- Department of Neurological Surgery, Sao Jose Hospital, Santa Casa Hospital Complex, RS, Brazil.
- Department of Neurosurgery, Cristo Redentor Hospital, Porto Alegre, RS, Brazil.
Correspondence Address:
Guilherme Gago
Department of Neurological Surgery, Sao Jose Hospital, Santa Casa Hospital Complex, RS, Brazil.
DOI:10.25259/SNI-121-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Paulo Valdeci Worm, Amauri Dalla-Corte, Albert Vincent Berthier Brasil, Gerson Perondi, Ericson Sfreddo, Antônio Delacy Martini Vial, Guilherme Gago, Pablo Ramon Fruett da Costa. Cerebellar hemorrhage as a complication of spine surgery. 10-May-2019;10:85
How to cite this URL: Paulo Valdeci Worm, Amauri Dalla-Corte, Albert Vincent Berthier Brasil, Gerson Perondi, Ericson Sfreddo, Antônio Delacy Martini Vial, Guilherme Gago, Pablo Ramon Fruett da Costa. Cerebellar hemorrhage as a complication of spine surgery. 10-May-2019;10:85. Available from: http://surgicalneurologyint.com/surgicalint-articles/9341/
Abstract
Background: The association between remote cerebellar hematoma (RCH) and spinal surgery is poorly understood and rarely reported. We present seven cases of RCH after spinal surgery.
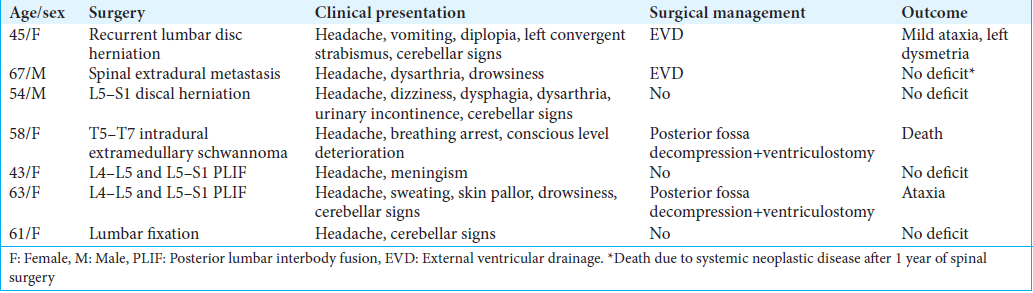
Methods: Seven patients were diagnosed with RCH utilizing computed tomography and/or magnetic resonance, between 2012 and 2016. Their clinical presentations, imaging data, treatment modalities, and outcome were analyzed. There were five females and two males with an average age of 55.8 ± 8.4 years. The age of onset ranged from 43 to 67 years and the time to clinical presentation ranged from 3 h to 5 days. Patients presented with: diplopia/strabismus (one patient), dysphagia/urinary incontinence (one patient), respiratory arrest (one patient), meningismus (one patient), and dysarthria (two patients), along with other symptoms/signs.
Results: Three patients were successfully managed without surgery, two required external ventricular drainage, and two were treated with posterior fossa decompression plus ventriculostomy. Four patients recovered completely, two showed mild residual deficits at discharge, while one expired 7 days postoperatively.
Conclusion: RCH is an uncommon and underdiagnosed complication of spine surgery. It should be suspected when intracranial symptoms occur after spinal procedures.
Keywords: Case report, cerebrospinal fluid leak, remote cerebellar hemorrhage, spinal surgery
INTRODUCTION
“Remote cerebellar hemorrhage” (RCH) is a rare complication of spinal surgery and may have catastrophic consequences. Cevik et al. reported an incidence of 0.08% among 2444 lumbar surgeries.[
Here, we present seven cases of RCH after spine surgery that included an intraoperative dural fistula.
METHODS
Patient population
We retrospectively reviewed the clinical presentation, operative notes, imaging data, treatment modalities, and outcomes of seven patients with intraoperative CSF fistulas resulting in RCH following spinal surgery (2012–2016).
Literature review
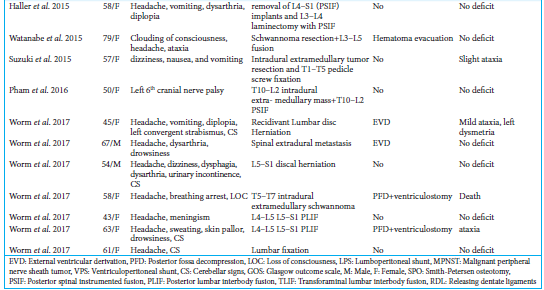
We reviewed the literature regarding RCH after spinal surgery that included a CSF fistula; 65 articles involving 70 patients were analyzed, to which we now add seven cases [
RESULTS
The clinical presentations, operations, operative findings, and outcomes for these seven patients are summarized in
DISCUSSION
RCH is an infrequent complication of spine surgery. RCH more likely occur in patients with intraoperative CSF fistulas (93%) draining large volumes of CSF.[
Chadduck[
Etiology of RCH
The majority of the RCH is attributed to venous hemorrhagic infarction,[
Time of onset of RCH
About 50% of RCH occur 24 h after surgery.[
Clinical findings for patients who develop RCH
Patients ranged in age from the fourth to the sixth decade. Of these, 72% were women. One paper[
Symptoms of RCH
The symptoms of RCH depend on the extent and severity of the RCH. These include uniformly, headache, altered level of consciousness, and cerebellar signs often including dysarthria.[
Outcomes of RCH following CSF fistula during spinal surgery
Outcomes vary due to several factors including extent of bleeding, intracerebellar component, underlying disease, amount of time before action is taken and presence of further complications.[
Nonsurgical versus surgical management
Small hematomas can be managed conservatively,[
CONCLUSION
RCH should be considered in patients who have unexpected neurological deterioration after spinal surgery involving an intraoperative CSF fistula. Early recognition of RCH and confirmation with neuroimaging investigation allows for quick proper management, and better outcomes.
References
1. Bernal-Garcia LM, Cabezudo-Artero JM, Ortega-Martinez M, Fernández-Portales I, Ugarriza-Echebarrieta LF, Pineda-Palomo M. Remote cerebellar hemorrhage after lumbar spinal fluid drainage. Report of two cases and literature review. Neurocirugia (Astur). 2008. 19: 440-5
2. Cevik B, Kirbas I, Cakir B, Akin K, Teksam M. Remote cerebellar hemorrhage after lumbar spinal surgery. Eur J Radiol. 2009. 70: 7-9
3. Chadduck WM. Cerebellar hemorrhage complicating cervical laminectomy. Neurosurg. 1981. 9: 185-9
4. Friedman JA, Ecker RD, Piepgras DG, Duke DA. Cerebellar hemorrhage after spinal surgery: Report of two cases and literature review. Neurosurg. 2002. 50: 1361-3
5. Gobel F, Heidecke V, Hube R, Reichel H, Held A, Hein W. Cerebellar hemorrhage as an early complication of spinal operations. 2. Case reports and review of the literature. Z Orthop Ihre Grenzgeb. 1999. 137: 2-6
6. Karaeminogullari O, Atalay B, Sahin O, Ozalay M, Demirors H, Tuncay C. Remote cerebellar hemorrhage after a spinal surgery complicated by dural tear: Case report and literature review. Neurosurg. 2005. 57: 215-
7. Konya D, Ozgen S, Pamir MN. Cerebellar hemorrhage after spinal surgery: Case report and review of the literature. Eur Spine J. 2006. 15: 95-9
8. Ma X, Zhang Y, Wang T, Li G, Zhang G, Khan H. Acute intracranial hematoma formation following excision of a cervical subdural tumor : A report of two cases and literature review. Br J Neurosurg. 2014. 28: 125-30
9. Sturiale CL, Rossetto M, Ermani M, Baro V, Volpin F, Milanese L. Remote cerebellar hemorrhage after spinal procedures (part 2): A systematic review. Neurosurg Rev. 2016. 39: 369-76
10. Yasargil MG, Yonekawa Y. Results of microsurgical extra-intracranial arterial bypass in the treatment of cerebral ischemia. Neurosurg. 1977. 1: 22-4
11. Yoshida S, Yonekawa Y, Yamashita K, Ihara I, Morooka Y. Cerebellar hemorrhage after supratentorial craniotomy-Report of three cases. Neurol Med Chir (Tokyo). 1990. 30: 738-43