsukasa M. Spontaneous intracranial hypotension presenting without orthostatic headache complicated by acute subdural hematoma after drainage for chronic subdural hematoma: Case report. Neurol Med Chir. 2011. 51: 518-21
8. Kwon SY, Kim YS, Han SM. Spontaneous C1-2 cerebrospinal fluid leak treated with a targeted cervical epidural blood patch using a cervical epidural Racz catheter. Pain Physician. 2014. 17: E381-4
9. Luetmer PH, Schwartz KM, Eckel LJ, Hunt CH, Carter RE, Diehn FE. When should I do dynamic CT myelography. Predicting fast spinal CSF leaks in patients with spontaneous intracranial hypotension?. AJNR Am J Neuroradiol. 2012. 33: 690-4
10. Schievink WI, Maya MM, Tourje J. False localizing sign of C1-2 cerebrospinal fluid leak in spontaneous intracranial hypotension. J Neurosurg. 2004. 100: 639-44
11. Sykes KT, Yi X. Intracranial hypotension headache caused by a massive cerebrospinal fluid leak successfully treated with a targeted C2 epidural blood patch: A case report. Pain Physician. 2013. 16: 399-404
12. Takeuchi K, Ono A, Hashiguchi Y, Misawa H, Takahata T, Teramoto A, Nakahara S. Visualization of cerebrospinal fluid flow in syringomyelia through noninvasive magnetic resonance imaging with a time-spatial labeling inversion pulse (Time-SLIP). J Spinal Cord Med. 2016. p. 1-4
13. Thielen KR, Sillery JC, Morris JM, Hoxworth JM, Diehn FE, Wald JT. Ultrafast dynamic computed tomography myelography for the precise identification of high-flow cerebrospinal fluid leaks caused by spiculated spinal osteophytes. J Neurosurg Spine. 2015. 22: 324-31
14. Urbach H. Intracranial hypotension: Clinical presentation, imaging findings, and imaging-guided therapy. Curr Opin Neurol. 2014. 27: 414-24
15. Verdoorn JT, Luetmer PH, Carr CM, Lane JI, Lehman VT, Morris JM. Predicting high-flow spinal CSF leaks in spontaneous intracranial hypotension using a spinal MRI-based algorithm: Have repeat CT myelograms been reduced?. AJNR Am J Neuroradiol. 2016. 37: 185-8
16. Walker DG. Refractory headache due to spontaneous intracranial hypotension from a CSF leak at C1-2. J Clin Neurosci. 2003. 10: 482-5
17. Yamada S, Tsuchiya K, Bradley WG, Law M, Winkler ML, Borzage MT. Current and emerging MR imaging techniques for the diagnosis and management of CSF flow disorders: A review of phase-contrast and time-spatial labeling inversion pulse. AJNR Am J Neuroradiol. 2015. 36: 623-30
18. Yoshida H, Takai K, Taniguchi M. Leakage detection on CT myelography for targeted epidural blood patch in spontaneous cerebrospinal fluid leaks: Calcified or ossified spinal lesions ventral to the thecal sac. J Neurosurg Spine. 2014. 21: 432-41
19. Yousry I, Förderreuther S, Moriggl B, Holtmannspötter M, Naidich TP, Straube A. Cervical MR imaging in postural headache: MR signs and pathophysiological implications. AJNR Am J Neuroradiol. 2001. 22: 1239-50