- Division of Neurosurgery.Institute of Medical Research A.Lanari, University of Buenos Aires (UBA), Buenos Aires, Argentina
- Argentine Association of Neurosurgery (AANC), Buenos Aires, Argentina
- Section of Neuro Oncology, Argentine Society of Cancer (SAC), Buenos Aires, Argentina
- Public Health Department, University of Buenos Aires (UBA), Buenos Aires, Argentina
DOI:10.4103/sni.sni_497_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alejandra T. Rabadán, Diego Hernandez, Néstor Vazquez, Rafael Torino, Blanco V. Marcelo, Adhemar Merida. Assessment of accessibility to the diagnosis and treatment of brain tumors in Argentina: Preliminary results. 13-Jun-2017;8:118
How to cite this URL: Alejandra T. Rabadán, Diego Hernandez, Néstor Vazquez, Rafael Torino, Blanco V. Marcelo, Adhemar Merida. Assessment of accessibility to the diagnosis and treatment of brain tumors in Argentina: Preliminary results. 13-Jun-2017;8:118. Available from: http://surgicalneurologyint.com/surgicalint-articles/assessment-of-accessibility-to-the-diagnosis-and-treatment-of-brain-tumors-in-argentina-preliminary-results/
Abstract
Background:As far as public health is concerned, brain tumors burden is significant despite their low incidence, because they comprise high direct costs (specific diagnostic resources, high complexity treatments, and rehabilitation) and high-unforeseen costs (labor leave, family, and social issues). Although the Argentine's Health System is supposed to provide healthcare to all the population, it would not guarantee equity of access for brain tumors treatment. In order to analyze this hypothesis we decided to carry out a survey to obtain data on access, availability and resources for tumor management in Argentina.
Methods:An online questionnaire with eight dimensions and 29 queries was conducted addressing all professionals involved in tumor management. Two variables were generated: (1) type of medical center according to their financial support, and (2) the geographic region (GeoR). Analysis of association between these variables and the accessibility to different resources was performed with Chi-square and Fisher's exact test. Multivariate analyses through multiple logistic regression models were also tested.
Results:One hundred and fourteen surveys were collected from 56 state-managed centers and 55 private/trade-union managed centers. Responders came from 15 provinces grouped into integrated GeoR. Results and analysis of each dimension were reported.
Conclusion:The data obtained provides information about the accessibility to brain tumors treatment, exposing the unequal distribution of human and technologic resources in Argentina. This problem exceeds the limits of public health to become a bioethical problem. We think these results could be essentially associated to our health system fragmented structure, and the large geographical extension of our country. Finally, we believe that collaboration of professional associations working together with public and private sector authorities responsible for financial resources and logistic should bring a principle of solution.
Keywords: Bioethics, brain neoplasm, brain tumor, equity, neurosurgery, oncology, public health, radiotherapy
INTRODUCTION
Brain tumors represent a heterogeneous group of lesions in which brain metastases predominate, followed by primary tumors. The incidence of brain metastases has recently increased due to the substantial development of oncologic therapies. Regarding primary tumors, although their prevalence is low, the most malignant type leads the ranking, being the second cause of death from cancer among people under 35 years old. The predominance of this type of tumors is higher in the sixth and sixth decades of life, and it is estimated that one out of 5000 adults will suffer from a primary brain tumor.
Therapeutic progress is transforming nowadays many of these brain tumors either into chronic processes or that require long treatments. The incidence of these pathologies will presumably increase in the future since the life expectancy of this range of population is outspreading.
As far as public health is concerned, the impact of brain tumors is significant in spite of their low incidence because they comprise high direct costs (specific diagnostic resources, high complexity treatments, and rehabilitation) and high-unforeseen costs (labor leave, family, and social expenditures).[
Three main sectors are involved in Argentina's Health System: Union's health organizations, medical prepaid companies, and state-run (public) health establishments. The latter is divided into municipal, provincial, and federal government management. Although this scheme is supposed to provide healthcare to the entire population, it would not guarantee equal access in cases of low-incidence and high-impact pathologies such as brain tumors.
In order to analyze this hypothesis, we decided to carry out a survey to obtain data on access parameters, resources, and availability in the whole management of this entity.
OBJECTIVE AND GENERAL CHARACTERISTICS
The aim was to build a survey to gather data on the accessibility, availability, and time-to-access to the diagnostic and therapeutic resources necessary for the treatment of brain tumors in Argentina.
MATERIALS AND METHODS
A structured online-based questionnaire of 29 queries was designed comprising all the involved health areas.
It was carried out from 3/6/15 to 4/6/15 with the sponsorship of several professional associations, which enabled the access to the online survey for the specialists involved in the management of brain tumors (mainly neurosurgeons, neuro-oncologists, and radiotherapists). Certain parameters were set up for the construction of the instrument such as conceptual definitions of access, resources, availability, and timing about the entire management of brain tumors. Resources were defined in eight dimensions according to the present requirements for diagnosis and treatment of a brain tumor:
Diagnostic resources
Brain magnetic resonance imaging (MRI) with gadolinium MRI-spectroscopy Functional MRI and tractography Accessibility time periods Intraoperative resources
Microsurgery Neuro-navigation Intraoperative MRI Intraoperative neurophysiology Ultrasonic aspiration Pathology
Specific biomarkers Molecular biology Pathologist experienced in neuropathology Revision of reports on pathology Accessibility time periods Chemotherapy
Chemotherapeutic drugs Specialists in oncology or neuro-oncologists Start-up terms for treatment Radiation treatment
Radiotherapy 3D Radiosurgery Radiotherapy with modulated intensity (RTMI) Radiotherapy start-up terms Psycho-oncology
Resource availability Start-up terms for treatment Palliative care
Access to the resource Access time periods Interdisciplinary team work
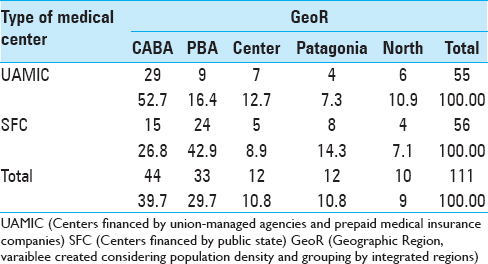
Two variables were created for the analysis, considering the data gathered from the survey. One of them related to the characteristics of the involved centers, and the other to their geographic location. The first variable was called Medical Center Type with two categories: 1) Centers financed by union-managed agencies and prepaid medical insurance companies (UAMIC) and 2) public state financed centers (SFC). The other variable was called geographic region (GeoR) and was created considering population density and grouping by integrated regions. This variable was divided into five categories: Autonomous City of Buenos Aires (ACBA); Buenos Aires province (BAP); central provinces (Santa Fé, Córdoba, Entre Ríos Corrientes); southern provinces (Río Negro, Chubut, Tierra del Fuego, La Pampa and Mendoza); and the northern provinces (Santiago del Estero, Tucumán, Salta, La Rioja, Jujuy).
This classification allowed the analysis of the association between the center types, the geographical distribution, the access to different resources, and the accessibility time periods. A univariate analysis was performed through Chi-square and Fisher's exact test, and logistic regression models were used for multivariate adjusting purposes. A P value <0.05 was considered significant in all tests.
RESULTS
A pilot test was carried out and 114 surveys were gathered from 15 provinces, which were grouped according to integrated GeoR. Fifty-five surveys corresponded to UAMIC, and 56 to SFC [
The following is a description of the obtained results that were specified in each dimension.
Diagnosis imaging
Magnetic resonance imaging
According to the answers, 88.6% of the centers have access to MRI, with 80.7% availability in SFC and 96.5% in UAMIC, with this difference being statistically significant (P: 0.01). Access did not show differences from the statistics point of view according to GeoR (P: 0.822). There was no confounder effect in the multivariate analysis adjusting both variables with the availability of MRI.
Magnetic resonance imaging spectroscopy
51.6% of the centers access the resource. In the case of the SFC, 35.1%; and in the UAMIC 68.4%, being this difference statistically significant (P: < 0.001). Access did not show differences from the statistics point of view according to GeoR (P: 0.173). There was no confounder effect in the multivariate adjusting model.
Functional magnetic resonance imaging and tractography
40.35% of the centers declare to have access, 26.3% in the SFC and 54.3% in the UAMIC, being this difference statistically significant (P: 0.004). The access to functional MRI tests and tractographies showed to be different from the statistical point of view according to GeoR (P: 0.007), showing a greater amount of affirmative answers in the ACBA compared with other regions. There was no interaction or confounder effect in the multivariate analysis adjusting both variables with the availability.
Time to obtain brain imaging tests
70% of the UAMIC get MRIs within 24 hours and 19% within 48 hours. In the SFC it is reduced to 28% for the 24-hour term and to 10% for the 48-hour term, being this difference statistically significant (P: < 0.001).
It should be pointed out that in the SFC, 60% get MRIs in 48 hours and 22.8% in a week's time. The greatest amount of tests obtained rapidly within 24 hours was in the northern and central regions (80% and 75% respectively). There was no confounder effect in the multivariate analysis adjusting both variables with the time terms to get MRIs.
Access within 24-hour for a MRI-spectroscopy was 26% in the UAMIC compared with only 1.75% in SFC, with statistically significant difference (P: < 0.001). The time periods to perform a MRI-spectroscopy were different according to GeoR (P: < 0.001), observing important variations in times in all the regions. There was no confounder effect in the multivariate analysis adjusting both variables with the time terms to perform a MRI-spectroscopy.
The access to functional MRIs and tractographies is obtained within 24 hours only in 17.5% UAMIC. In the SFC it is not possible to get this test in 24 hours, requiring 1 week in 75.4% of the cases to obtain such a study; very significant difference according to the financier involved (P: < 0.001).
Specific surgical resources
Microsurgery
90% of the surveyed access the resource. The difference between the SFC and the UAMIC is not significant (P: 0.2). It does not differ statistically according to the GeoR either (P: 0154). The multivariate analysis did not show confounder effect.
Neuronavigation
51.75% reported to have access. The difference is significant (P: 0.003) between SFC 36.9% and UAMIC 66.7%. Statistically significant differences are also observed among centers according to the GeoR (P: 0.001). The smallest amount of this resource is observed in the southern region and in the BAP. The multivariate analysis did not show confounder effect.
Intraoperative magnetic resonance imaging
It appears to be inaccessible for the 92.3%. The difference between centers, although it is not significant (P: 0.06), shows greater access in the UAMIC 12.3% vs. 1.75% in the SFC. It's inexistent in most of the GeoR; being only available in the ACBA and in the central region. The difference in proportions is not significant (P: 0.19). The multivariate analysis did not show confounder effect.
Intraoperative neurophysiology
Appears to be accessible by 55.3%. The difference between categories is significant (P: 0.008), with better access in the UAMIC 68.4% vs. SFC with 42.1%. Availability varies considerably according to GeoR, being higher in the ACBA and northern region, almost 50% in the BAP and central region and non-existent in the southern area. This difference is significant (P: <0.001). The multivariate analysis did not show confounder effect.
Ultrasonic aspiration
78% accounted to have access, not having differences between centers (P: 0.17); and availability in all the GeoR; with the greatest proportion in the ACBA and northern and central regions. This difference is not significant, though, (P: 0.538). The multivariate analysis did not show confounder effect.
Pathology
Specific biomarkers
79.8% answered that the resource was available. There is statistically significant difference (P: 0.004) between the availability in the UAMIC (91.2%) vs. SFC (68.4%). This difference is remarkable (P: 0.005), and it is available in all the GeoR. When it was adjusted to the variable of coverage, the multivariate model showed that the access to markers in different regions vary in relation with the UAMIC or SFC.
Molecular biology
52.6% answered to have access, with greater proportion in UAMIC (68.4%) vs. SFC (36.8), being this difference statistically significant (P: < 0.001). This resource is available in all of the GeoR, with greater amounts in the ACBA, the PBA, and central region. This difference was not relevant (P: 0.123). The multivariate analysis showed confounder effect when adjusted with the coverage variable, which suggests that this resource differs in relation with the UAMIC or with the SFC.
Pathologist experienced in neuropathology
The access shows a strong difference among groups, being statistically significant (P: <0.001). There's a greater proportion in UAMIC (71.9%) vs. SFC (29.8%). Availability is prevalent in the ACBA and lesser in the rest of the GeoR. This difference is relevant (P: 0.001) in the univariate analysis. The logistic regression model showed confounder effect when adjusted with the coverage variable, which suggests that this resource varies in relation with the UAMIC or SFC.
Review of pathologic reports
The possibility of revision is high (82.5%), although the difference between the UAMIC (91.2%) vs. SFC (73.7%) is statistically significant (P: 0.025). This resource is available in all the regions with a lesser proportion in the southern area. These differences are statistically relevant (P: 0.02) in the univariate analysis. The logistic regression model showed confounder effect when adjusted to the coverage variable, which suggests that this resource varies according to the center types.
Chemotherapy
Chemotherapeutic drugs
95.6% reported availability of the resource. There were no relevant differences between groups (94.7% vs. 96.6%); P: 0.625 in the univariate analysis and the multivariate did not show confounder effect.
Specialists in oncology or neuro-oncologists
The access reaches 96.5%, without significant differences between groups both in the univariate and multivariate analysis.
Treatment start-up time
72.8% reported adequate terms. There were statistically significant differences between UAMIC 86% vs. SFC 59.6% (P: 0.003). The time periods for the start-up treatment with chemotherapy were adequate in all the GeoR. There are no significant differences in the univariate analysis (P: 0374). The multivariate analysis showed confounder effect when adjusted to the coverage variable suggesting that the start-up time depends on the type of center involved.
Radiation treatment
Three-dimensional radiotherapy
68.4% of availability was reported. There were no relevant differences between groups (77.2% vs. 59.7%; P: 0.069). There are no significant differences in the univariate analysis (P: 0294). The multivariate model, did not show confounder effect when adjusted to the coverage variable suggesting that access to radiotherapy 3D does not vary according to the type of center.
Radiosurgery
52% have access. The difference between groups is significant (P: <0.001), 70% in the UAMIC vs. 35% in the SFC. Radiosurgery is not available in all the GeoR in the same proportion. The differences are statistically significant (P: 0.002) in the univariate analysis. The multivariate model did not show confounder effect when adjusted to the coverage variable, which indicates that access to radiotherapy does not vary according to center category.
Radiotherapy with modulated intensity
Access was observed in 41.2% with significant difference (P: 0.002) between UAMIC 52.6% vs. SFC 29.8%. The treatment of RTMI is not available in identical proportions in all of the regions. The differences however, are not statistically significant (P: 0296) in the univariate analysis. The multivariate model did not show confounder effect when adjusted to the coverage variable indicating that access to RTMI does not vary according to the center category.
Radiotherapy start-up terms
51.8% considered the start-up term adequate. There are significant differences (P: 0.003) with a bigger proportion in the UAMIC 66.7% vs. the SFC 36.8%. The treatment start-up varies according to GeoR. The differences are not statistically relevant (P: 0.122) in the univariate analysis. The multivariate model showed confounder effect when adjusted to the coverage variable of, which suggests that the start-up time for radiation treatment differs according to the type of centers involved.
Psycho-oncology
Resource availability
The reported availability is 49.1%. There are significant differences (UAMIC 59.6% vs. SFC 38.6% - P: 0.039). It is not available in the same proportion in all of the regions. The differences are not statistically relevant (P: 0.263) in the univariate analysis. The multivariate model did not show confounder effect, which suggests that the access to specialists in oncology does not vary according to financer.
Treatment start-up terms
46.5% stated that the start-up terms for treatment seemed adequate. There are significant differences (P: 0.024), with more affirmative answers in the UAMIC 57.9% vs. the SFC 35.1%. The time for the treatment start-up is not the same in all the regions. The differences are not statistically relevant in the univariate analysis (P: 0107). The multivariate analysis did not show confounder effect when adjusted to the variable of coverage.
Palliative care
Resource accessibility
75.4% reported to have access to specialists. There is no significant difference between the type of center (P: 0.127). The differences are not statistically relevant (P: 0.998) in the univariate analysis. The multivariate test did not show confounder effect, which implies that access to palliative care does not vary according to the financing agency.
Access time terms
64% stated that the treatment start-up time seemed adequate. There are significant differences (P: 019) between groups, with a bigger proportion of affirmative answers in the UAMIC 75.4% vs. SFC 52.6%. The start-up time for palliative care is adequate in all the regions. The differences in the univariate analysis are not statistically significant (P: 0.704). The univariate analysis did not show confounder effect when adjusted to the coverage variable that implies that the palliative care start-up time does not vary according to the center type involved.
Interdisciplinary teamwork
71% reported to count on teamwork approach, although the differences between groups are very notorious (P: <0.001) when compared: UAMIC 87.7% vs. SFC 54.4% in all the regions.
DISCUSSION
Brain tumor management represents a great effort for the committed professionals, whose foremost goal is to obtain satisfactory results and give patients a better quality of life.[
The pathological analysis is essential to define the adequate oncologic treatment.[
Regarding chemotherapy, the access to drugs seems to be adequate, but the treatment start-up process differs according to centers. We think that giving visibility to this problem could help to improve the situation. On the other hand, the most critical issue goes on getting conclusive pathology without which everything else is inadequate.
3D radiotherapy is accessible by 70% throughout the country with low availability in the northern area, and the time terms have big differences between the public and the private sectors in all the regions. The availability of radiosurgery and RTMI is low. Summing up, access to radiotherapy for tumors that require it, is insufficient and the time terms are affected according to the financer involved.
It is observed that the resources of palliative care, psycho-oncology and teamwork do exist but the access differs according to the type of financing agency. We would like to point out that the results obtained in these three items depend exclusively on the human resource without requirements of specific equipment.
When it comes to the global analysis of the problem of inequity with respect to the access and availability of resources, the inference is that the factors that may be influencing these results are various. First, we believe that there may exist total unawareness of the problem by the Public Health Organizations in charge of the resources management, and secondly we believe that the unidisciplinary approach of brain tumor management is still dominant.[
There are many other subjects to take into account. However, we believe that the current report offers a start point of transformation, because it acknowledges the generation of an observatory that could promote this initiative, strengthen the request to the authorities concerned, and generate future improvement proposals.
As a pilot test, the survey shows results that might be biased and hence subject to future corrections. For that reason, the idea is to reproduce it in new survey instances to broaden the universe of participating professionals and centers in the search for further cooperation.
CONCLUSIONS
The data obtained provide qualitative and quantitative information about the current situation of the accessibility to brain tumor management in Argentina. The main result is the unequal distribution of the human and technological resources that exceeds the limits of public health to become a bioethical concern. The primary causes of this inequality could be the complexity of the fragmented Argentine Health System and the complicated access to resources in such a large country with very irregular population density.
We think solutions should be addressed with the cooperation of all the involved partners, mainly professional associations and the authorities responsible for the financing and logistics of different resources both in the public and private areas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bhangoo SS, Linskey ME, Kalkanis SN. Evidence-based guidelines for the management of brain metastases. American Association of Neurological Surgeons (AANS); Congress of Neurological Surgeons (CNS). Neurosurg Clin N Am. 2011. 22: 97-104
2. Brown TJ, Brennan MC, Li M, Church EW, Brandmeir NJ, Rakszawski KL. Association of the Extent of Resection with Survival in Glioblastoma: A systematic review and Meta-analysis. JAMA Oncol. 2016. p. 16-
3. Cabrera AR, Kirkpatrick JP, Fiveash JB, Shih HA, Koay EJ, Lutz S. Radiation therapy for glioblastoma: Executive summary of an American society for Radiation Oncology Evidence-Based clinical practice Guideline. Pract Radiat Oncol. 2016. 6: 217-25
4. Fouke SJ, Benzinger T, Gibson D, Ryken TC, Kalkanis SN, Olson JJ. The role of imaging in the management of adults with diffuse low grade glioma: A systematic review and evidence-based clinical practice guideline. J Neurooncol. 2015. 125: 457-79
5. Louis DN, Perry A, Burger P, Ellison DW, Reinferberger G, von Deimling A. International Society of Neuropathology-Haarlem consensus guidelines for nervous system tumor classification and grading. Brain Pathol. 2014. 24: 429-35
6. Masui K, Mischel PS, Reifenberger G. Molecular classification of gliomas. Handb Clin Neurol. 2016. 134: 97-120
7. Rabadán A, Diez B, Martínez AM, Antico J, Saidón P, Chistiansen S. Consenso para el Tratamiento de las Metástasis Cerebrales.Capítulo de Neurooncología de la Sociedad Argentina de Cancerología AMA. Revista Argentina de Neurocirugía. 2006. 20: 179-93
8. Rabadán AT, Hernandez D, Eleta M, Pietrani M, Bacanelli M, Christiansen S. Factors related to surgical complications and their impact on the functional status in 236 open surgeries for malignant tumors in a Latinoamerican hospital. Surg Neurol. 2007. 68: 412-20
9. Rabadán AT. Neuroethics scope at a glance. Surg Neurol Int. 2015. 6: 183-
10. Rabadán AT, Hernández D, Vázquez N, Torino R, Blanco Villalba M. Evaluación de la accesibilidad al tratamiento de los tumores cerebrales en Argentina: Resultados preliminares. Rev Argent Neurocir. 2016. 30: 130-5
11. Ragel BT, Ryken TC, Kalkanis SN, Ziu M, Cahill D, Olson JJ. The role of biopsy in the management of patients with presumed diffuse low grade glioma: A systematic review and evidence-based clinical practice guideline. J Neurooncol. 2015. 125: 481-501
12. Weller M, van den Bent M, Hopkins K, Tonn JC, Stupp R, Falini A. EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol. 2014. 15: 395-403
13. Ziu M, Kalkanis SN, Gilbert M, Ryken TC, Olson JJ. The role of initial chemotherapy for the treatment of adults with diffuse low grade glioma: A systematic review and evidence-based clinical practice guideline. J Neurooncol. 2015. 125: 585-607