- Bone Joint and Related Tissues Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran
Correspondence Address:
Abbas Amirjamshidi
Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran
DOI:10.4103/sni.sni_359_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ali A. Esmailiejah, Mohammadreza Abbasian, Ramin Bidar, Nina Esmailiejah, Farshad Safdari, Abbas Amirjamshidi. Diagnostic efficacy of clinical tests for lumbar spinal instability. 25-Jan-2018;9:17
How to cite this URL: Ali A. Esmailiejah, Mohammadreza Abbasian, Ramin Bidar, Nina Esmailiejah, Farshad Safdari, Abbas Amirjamshidi. Diagnostic efficacy of clinical tests for lumbar spinal instability. 25-Jan-2018;9:17. Available from: http://surgicalneurologyint.com/surgicalint-articles/diagnostic-efficacy-of-clinical-tests-for-lumbar-spinal-instability/
Abstract
Background:Although various clinical tests are utilized to assess lumbar spine instability (LSI), few have documented diagnostic efficacy. We assessed the diagnostic efficacy of four clinical and one radiographic test for LSI in patients with degenerative lumbar disease.
Methods:A cohort of 52 patients with pain attributed to lumbar spine stenosis and degenerative spondylolisthesis were prospectively evaluated utilizing dynamic X-rays, the passive lumbar extension (PLE) test, instability catch sign, painful catch sign, and the apprehension sign. The results of these preoperative tests were compared with spinal surgeons’ intraoperative documentation of spinal instability considered in this study as the “gold” standard.
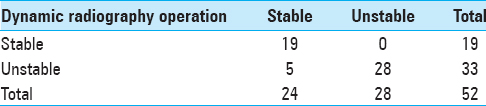
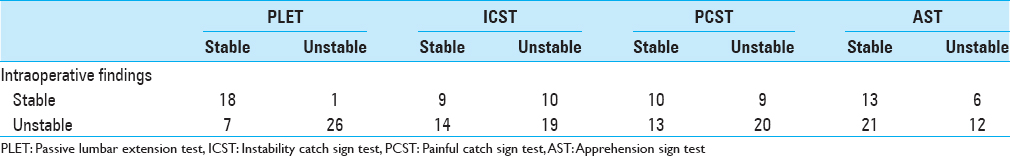
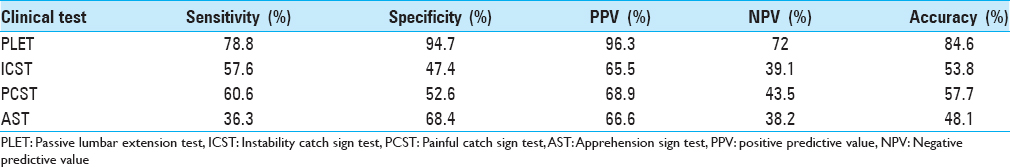
Results:Intraoperatively, 33 patients demonstrated instability (63.5%) whereas 28 had motion documented on preoperative dynamic radiography. The sensitivity, specificity, positive, and negative predictive value and accuracy of dynamic radiography were 84.8%, 100%, 100%, 79.1%, and 90.4%, respectively. The diagnostic efficiency of PLE was higher than other additional studies – sensitivity 78.8%, specificity 94.7%, positive predictive value 96.3%, negative predictive value 72%, and accuracy rate 84.6%.
Conclusion:Dynamic radiography was more reliable than any of the clinical tests in diagnosing LSI. Among the latter, PLE had the highest diagnostic value for establishing LSI.
Keywords: Clinical test, diagnostic efficacy, dynamic radiography, instability, spine
INTRODUCTION
Lumbar spinal instability (LSI) is a common cause of nonspecific low back pain (LBP).[
We investigated the diagnostic efficacy of dynamic X-rays and four clinical tests to assess LSI: (a) passive lumbar extension (PLE) test, (b) instability catch sign, (c) painful catch sign, and (d) apprehension sign utilized to establish the diagnosis of LSI. Furthermore, patients were followed 6 months postoperatively with dynamic X-rays to determine if they became unstable.
MATERIALS AND METHODS
Clinical data
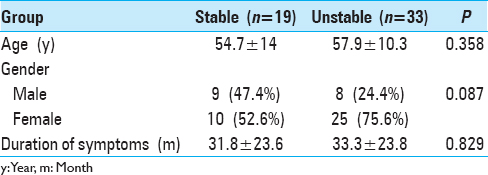
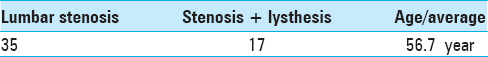
The 52 patients included in this prospective study met the following inclusion criteria: (1) back/radicular leg pain, (2) age between 50 and 70 years, (3) diagnostic studies showing degenerative lumbar spine disease, (4) patients who underwent laminectomy for lumbar spine stenosis and/or degenerative spondylolisthesis [
Imaging assessment
Preoperatively, all patients had dynamic radiographs and MRI [
Intervention
Patients underwent decompression by the two attending surgeons who could see the images but were not informed of the outcome of the clinical tests. They could independently judge whether patients had LSI and required fusion or not. In addition, patients underwent dynamic X-rays 6 months postoperatively to see if they developed LSI.
Lumbar canal stenosis was present in 35 patients, whereas stenosis/degenerative spondylolisthesis was found in 17. The average age of patients was 56.7 years.
Statistical analysis
The independent samples t-test (quantitative) and Chi-square test (qualitative) were utilized to compare data between patients with/without LSI. The qualitative data were compared using Pierson's or Spearman's correlation test using SPSS software (version 15.0). P > 0.05 while the sensitivity, specificity, accuracy, positive and negative predictive values of dynamic radiography and clinical tests were calculated.
RESULTS
Although preoperative dynamic X-rays showed LSI in 28 patients, 33 patients were unstable intraoperatively (63.5%). The sensitivity, specificity, PPV, NPV, and accuracy of dynamic radiography in establishing the diagnosis of LSI were uniformly high [Tables
DISCUSSION
Intraoperative documentation of LSI best correlated with preoperative dynamic X-ray evidence of instability. Similar to Kasai et al.,[
Limitations
Although two expert spine surgeons evaluated the presence of intraoperative LSI, there may still be nonreproducible intraoperative surgeon-bias constituting a flaw in the study design. Another shortcoming of this study is the relatively low number of cases included.
CONCLUSION
Preoperative dynamic X-rays best predicated the chance of intraoperative documentation of LSI as performed by two spine surgeons. Among the clinical tests for assessing preoperative LSI, the PLE had the highest predictive value.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alqarni AM, Schneiders AG, Hendrick PA. Clinical tests to diagnose lumbar segmental instability: A systematic review. J Orthop Sports Phys Ther. 2011. 41: 130-40
2. Alyazedi FM, Lohman EB, Wesley Swen R, Bahjri K. The inter-rater reliability of clinical tests that best predict the subclassification of lumbar segmental instability: Structural, functional and combined instability. J Man Manip Ther. 2015. 23: 197-204
3. Denteneer L, Stassijns G, De Hertogh W, Truijen S, Van Daele U.editors. Inter- and Intrarater Reliability of Clinical Tests Associated With Functional Lumbar Segmental Instability and Motor Control Impairment in Patients With Low Back Pain: A Systematic Review. Arch Phys Med Rehabil. 2017. 98: 151-64-e6
4. Hammouri QM, Haims AH, Simpson AK, Alqaqa A, Grauer JN. The utility of dynamic flexion-extension radiographs in the initial evaluation of the degenerative lumbar spine. Spine (Phila Pa 1976). 2007. 32: 2361-4
5. Hicks GE, Fritz JM, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil. 2003. 84: 1858-64
6. Kasai Y, Morishita K, Kawakita E, Kondo T, Uchida A. A new evaluation method for lumbar spinal instability: Passive Lumbar Extension Test. Phys Ther. 2006. 86: 1661-7






Sunil Munakomi
Posted February 8, 2018, 5:04 pm
One of the simple clinical methods for diagnosing underlying lumbar canal stenosis is looking out for the presence of extensor digitorum brevis (EDB) wasting on the lateral aspect of the foot. This is supplied by L5 which is the mostly affected region on degenerative lumbar canal stenosis.This method is reliable with minimal inter-observer bias.