- Department of Neurosurgery, Sher-i- Kashmir Institute of Medical Sciences Soura, Srinagar, Jammu and Kashmir, India
- Department of Neuroanesthesiology, Sher-i- Kashmir Institute of Medical Sciences Soura, Srinagar, Jammu and Kashmir, India
Correspondence Address:
Abrar A. Wani
Department of Neurosurgery, Sher-i- Kashmir Institute of Medical Sciences Soura, Srinagar, Jammu and Kashmir, India
DOI:10.4103/sni.sni_340_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Humam Tanki, Abrar A. Wani, Altaf U. Ramzan, Nayl K. Malik, Sarbjit S. Chhibber, Bashir A. Dar, Sajad Arif, Zulfiqar Ali, M. Masood Laherwal. Conservative management of craniovertebral junction injuries: Still a good option. 05-Apr-2017;8:43
How to cite this URL: Humam Tanki, Abrar A. Wani, Altaf U. Ramzan, Nayl K. Malik, Sarbjit S. Chhibber, Bashir A. Dar, Sajad Arif, Zulfiqar Ali, M. Masood Laherwal. Conservative management of craniovertebral junction injuries: Still a good option. 05-Apr-2017;8:43. Available from: http://surgicalneurologyint.com/surgicalint-articles/conservative-management-of-craniovertebral-junction-injuries-still-a-good-option/
Abstract
Background:Injuries to the craniovertebral junction (CVJ) are not uncommon, and are among the few skeletal injuries that carry a high mortality rate. Successful management of these injuries depends on familiarity with the normal anatomic relationships of this region, as well as prudent decision making regarding surgical versus conservative management alternatives.
Methods:The purpose of this study was to analyze the indications for conservative treatment of CVJ trauma and to analyze the outcomes.
Results:Eighty-eight patients admitted with CVJ injuries were managed conservatively. More than half were nearly neurologically intact on admission; 91% improved whereas 80% (excluding deaths/lost to follow) ultimately achieved bony union without surgical intervention.
Conclusion:This study documents that conservative management of CVJ injuries in a select population can yield good clinical results.
Keywords: Atlanto-axial subluxation, C1 fracture, C2 fracture, craniovertebral junction (CVJ), odontoid fracture
INTRODUCTION
Here, we reviewed our experience at one institution with 88 patients with craniovertebral junction (CVJ) trauma treated nonsurgically over a 10-year period. Notably, injuries to the CVJ are not uncommon, and are among the few skeletal injuries that carry high mortality rates.[
This study analyzed the indications and outcome of conservative management with immobilization of 88 individuals, as well as correlated the clinical presentation and radiographic findings with nonsurgical treatment options.
MATERIALS AND METHODS
All 88 patients who presented with CVJ trauma admitted to Neurosurgery department at the SKIMS Kashmir (2005–2014) and were managed conservatively were included in this study.
The patients were resuscitated immediately and immobilized by a rigid cervical collar. They subsequently underwent radiographic investigation (e.g., anterioposterior, lateral, and oblique cervical X-rays). Those demonstrating X-ray evidence of fracture/dislocation and or with neurological deficits additionally had computed tomography (CT) scans (including three-dimensional reconstructions); moreover, cervical magnetic resonance (MR) studies were performed. MRI is definitely better than CT scan in evaluating the status of ligaments and cord.[
Clinical features of 88 patients with craniovertebral trauma
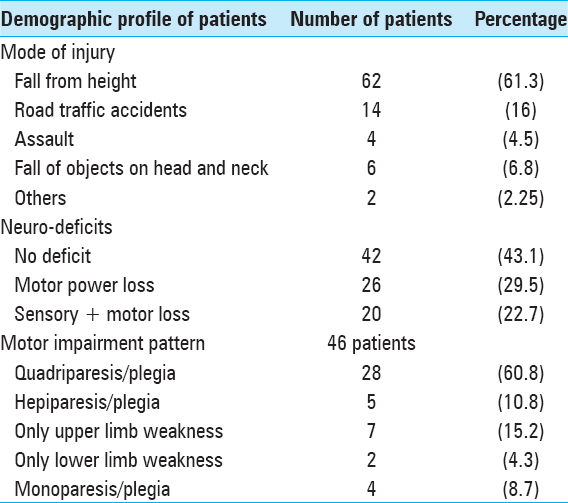
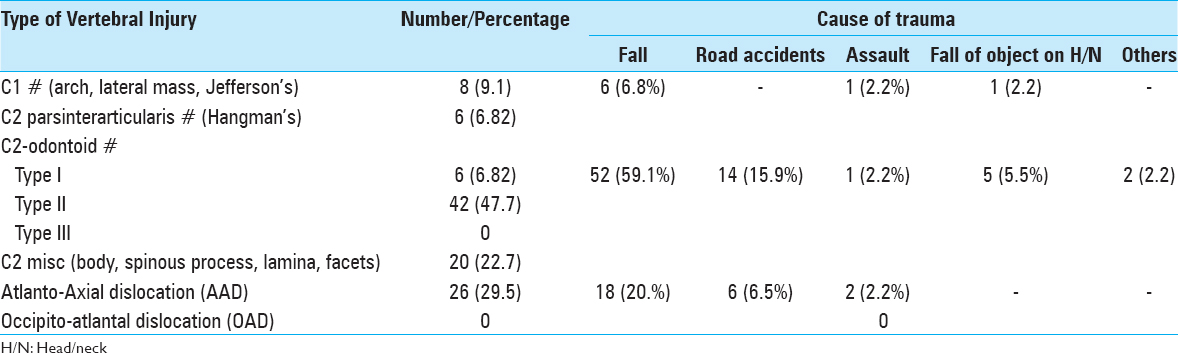
This population included mostly young males aged 21–40 years old (50%). A fall was the most common mode of trauma (61.3%). Notably, 47.7% patients were neurologically intact. Alternatively, 61% were quadriplegia/quadriparetic [
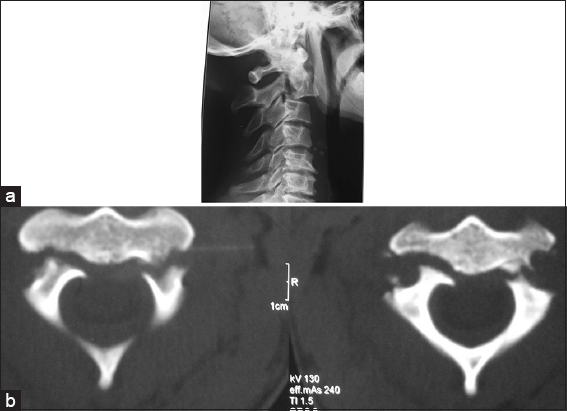
X-Rays were less reliable that CT studies in documenting pathology at the CVJ. Notably, X-rays identified fractures in just 73.6% of the patients, and subluxation in 84.6% patients. Alternatively, CT identified fractures in 97.5% of the patients and subluxation in 92.3%. MR studies also showed evidence of cord injury (e.g., edema, contusion, hematoma) with signal changes detected in 32 patients (36.3%), whereas 56 (67.7%) patients had no sign of cord injury.
All 88 patients were managed conservatively for C1 fracture (100%), Hangman's 66.6%, Odontoid type I 100%, type II 20%, and AAD 12%. Out of the 88 cases, 80 were treated with a Philadelphia collar primarily or following cervical traction, whereas 8 required halo-braces.
RESULTS
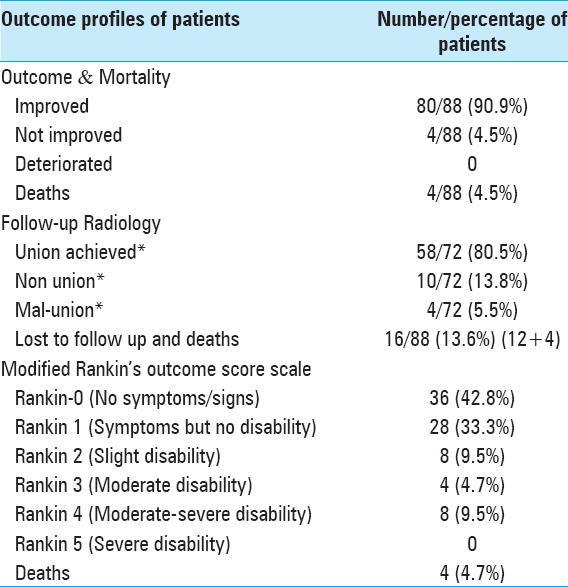
Out of the 88 cases, 80 (90.9%) improved, 4 (4.5%) did not improve, none deteriorated, and 4 (4.5%) died. With regards to initial motor weakness, all patients with power grade III and above showed improvement (100%). Out of 8 patients who had grade 0 power on admission, 4 patients (50%) improved whereas 2 (25%) did not improve and died. On follow-up radiology, 80.5% (58/72) achieved fusion, 13.8% (10/72) had nonunion, and 5.5% (4/72) had malunion by 6 months. For 16 patients, 6-month radiology was unavailable as 12 patients were lost to follow-up (13.6%) and 4 (4.45%) died [
DISCUSSION
Injuries of CVJ are potentially fatal due to close proximity of vital structures such as brainstem, upper cord, and vertebral arteries. Moreover, this region's vulnerability to injury is particularly high because of the large lever-arm induced rostrally by the cranium and the relative freedom of movement of the CVJ, which relies disproportionately on ligamentous structures rather than on intrinsic bony stability. Here, we reviewed our experience at one institution with 88 patients with CVJ trauma treated nonsurgically over a 10-year period. Literature reports that road traffic accidents are the most common mode of injury worldwide (70%),[
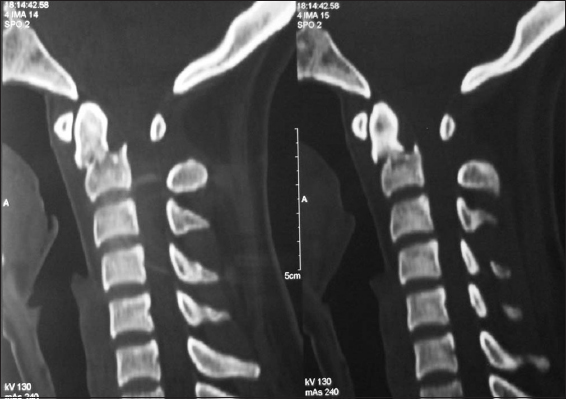
Atlas fractures seen in 8 (9.1%) patients [
Nonoperative treatment options consist of recumbent skeletal traction, bracing (Philadelphia collar and halo), and immobilization. The duration of external immobilization usually ranges from 2 to 4 months.[
Among the conservative group, 90.9% improved, 4.5% did not improve and none deteriorated [
In conservatively treated cases, fusion and nonunion rates were quite similar to operated cases; follow-up radiology revealed that 80.5% achieved fusion, 13.8% had nonunion, and 5.5% had malunion. In cases operated during this period, 81.8% achieved fusion, 4.5% had nonunion, and 9.09% had malunion [
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahuja A, Glasauer FE, Alker GJ, Klein DM. Radiology in survivors of traumatic atlanto-occipital dislocation. Surg Neurol. 1994. 41: 112-8
2. Anderson PA, Budorick TE, Easton KB, Henley MB, Salciccioli GG. Failure of halo vest to prevent in vivo motion in patients with injured cervical spines. Spine. 1991. 16: S501-5
3. Blacksin MF, Lee HJ. Frequency and significance of fractures of the upper cervical spine detected by CT in patients with severe neck trauma. AJR Am J Roentgenol. 1995. 165: 1201-4
4. Bozkus H, Karakas A, Hancı M, Uzan M, Bozdag E, Sarıoglu A. Finite Element Model of the Jefferson Fracture: Comparison with a Cadaver Model. Eur Spine J. 2001. 10: 257-63
5. Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures: Analysis of management and outcome in 340 consecutive cases. Spine. 1997. 22: 1843-52
6. Holmes JF, Mirvis SE, Panacek EA, Hoffman JR, Mower WR, Velmahos GC. Variability in computed tomography and magnetic resonance imaging in patients with cervical spine injuries. J Trauma. 2002. 53: 524-9
7. Landells CD, Van Peteghem PK. Fractures of the atlas: Classification, treatment and morbidity. Spine. 1988. 13: 450-2