- Department of Neurosurgery, The University of Kansas Health System, Kansas City, Kansas,
- Department of Neurosurgery, Carle Illinois College of Medicine, Carle Foundation Hospital, Urbana, Illinois, USA.
- Department of Division of Vascular Surgery, The University of Kansas Health System, Kansas City, Kansas,
Correspondence Address:
Paige Lundy
Department of Division of Vascular Surgery, The University of Kansas Health System, Kansas City, Kansas,
DOI:10.25259/SNI_205_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Paige Lundy, Paul Arnold, Kirk Hance. Coxiella burnetii infection of the spine requiring neurosurgical intervention. 20-Sep-2019;10:182
How to cite this URL: Paige Lundy, Paul Arnold, Kirk Hance. Coxiella burnetii infection of the spine requiring neurosurgical intervention. 20-Sep-2019;10:182. Available from: http://surgicalneurologyint.com/surgicalint-articles/9661/
Abstract
Background: Infections from Coxiella burnetii, resulting in what is known as Q fever, are relatively rare and difficult to diagnose. Very few reports of spinal infection from C. burnetii have been reported rarely have these cases required surgical intervention.
Case Description: We report a patient with the previous vascular surgery and Q fever spinal osteomyelitis. Previously reported cases with spinal involvement have described initial infection of vascular grafts in proximity to the spine. Literature on spinal infection from C. burnetii reports only one case that required surgical intervention of the spine. We report a patient with L5-S1 diskitis who required surgical intervention and subsequent percutaneous drainage.
Conclusion: Spinal infections from C. burnetii are rare; however, in the setting of a patient with osteodiscitis with negative cultures as well as a history of significant vascular disease with stents, the diagnosis of Q fever should be entertained. Operative and interventional procedures should also be considered in these patients to help alleviate pain and maintain neurologic function.
Keywords: Coxiella burnetii, Osteodiscitis, Q fever
INTRODUCTION
Infections from Coxiella burnetii, resulting in what is known as Q fever, are relatively rare and difficult to diagnose. A wide array of clinical presentations with a typical indolent course makes them a diagnostic challenge.[
CASE REPORT
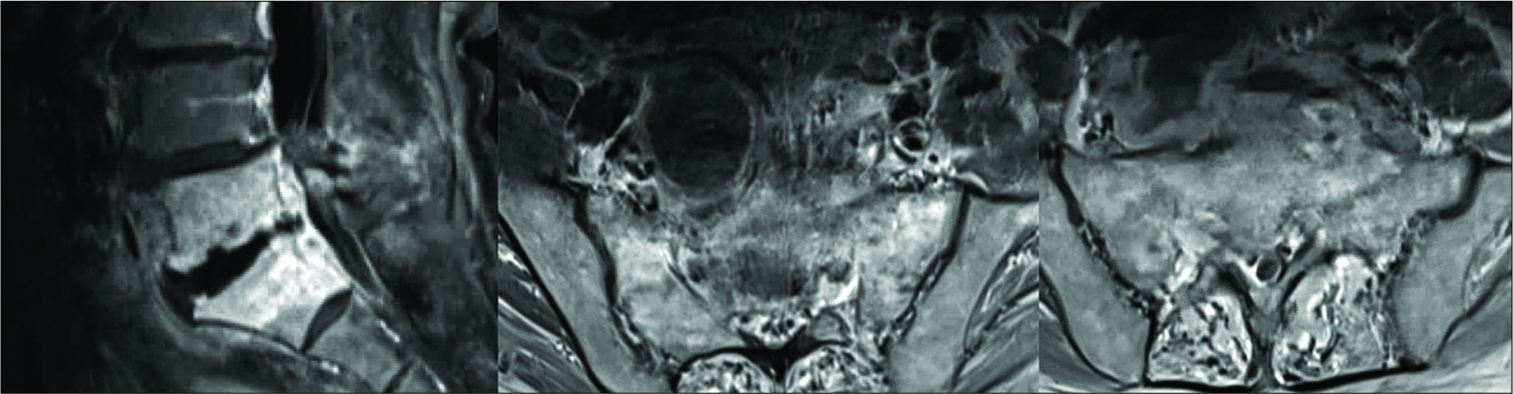
A 74-year-old man with a medical history of coronary artery disease, abdominal aortic aneurysm, and lumbar stenosis presented to the ER in January 2018 reporting severe sharp low back pain with radiation down his right lower extremity. He had recently undergone multiple vascular surgeries including repair of the right internal iliac aneurysm, which required a vascular graft, in April 2017, and L1-4 laminectomy in July 2017. His preoperative symptoms had initially resolved; however, in December 2017, he began to have a gradual return of low back pain and radiculopathy. His neurologic examination was normal. Imaging revealed concerns for L5-S1 osteodiscitis [
Unfortunately, despite antibiotic treatment, the patient pain progressed to the point, he was no longer able to ambulate independently. A positron emission tomography scan was performed in March 2018 that showed progression of the L5-S1 spondylodiscitis with hypermetabolic activity in the paraspinous region as well as around the right iliac artery aneurysm that directly abutted the paraspinous phlegmon. Magnetic resonance imaging (MRI) showed progression of the spondylodiscitis as well with now mild height loss at L5-S1 [
In May, the patient was reporting continue back discomfort with new severe radicular right leg pain. MRI and computed tomography angiography were obtained to reveal a recurrent fluid collection in the prevertebral space. The patient underwent IR drainage/drain placement for this and experienced resolution of his symptoms, and follow-up studies showed resolution of the fluid.
As of the last follow-up, the patient is again ambulating without assistance and has made a marked improvement with plans to continue antibiotic therapy for 12–18 months.
DISCUSSION
Q fever is a zoonosis caused by C. burnetii. Goats, sheep, and cattle are known reservoirs for this Gram-negative bacteria and serve as the source for human infection.[
Pre-existing cardiovascular disease, aortic aneurysms, and vascular grafts are reported risk factor for chronic Q fever infections.[
Reports of spinal involvement are limited, but this diagnosis may serve as an important differential in patients with concomitant vascular grafts and suspected osteodiscitis, especially in the case when initial spinal cultures remain negative and traditional antibiotics fail to adequately treat infection.
O’Donnel et al. presented a series of six patients, all of whom suffered from C. burnetii infections involving vascular prosthetics.[
Landais et al. performed literature review spanning 1966– 2006 that identified three previous cases of pseudoaneurysm of prosthetic aortic bypass grafts and contiguous vertebral osteomyelitis.[
A recent case report from France presents a patient with destruction of the L2-3 disc space associated with an aortic stent graft that had eroded into the body of L3.[
CONCLUSION
Spinal infections from C. burnetii are rare; however, in the setting of a patient with osteodiscitis with negative cultures as well as a history of significant vascular disease with stents, the diagnosis of Q fever should be entertained. Then with proper diagnosis by serology treatment can be appropriately changed. Although rarely reported, operative and interventional procedures should also be considered in these patients to help alleviate pain and maintain neurologic function.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Landais C, Fenollar F, Constantin A, Cazorla C, Guilyardi C, Lepidi H. Q fever osteoarticular infection: Four new cases and a review of the literature. Eur J Clin Microbiol Infect Dis. 2007. 26: 341-7
2. Michel M, Cesini J, Michon J, Dargere S, Vergnaud M, Marcelli C. Vertebral fractures and abdominal aortic aneurysm revealing Q fever. Joint Bone Spine. 2016. 83: 241-2
3. Mongardon N, Dubory A, Dorget A, De Wailly G, Lepeule R, Cochennec F. Vascular infection and vertebral destruction in a patient with Q fever. Lancet Infect Dis. 2018. 18: 226-
4. O’Donnell ME, Manshani N, McCaughey C, Soong C, Lee B. Coxiella burnetii infection of an aortic graft with multiple vertebral body erosion. J Vasc Surg. 2007. 45: 399-403
5. Wegdam-Blans MC, Kampschreur LM, Delsing CE, Bleeker-Rovers CP, Sprong T, van Kasteren ME. Chronic Q fever: Review of the literature and a proposal of new diagnostic criteria. J Infect. 2012. 64: 247-59