- Department of Neurosurgery, University of Pisa, AOUP, Pisa, Italy
- Department of Infectious Diseases, Cotugno Hospital, Naples, Italy
- GSpine4, IRCCS Istituto Ortopedico Galeazzi, Milan, Italy
Correspondence Address:
Paolo di Russo
GSpine4, IRCCS Istituto Ortopedico Galeazzi, Milan, Italy
DOI:10.4103/sni.sni_96_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Paolo di Russo, Carlo Tascini, Maria Elena Benini, Carlotta Martini, Paolo Lepori. C1-C2 arthrodesis after spontaneous Propionibacterium acnes spondylodiscitis: Case report and literature analysis. 22-Jan-2018;9:14
How to cite this URL: Paolo di Russo, Carlo Tascini, Maria Elena Benini, Carlotta Martini, Paolo Lepori. C1-C2 arthrodesis after spontaneous Propionibacterium acnes spondylodiscitis: Case report and literature analysis. 22-Jan-2018;9:14. Available from: http://surgicalneurologyint.com/surgicalint-articles/c1%e2%80%91c2-arthrodesis-after-spontaneous-propionibacterium-acnes-spondylodiscitis-case-report-and-literature-analysis/
Abstract
Background:Propionibacterium acnes (P. acnes) is a microaerophilic anaerobic Gram-positive rod responsible for acne vulgaris. Although it is often considered to be a skin contaminant, it may act as a virulent agent in implant-associated infections. Conversely, spontaneous infectious processes have been rarely described.
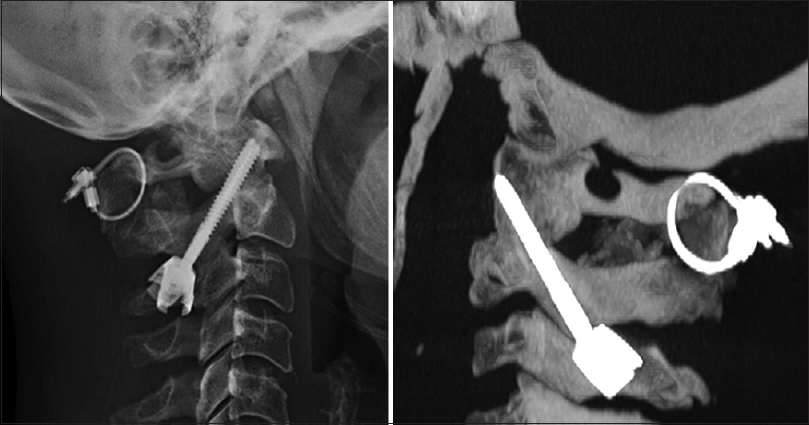
Case Description:Here, we describe a 43-year-old female with C1-C2 spondylodiscitis attributed to P. acnes infection. Despite long-term antibiotic treatment, computed tomography demonstrated erosion of the C1 and C2 vertebral complex that later warranted a fusion. One year postoperatively, the patient was asymptomatic.
Conclusions:Clinical knowledge of P. acnes virulence in spontaneous cervical spondylodiscitis allows early diagnosis, which is necessary to prevent or reduce complications such as cervical deformity with myelopathy or mediastinitis.
Keywords: Atlantoaxial fusion, cervical spinal cord, Propionibacterium acnes, spondylodiscitis
INTRODUCTION
Propionibacterium acnes (P. acnes) is increasingly recognized as a source of musculoskeletal and vertebral infections, particularly associated with the use of spinal instrumentation.[
CASE REPORT
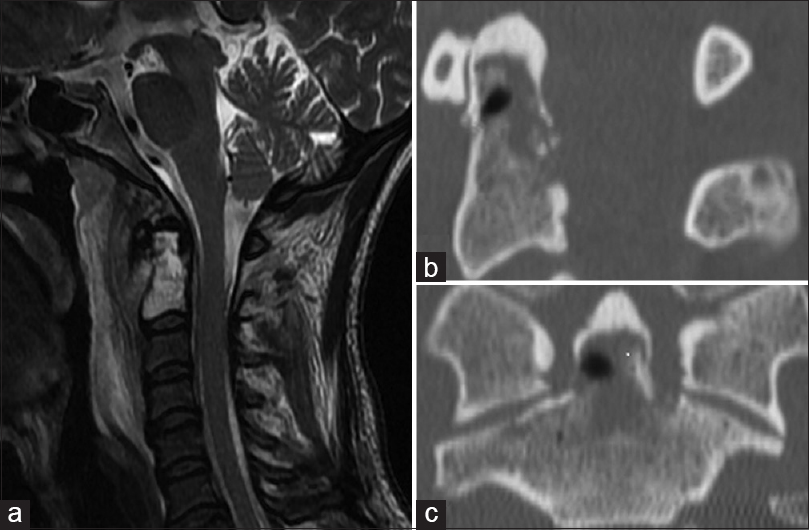
A 43-year-old female had received both local and oral corticosteroid treatment for facial acne 1 month before presenting with neck/pharyngeal pain and progressive dysphagia. Magnetic resonance imaging (MRI) showed a T2-hyperintense signal involving the dens (C2), accompanied by an extensive inflammatory reaction involving the retropharyngeal space [
Biopsy and culture of the C2 lesion
A biopsy was performed of the C1-C2 level through the posterior oral pharynx. Although the histological finding was consistent with inflammation, cultures remained negative (e.g., for common aerobic and anaerobic pathogens). Ten days later, however, the cultures grew P. acnes, sensitive to linezolid. A second confirmatory biopsy confirmed this diagnosis.
Treatment
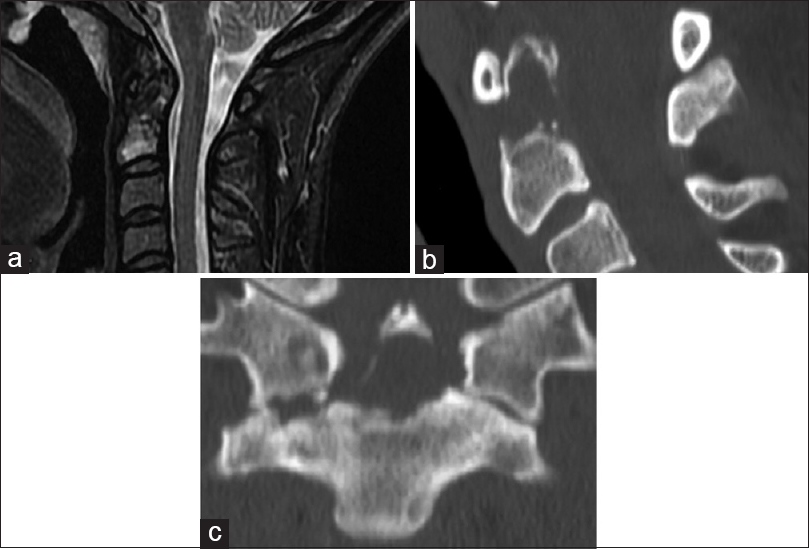
The patient was treated for 20 days with linezolid 600 mg, and was placed in a Halo-vest for atlantoaxial instability. Three months later, although laboratory tests documented resolution of the infection, both the MRI [
DISCUSSION
Several conditions such as diabetes mellitus, immunosuppressive states, intravascular devices, and instrumentation/foreign body implants may result in spontaneous spondylodiscitis.[
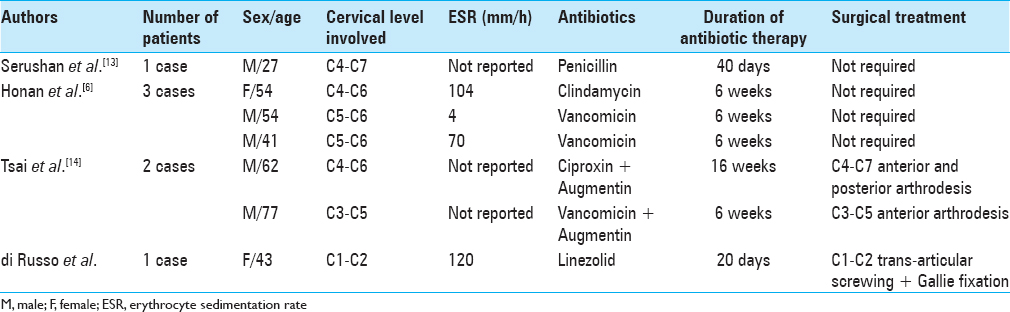
Other cases of cervical spine infections attributed to P. acnes [
CONCLUSIONS
P. acnes may contribute to spontaneous cervical spondylitis in patients with skin lesions. In this and similar cases, a longer incubation period for microbiological cultures is required if P. acnes is suspected as the cause of infection. Early diagnosis is critical to allow for initiation of appropriate antibiotic therapy for preventing subsequent life-threatening complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Brotfain E, Koyfman L, Saidel-Odes L, Borer A, Refaely Y, Klein M. Deep Neck Infection and Descending Mediastinitis as a Complication of Propionibacterium acnes Odontogenic Infection. Case Rep Infect Dis. 2015. 2015: 190134-
2. Carricajo A, Nuti C, Aubet E, Hatem O, Fonsale N, Mallaval FO. Propionibacterium acnes contamination in lumbar disc surgery. J Hosp Infect. 2007. 66: 275-7
3. Hahn F, Zbinden R, Min K. Late implant infections caused by Propionibacterium ances in scoliosis surgery. Eur Spine J. 2005. 14: 783-8
4. Harifi G, Belkhou A, El Bouchti I, Idrissi MO, Idrissi NC, Ousehal A. C1–C2 spondylodiscitis in an adult with SAPHO syndrome: An unusual presentation. Rheumatol Int. 2012. 32: 445-7
5. Harris AE, Hennicke C, Byers K, Welch WC. Postoperative discitis due to Propionibacterium acnes: A case report and review of the literature. Surg Neurol. 2005. 63: 538-41
6. Honan M, White GW, Eisenberg GM. Spontaneous infectious discitis in adults. Am J Med. 1996. 100: 85-9
7. Kapsalaki E, Gatselis N, Stefos A, Makaritsis K, Vassiou A, Fezoulidis I. Spontaneous spondylodiscitis: Presentation, risk factors, diagnosis, management, and outcome. Int J Infect Dis. 2009. 13: 564-9
8. Karadimas EJ, Bunger C, Lindblad BE, Hansen ES, Høy K, Helmig P. Spondylodiscitis. A retrospective study of 163 patients. Acta Orthop. 2008. 79: 650-9
9. McLorinan GC, Glenn JV, McMullan MG, Patrick S. Propionibacterium acnes wound contamination at the time of spinal surgery. Clin Orthop Relat Res. 2005. 437: 67-73
10. Mhaidli HH, Der-Boghossian AH, Haidar RK. Propionibacterium acnes delayed infection following spinal surgery with instrumentation. Musculoskelet Surg. 2013. 97: 85-7
11. Perry AL, Lambert PA. Propionibacterium acnes. Lett Appl Microbiol. 2006. 42: 185-8
12. Portillo ME, Corvec S, Borens O, Trampuz A. Propionibacterium acnes: An Understimated Pathogen in Implant-Associated Infections. Biomed Res Int. 2013. 2013: 804391-
13. Serushan M, Spencer DL, Yeh WL, Kaminski M, Skosey JL. Osteomyelitis of cervical spine from Propionibacterium acnes. Arthritis Rheum. 1982. 25: 346-8
14. Tsai CE, Lee FT, Chang MC, Yu WK, Wang ST, Liu CL. Primary Cervical Osteomyelitis. J Chin Med Assoc. 2013. 76: 640-7
15. Uckay I, Dinh A, Vauthey L, Asseray N, Passuti N, Rottman M. Spondylodiscitis due to Propionibacterium acnes: Report of twenty-nine cases and review of the literature. Clin Microbiol Infect. 2010. 16: 353-8