- Department of Neurosurgery, Nanoori Hospital Suwon, Suwon-si, Gyeonggi-do,
- Department of Neurosurgery, Nanoori Hospital Gangseo,
- Department of Neurosurgery, Nanoori Hospital Gangnam, Seoul, South Korea.
Correspondence Address:
Ki Joon Kim
Department of Neurosurgery, Nanoori Hospital Gangnam, Seoul, South Korea.
DOI:10.25259/SNI_431_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ki Joon Kim, Mun Soo Gang, Jung-Sik Bae, Jee Soo Jang, Il-Tae Jang. Cervical instability following artificial disc replacement. 20-Sep-2019;10:183
How to cite this URL: Ki Joon Kim, Mun Soo Gang, Jung-Sik Bae, Jee Soo Jang, Il-Tae Jang. Cervical instability following artificial disc replacement. 20-Sep-2019;10:183. Available from: http://surgicalneurologyint.com/surgicalint-articles/cervical-instability-following-artificial-disc-replacement/
Abstract
Background: Although there has been increased interest in utilizing artificial disc replacement (ADR) techniques to treat cervical degenerative disease, few reports have focused on their postoperative complication and reoperation rates.
Case Description: A 52-year-old male underwent the uneventful placement of a C5-C6 cervical ADR for disc disease and foraminal stenosis. One year later, he experienced the onset of severe neck pain attributed to instability of the ADR construct. This required removal of the C5-6 ADR and subsequent fusion.
Conclusion: Strict adherence to appropriate criteria is critical for choosing when to place a cervical ADR. This requires documenting; adequate surgical indications, careful selection of the appropriate ADR device, meticulous surgical technique, proper preservation of the supporting structures, and sufficient neural decompression.
Keywords: Artificial disc replacement, Cervical instability, Fusion
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is typically utilized to treat degenerative cervical disease but carries an approximately 5% risk of adjacent segment disease. Artificial disc replacement (ADR) was developed to preserve motion and avoid this complication of ACDF.[
CASE DESCRIPTION
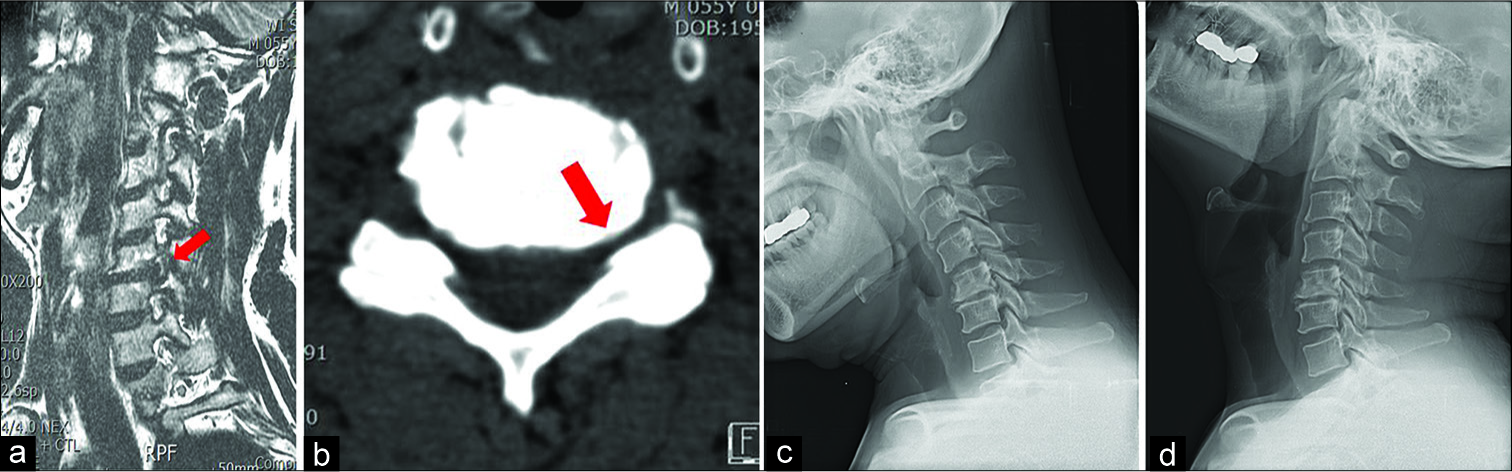
A 52-year-old male underwent an uneventful C5-C6 ADR for an MR documented herniated disc with foraminal stenosis [
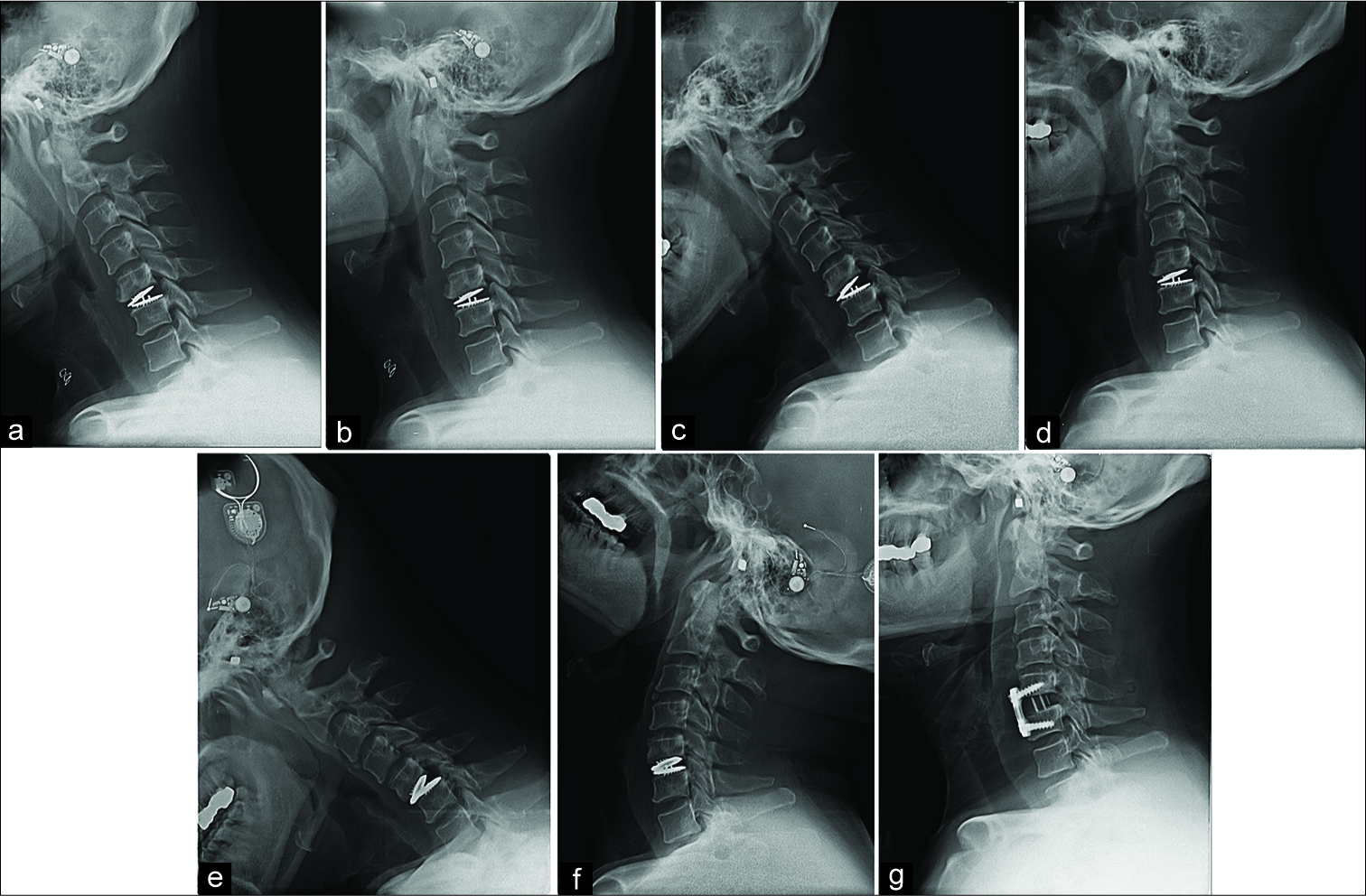
Figure 2:
(a) Postoperative – 1 week, (b) Postoperative – 1 week, (c) Postoperative – 2 months, (d) Postoperative – 2 months, (e) Postoperative – 14 months, (f) Postoperative - 14 months showed an aggravation of cervical instability at C5-6. Cervical instability at C5-6, the ADR site, aggravated in the temporal order of (a-f). (g) Radiograph obtained after a revision operation, in which the ADR implant was removed and ACDF was performed.
DISCUSSION
The success of ADR is attributed to; proper patient selection, operating for the right surgical indications, utilizing meticulous technique, and careful implant device selection.[
CONCLUSION
With the increased use of the ADR, more revision surgery is anticipated. To prevent cervical instability following ADR, one must carefully choose appropriate patients and strictly follow surgical techniques that preserve supporting structures while achieving sufficient neural decompression.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Burkus JK, Haid RW, Traynelis VC, Mummaneni PV. Long-term clinical and radiographic outcomes of cervical disc replacement with the prestige disc: Results from a prospective randomized controlled clinical trial. J Neurosurg Spine. 2010. 13: 308-18
2. Kerferd JW, Abi-Hanna D, Phan K, Rao P, Mobbs RJ. Focal hypermobility observed in cervical arthroplasty with mobi-C. J Spine Surg. 2017. 3: 693-6
3. Kowalczyk I, Lazaro BC, Fink M, Rabin D, Duggal N. Analysis of in vivo kinematics of 3 different cervical devices: Bryan disc, proDisc-C, and prestige LP disc. J Neurosurg Spine. 2011. 15: 630-5
4. Park SB, Kim KJ, Jin YJ, Kim HJ, Jahng TA, Chung CK. X-ray-based kinematic analysis of cervical spine according to prosthesis designs: Analysis of the mobi C, bryan, PCM, and prestige LP. J Spinal Disord Tech. 2015. 28: E291-7
5. Salari B, McAfee PC. Cervical total disk replacement: Complications and avoidance. Orthop Clin North Am. 2012. 43: 97-107
6. Sekhon LH, Ball JR. Artificial cervical disc replacement: Principles, types and techniques. Neurol India. 2005. 53: 445-50
7. Yu CC, Hao DJ, Ma YL, Huang DG, Li HK, Feng H. The role of posterior longitudinal ligament in cervical disc replacement: An ovine cadaveric biomechanical analysis. Med Sci Monit. 2016. 22: 1843-9