- Department of Neurosurgery, University of California-Los Angeles, Los Angeles, California, USA
Correspondence Address:
Alexander M. Tucker
Department of Neurosurgery, University of California-Los Angeles, Los Angeles, California, USA
DOI:10.4103/2152-7806.193727
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tucker AM, Niu T, Nagasawa DT, Everson R, Sedighim S, Buitrago Blanco MM. CT-negative, MRI GRE-positive primary motor cortex contusion causing isolated foot drop. Surg Neurol Int 09-Nov-2016;7:
How to cite this URL: Tucker AM, Niu T, Nagasawa DT, Everson R, Sedighim S, Buitrago Blanco MM. CT-negative, MRI GRE-positive primary motor cortex contusion causing isolated foot drop. Surg Neurol Int 09-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/ct%e2%80%91negative-mri-gre%e2%80%91positive-primary-motor-cortex-contusion-causing-isolated-foot-drop/
Abstract
Background:Isolated acute foot drop due to traumatic brain injury is exceedingly rare and is often misdiagnosed during initial evaluation. Here, we present the case of a patient who presented with left foot drop after falling off a bicycle.
Case Description:The patient is a 55-year-old male who was mountain biking when he fell, hit his head, and lost consciousness. Neurologic examination of the left leg revealed foot drop, no sensory deficits, and 3+ reflexes at the knee and ankle with clonus. Electroencephalography, computed tomography (CT) of the head, magnetic resonance imaging (MRI) of the lumbar spine, and CT of the lower extremities were all negative. Only MRI of the brain with a gradient echo sequence revealed microhemorrhages focused around the right precentral gyrus. The patient underwent physical therapy, and by 3 months had regained full strength in his left leg.
Conclusion:Central causes of foot drop are exceptionally rare, however, they should be considered in all cases of post-traumatic dorsiflexion paresis. The key to the accurate diagnosis is a high index of suspicion as well as thorough and careful physical examination including reflex and sensory testing. Selective imaging modalities such as MRI or CT can then be used to verify the diagnosis.
Keywords: Computed tomography, contusion, foot drop, motor cortex, magnetic resonance imaging, traumatic brain injury
INTRODUCTION
Post-traumatic acute foot drop is most commonly the result of direct peripheral nerve injury at the level of the fibular head or secondary to intervertebral disc herniation causing L5 nerve root compression.[
Here, we present a patient who presented with left lower extremity weakness and isolated foot drop after falling off a bicycle. Work-up included a computerized tomography (CT) of the brain which was negative for acute injury and magnetic resonance imaging (MRI) of the brain which revealed a localized area of hemorrhagic contusion in the right precentral gyrus.
CASE HISTORY
A 55-year-old male was mountain biking and fell 15 feet, hitting his head and losing consciousness. Neurologic examination of the left leg revealed MRC grade 2/5 strength of dorsiflexion (tibialis anterior), MRC grade 1/5 strength distally (extensor digitorum longus, extensor hallucis), no sensory deficits were noted (normal light touch, two-point discrimination, temperature and vibratory sensation modalities), 3+ tendon reflexes at the knee and ankle, and positive sustained clonus. He reported a headache, but was oriented to name, place, and date. Upon work-up, electroencephalogram (EEG) showed no evidence seizures, CT of the head showed no ischemia or hemorrhage, and MRI of the lumbar spine was negative for acute pathology [
Figure 1
(a) Sagittal T2-weighted magnetic resonance imaging (MRI) showing degenerative spondylosis without significant cord compression. (b) Computed tomography scout image of left leg demonstrating fibular head without evidence of fracture. (c) Axial proton-density-weighted turbospin echo MRI showing the L5 nerve roots exiting the spinal canal, no foraminal stenosis, or disc herniation
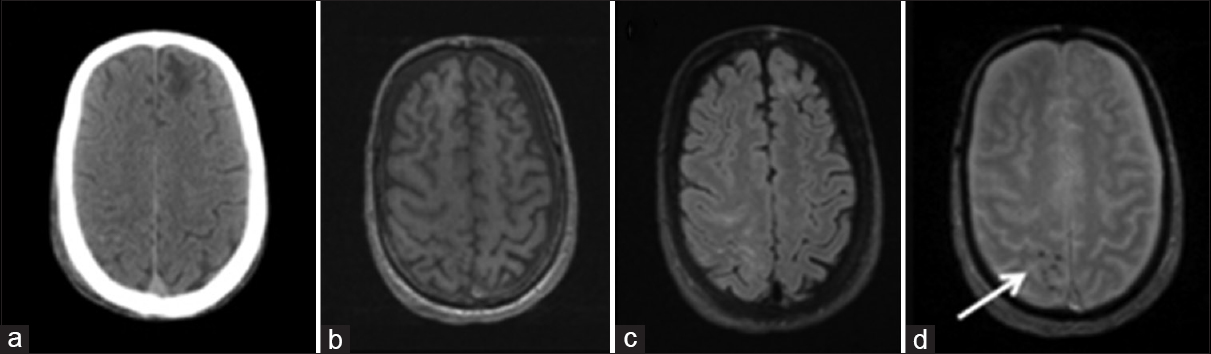
Figure 2
(a) Computed tomography showing chronic left frontal encephalomalacia, but no acute intracranial blood. (b) T1-magnetization prepared rapid gradient echo unremarkable. (c) Fluid-attenuated inversion recovery revealing right frontoparietal hyperintensity. (d) T2-gradient recall echo showing punctate pre and post-central intraparenchymal hemorrhage (white arrow)
DISCUSSION
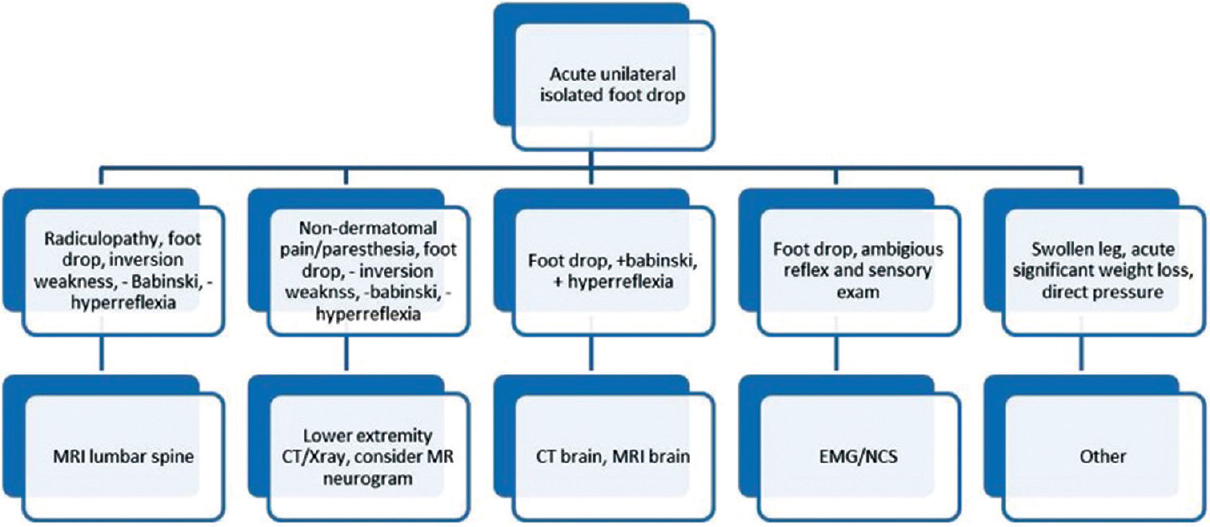
Foot drop or dorsiflexion paresis is typically the result of a lower motor neuron injury, such as a lumbar 4-5 disc herniation or a common peroneal nerve injury at the fibular head.[
Despite a low prevalence, we believe that central etiologies of foot drop must be included in the differential diagnosis of all patients presenting with head trauma and unilateral lower extremity weakness. When examining such patients, particular attention should be paid to upper motor neuron signs; Babinski’s sign, hyper-reflexia, and clonus. A detailed sensory exam should also be carefully conducted to determine the existence of sensory changes within a dermatomal distribution. In individuals with clear discogenic or peroneal etiology, MRI of the lumbar spine or CT of the lower extremity in question should be readily obtained to establish the correct diagnosis and treatment. If these imaging studies are nondiagnostic, electrophysiologic studies and cranial evaluation should be considered.
Although the quality of CT imaging of the brain continues to advance, MRI remains the most sensitive neurodiagnostic imaging modality for the evaluation of intracranial hemorrhage.[
Other rare causes of foot drop include deep venous thrombosis, rapid weight loss after bariatric surgery, severe diabetic neuropathy, Hansen’s disease, nerve compression during sleep, surgery, or while in stirrups during gynecologic procedures, as well as orthopedic injuries such as hip dislocation, acetabular fractures, proximal fibular fractures, or tight plaster casts.[
CONCLUSION
While central causes of foot drop are exceptionally rare,[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Atac K, Ulas UH, Erdogan E, Gokcil Z. Foot drop due to cranial gunshot wound. Mil Med. 2004. 169: 568-9
2. Baima J, Krivickas L. Evaluation and treatment of peroneal neuropathy. Curr Rev Musculoskelet Med. 2008. 1: 147-53
3. Djekidel M, Harb W. A case of foot drop as an expression of brain metastases?. Neurologist. 2006. 12: 274-5
4. Elias WJ, Nader P, Oskouisan RJ, Schirmer B, Burns T. Peroneal neuropathy following successful bariatric surgery. J Neurosurg. 2006. 105: 631-5
5. Fazekas F, Kleinert R, Roob G, Kleinert G, Kapeller P, Schmidt R. Histopathologic analysis of foci of signal loss on gradient-Echo T2*-weighted MR images in patients with spontaneous intracerebral hemorrhage: Evidence of microangiopathy-related microbleeds. AJNR Am J Neuroradiol. 1999. 20: 637-42
6. Fukada H. Bilateral peroneal nerve palsy caused by intermittent pneumatic compression. Int Med. 2006. 45: 93-4
7. Gentry LR, Godersky JC, Thompson B. MR imaging of head trauma: Review of the distribution and radiopathologic features of traumatic lesions. AJR Am J Roentgenol. 988. 50: 663-72
8. Katirji MB, Wilbourn AJ. Common peroneal mononeuropathy: A clinical and electrophysiologic study of 116 lesions. Neurology. 1988. 38: 1723-8
9. Kidwell CS, Chalela JA, Saver JL, Starkman S, Hill MD, Demchuk AM. Comparison of MRI and CT for detection of acute intracerebral hemorrhage. JAMA. 2004. 292: 1823-30
10. Oktem NB, Tari R, Kotil K, Bilge T. Cerebral contusion as a rare cause of foot drop: Case report. Turk Neurosurg. 2012. 22: 99-101
11. Ozdemir N, Citak G, Acar UD. Spastic foot drop caused by a brain tumour: A case report. Br J Neurosurg. 2004. 18: 314-5
12. Ozdemir N, Gelal MF, Oguzoglu S, Minoglu M. Unilateral acute foot drop due to diffuse axonal injury after head trauma. J Clin Neurosci. 2008. 15: 1051-3
13. Ricarte IF, Figueiredo MM, Fukuda TG, Pedroso JL, Silva GS. Acute foot drop syndrome mimicking peroneal nerve injury: An atypical presentation of ischemic stroke. J Stroke Cerebrovasc Dis. 2014. 23: 1229-31
14. Westhout FD, Pare LS, Linskey ME. Central causes of foot drop: Rare and underappreciated differential diagnoses. J Spinal Cord Med. 2007. 30: 62-6