- Program in Health Sciences-IAMSPE; Department of Neurosurgery, Hospital Mandaqui, Brazil.
- Department of Neurosurgery, Hospital Mandaqui, Brazil.
- Program in Health Sciences-IAMSPE; Department of Neurosurgery, Hospital Mandaqui and Hospital do Servidor Publico Estadual - HSPE, São Paulo, Brazil.
Correspondence Address:
Ítalo Teles de Oliveira Filho
Program in Health Sciences-IAMSPE; Department of Neurosurgery, Hospital Mandaqui and Hospital do Servidor Publico Estadual - HSPE, São Paulo, Brazil.
DOI:10.25259/SNI_469_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ítalo Teles de Oliveira Filho, Paulo Cesar Romero, Emílio Afonso França Fontoura, Ricardo Vieira Botelho. Chiari malformation and types of basilar invagination with/without syringomyelia. 18-Oct-2019;10:206
How to cite this URL: Ítalo Teles de Oliveira Filho, Paulo Cesar Romero, Emílio Afonso França Fontoura, Ricardo Vieira Botelho. Chiari malformation and types of basilar invagination with/without syringomyelia. 18-Oct-2019;10:206. Available from: http://surgicalneurologyint.com/surgicalint-articles/9714/
Abstract
Background: Craniometric studies document different subtypes of craniocervical junction malformations (CCJM). Here, we identified the different types and global signs and symptoms (SS) that correlated with these malformations while further evaluating the impact of syringomyelia.
Methods: Prospective data concerning SS and types of CCJM were evaluated in 89 patients between September 2002 and April 2014 using Bindal’s scale.
Results: The mean Bindal’s scores of each type of CCJM were Chiari malformation (CM) = 74.6, basilar invagination Type 1 (BI1) = 78.5, and BI Type 2 (BI2) = 78. Swallowing impairment and nystagmus were more frequently present in the BI patients. Symptomatic burdens were higher in patients with syringomyelia and included weakness, extremity numbness, neck pain, dissociated sensory loss, and atrophy.
Conclusion: There were no statistically significant differences in SS between the different CCJM types. BI patients had more swallowing and nystagmus complaints versus CM patients, but there were no significant differences in clinical SS between BI1 and BI2 patients. Notably, those with attendant syringomyelia had a higher SS burden.
Keywords: Arnold–Chiari malformation, Basilar impression, Neurologic manifestations, Platybasia, Signs and symptoms
INTRODUCTION
Chiari malformations (CMs) and basilar invagination (BI – BI1 and BI2) are the most common craniocervical junction malformations (CCJM) seen in adults; both may also be associated with syringomyelia.[
BI1 is associated with craniocervical instability, odontoid insinuation toward the foramen magnum, and often anterior arch of the atlas assimilation.[
METHODS
Study design
This study represented a cross-sectional evaluation of prospectively collected data conducted between September 2002 and April 2014 using Bindal’s scale. All patients filled out informed consent to enter in this study. The research protocol was approved by the research ethics committee (CAAE 32361614.6.0000.5551).
There were 89 consecutive symptomatic patients with CCJM; 46 (52%) had CM, 43 (48%) had BI; among those with BI: 13 (30%) had BI1, and 30 (70%) had BI2. Females represented 57% of the patients with CCJM (51 patients), and they averaged 47.7 years of age (range: 11–77 years). All exhibited varying degrees of SS attributed to neural structure/posterior fossa compression and/or CSF blockage. Syringomyelia was present in 44 (49%) of all CCJM (CM and BI) patients.
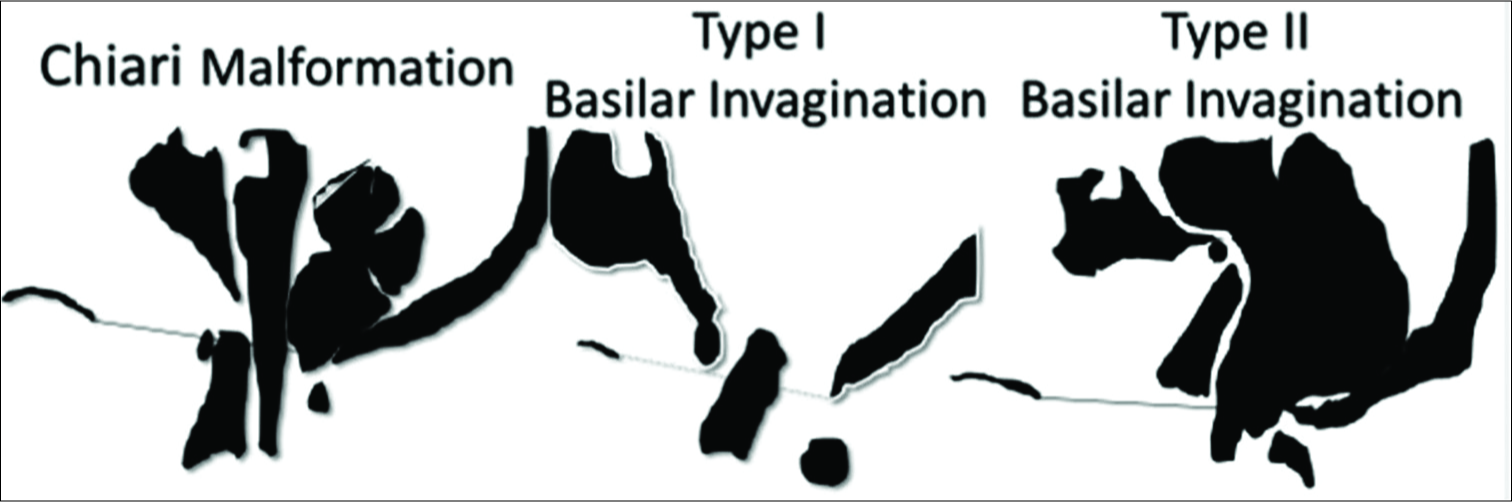
Definitions and diagnostic criteria of CM, B11, and B12 malformations [ Figure 1 ]
CM
Herniation (variable) of the cerebellar tonsils below the foramen magnum results in compression of the tonsils in the cisterna magna without odontoid insinuation toward the skull base.[
BI
BI1: Odontoid insinuation toward the foramen magnum, violating the McRae line, associated with the anterior arch of the atlas assimilation, and craniocervical instability.[
BI2: Odontoid axis process above the Chamberlain line, without violation of the foramen magnum.[
Syringomyelia
Syringomyelia constitutes a fluid accumulation around the spinal cord central canal, identified as intramedullary hypersignals on T2-weighted magnetic resonance imaging (MRI).[
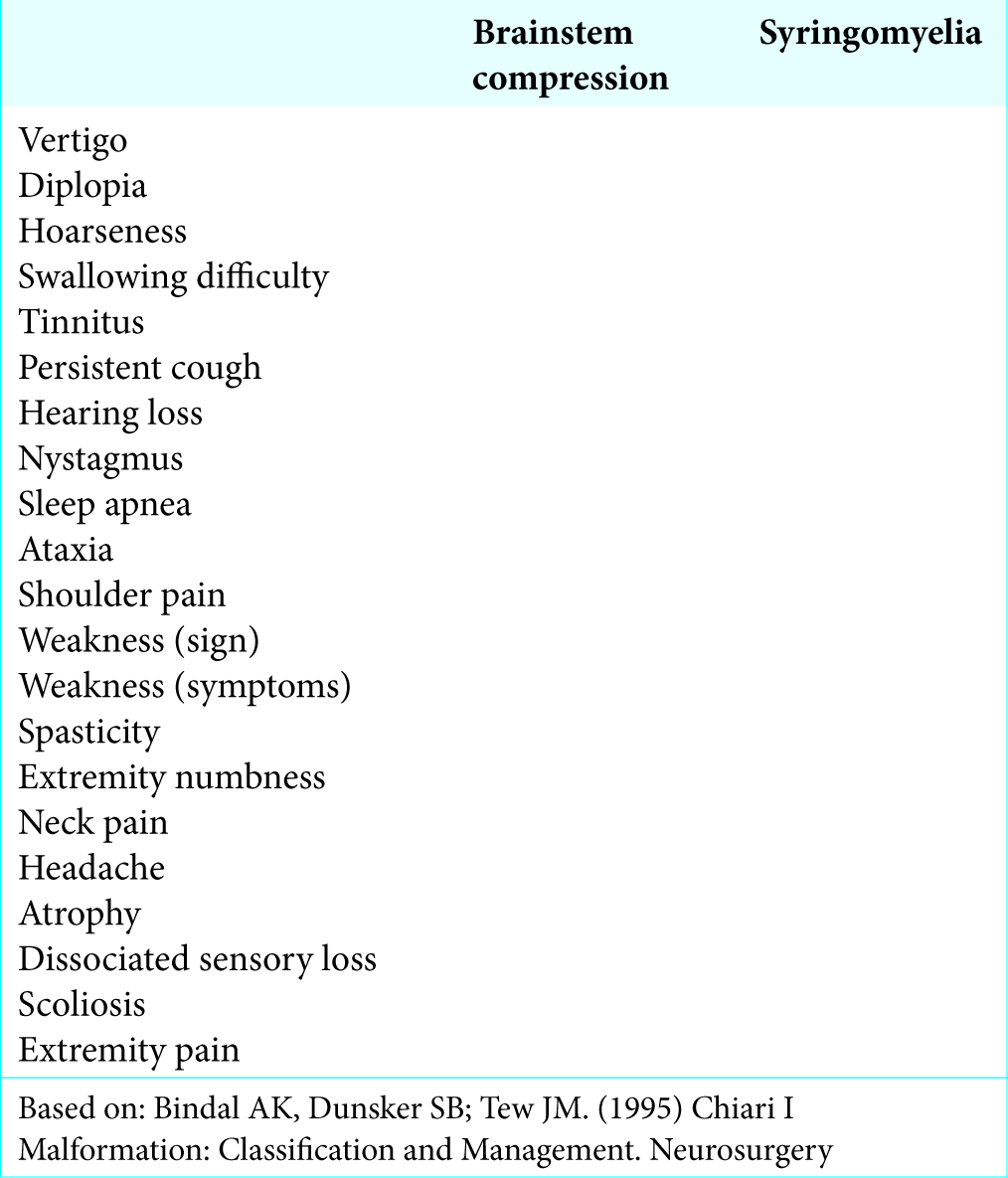
Assessment of SS of CCJM
Bindal’s standardized scale longitudinally evaluated CCJM patients’ clinical manifestations and provided the following score for follow-up comparisons; each sign or symptom received a score of 10, and the score (symptomatic burden) was defined as the sum of the SS presented by the patients [
Statistical evaluation
Bindal’s scores for the three types of malformations were compared using ANOVA (the Kruskal–Wallis test).
SS were described by percentages and were compared between types using the Chi-squared test; this was similarly applied to patients with/without syringomyelia [
RESULTS
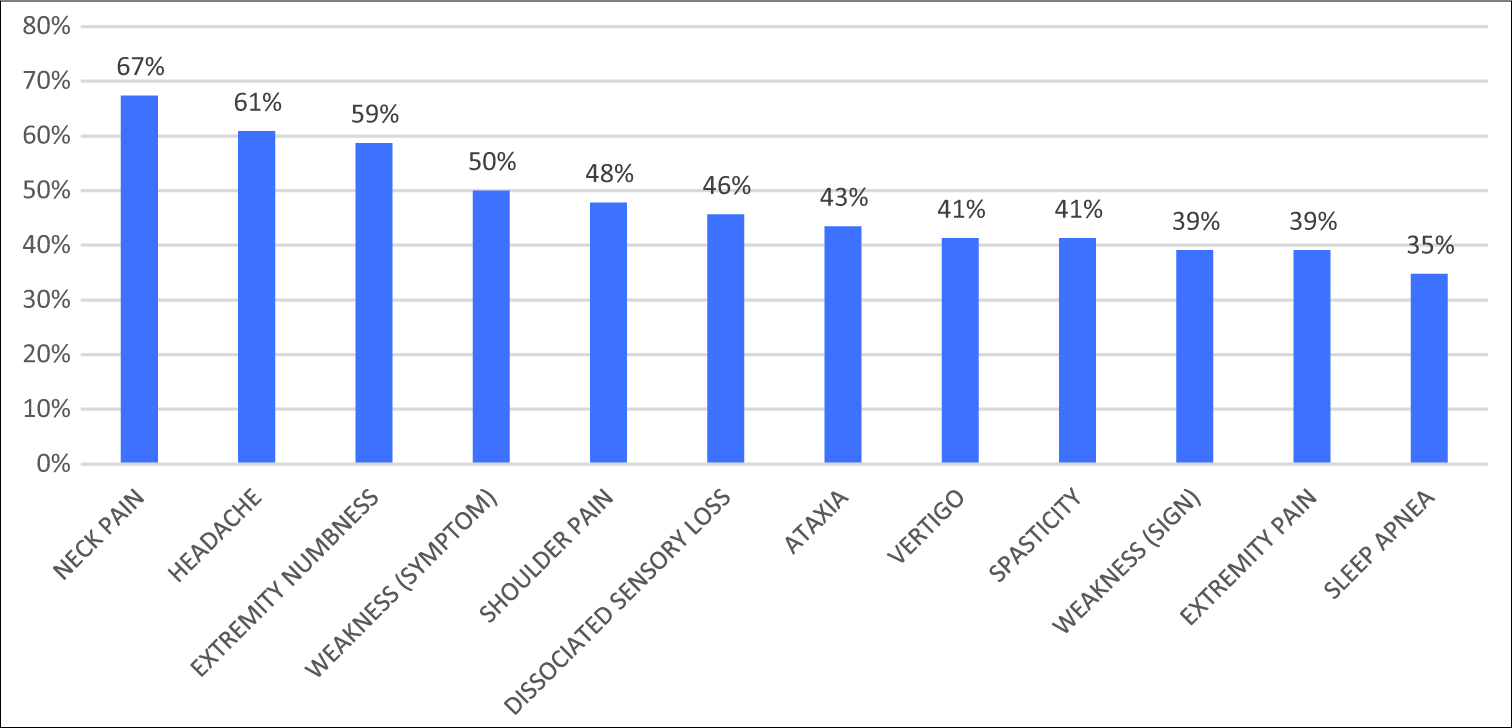
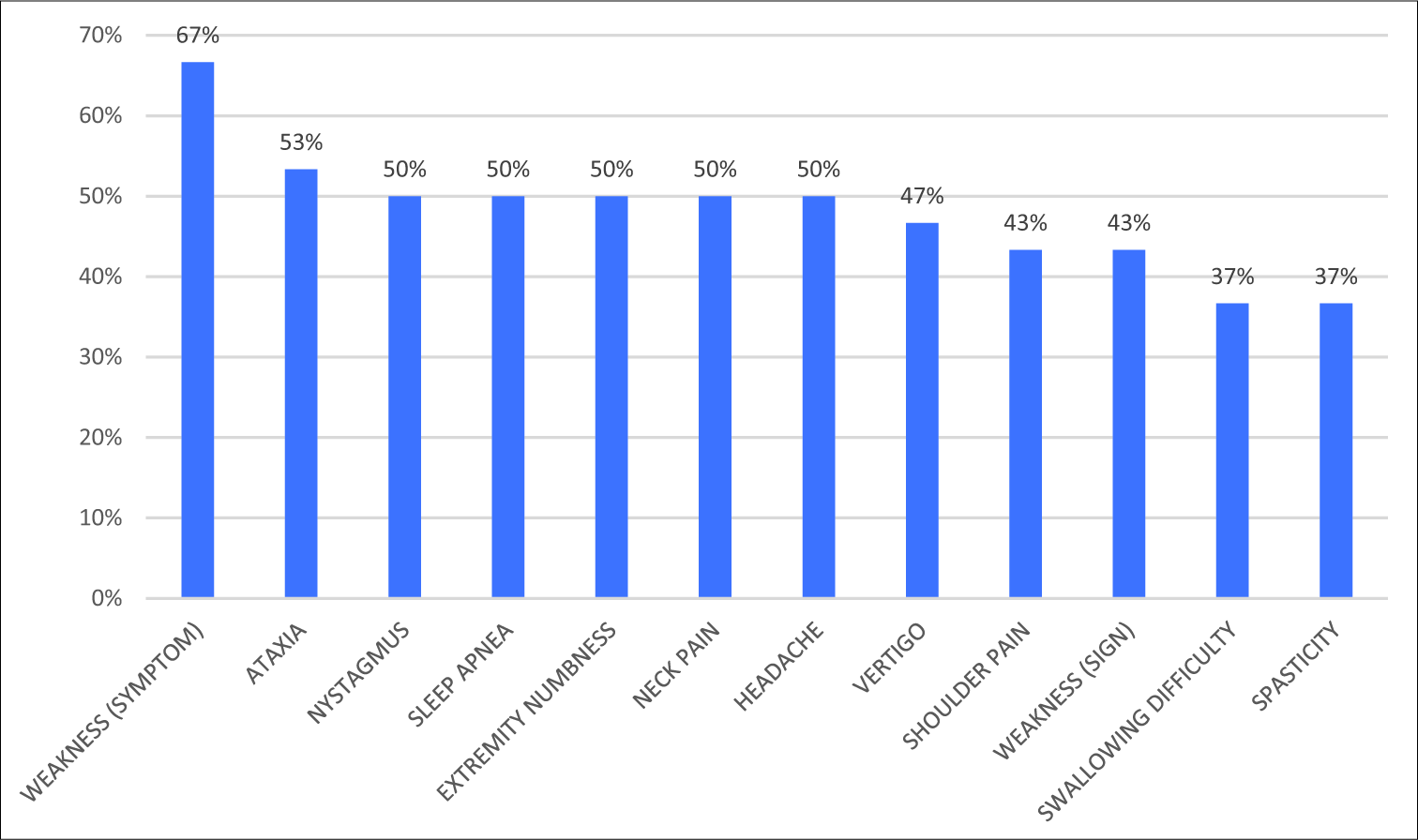
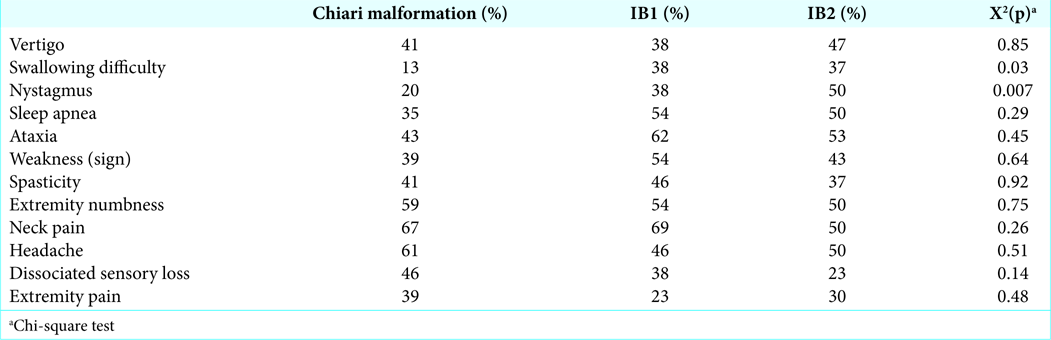
Prevalent SS among three CCJM malformations
Predominant SS for patients with these three malformations (CCJM, B11, and B12) included neck pain, ataxia, numbness, and weakness of the extremities (e.g., with added headaches for CM patients and sleep apnea for BI patients). For CM patients, SS in descending order included neck pain, headache, and numbness of extremities followed by weakness [
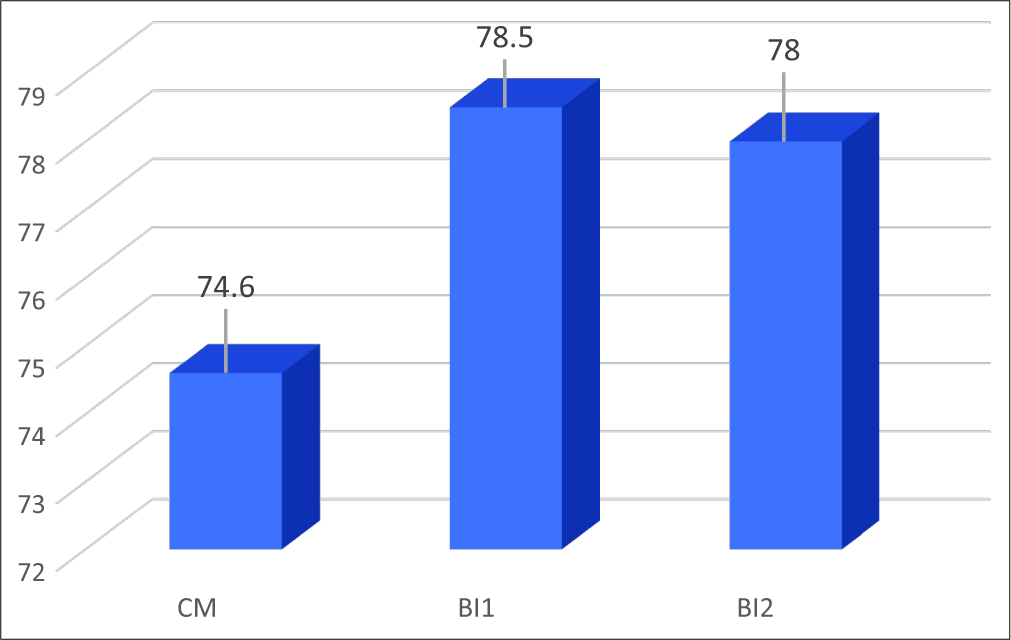
The mean Bindal’s score for each type of CCJM was 74.6 for CM, 78.5 for BI1, and 78 for BI2 (Kruskal–Wallis test, P = 0.9) [
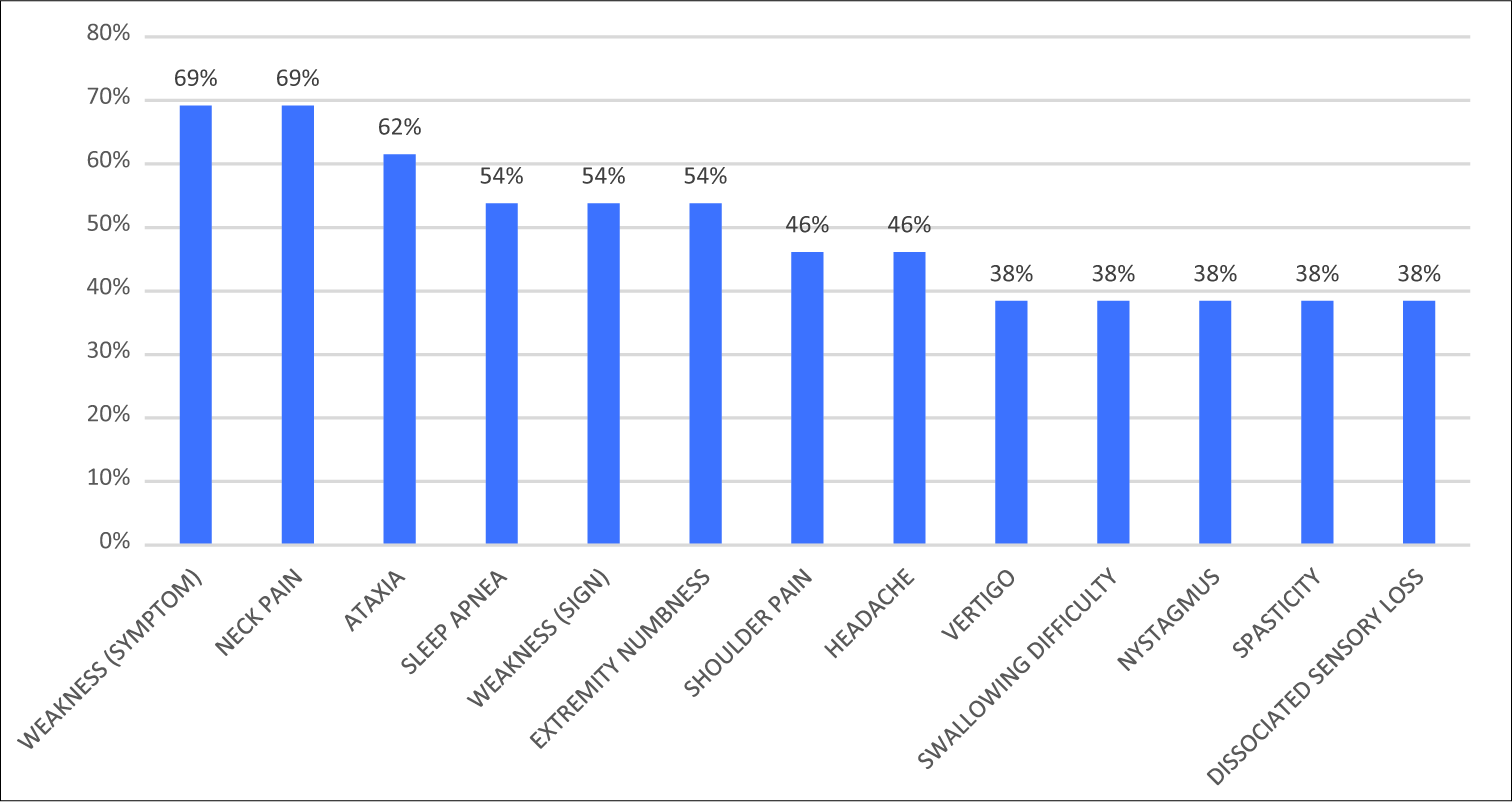
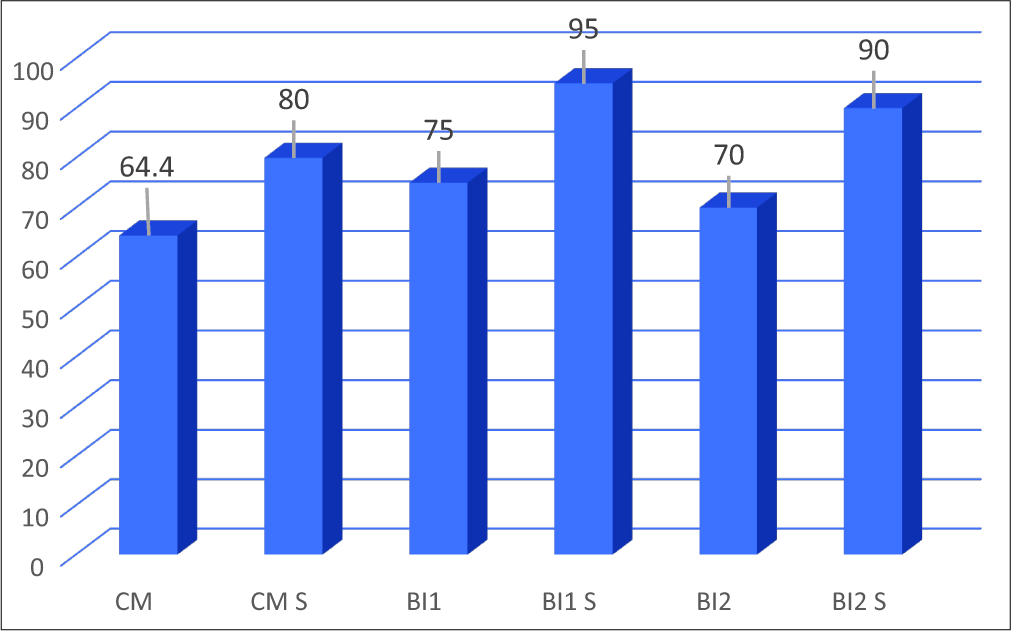
SS for patients with/without syringomyelia
The mean Bindal’s score was 69.3 for the patients without syringomyelia and 83.4 for the syringomyelic patients (Mann–Whitney U-test; P = 0.054) [
DISCUSSION
Our understanding of CCJM (e.g., CM, B11, and B12) has evolved with the introduction of computed tomography, MRI, linear and angular craniometric studies, and genetic and embryological studies.[
Goel showed that the following symptoms were more predominant in BI1 patients: paresthesias (55%), spinothalamic dysfunction (36%), cervicalgia (77%), and torticollis (41%). The study also reported that BI2 physiopathology was the same as for CM, largely attributable to the diminished cranial fossa volume contributing to SS.[
Bindals’ scale
Bindal’s scale was created to quantify SS, and in this study, no differences were found in the SS burden between the three types of CCJM, but SS burdens were uniformly increased in all patients with accompanying syringomyelia.[
CONCLUSION
For the three types of CCJM, swallowing difficulties and nystagmus were more prevalent in BI versus CM, while all CCJM patients with syringomyelia had higher frequencies of weakness, extremity numbness, neck pain, dissociated sensory loss, and atrophy.
References
1. Bindal AK, Dunsker SB, Tew JM. Chiari I malformation: Classification and management. Neurosurgery. 1995. 37: 1069-74
2. Botelho RV, Diniz JM. Basilar Invagination: Cranio-cervical kyphosis rather than prolapse from the upper cervical spine. J Neurol Neuromed. 2017. 2: 15-9
3. Ferreira JA, Botelho RV. The odontoid process invagination in normal subjects, chiari malformation and basilar invagination patients: Pathophysiologic correlations with angular craniometry. Surg Neurol Int. 2015. 6: 118-
4. Goel A. Basilar invagination, chiari malformation, syringomyelia: A review. Neurol India. 2009. 57: 235-46
5. Guerreiro RB, Bittencourt L, Reis RC, Rotta JM, Tufik S, Botelho RV. Upper airway dimensions in patients with craniocervical junction malformations with and without sleep apnea. A pilot case-control study. Arq Neuropsiquiatr. 2015. 73: 336-41
6. Klekamp J. Chiari I malformation with and without basilar invagination: A comparative study. Neurosurg Focus. 2015. 38: E12-
7. Pinter NK, McVige J, Mechtler L. Basilar invagination, basilar impression, and platybasia: Clinical and imaging aspects. Curr Pain Headache Rep. 2016. 20: 49-
8. Shuhui G, Jiagang L, Haifeng C, Hao ZB, Qing HS. Surgical management of adult reducible atlantoaxial dislocation, basilar invagination and chiari malformation with syringomyelia. Turk Neurosurg. 2016. 26: 615-21