- Department of Neurosurgery, Allegheny General Hospital, Drexel University College of Medicine, Pittsburgh, Pennsylvania, USA
- Department of Neurosurgery, Lariboisière Hospital, Assistance Publique – Hôpitaux de Paris, University of Paris VII-Diderot, Paris, France
- Department of Neurosurgery, University of Cincinnati College of Medicine, Cincinnati, Ohio, USA
Correspondence Address:
Khaled M. Aziz
Department of Neurosurgery, Allegheny General Hospital, Drexel University College of Medicine, Pittsburgh, Pennsylvania, USA
DOI:10.4103/2152-7806.195575
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nouman Aldahak, Mohamed El Tantowy, Derrick Dupre, Alexander Yu, Jeffrey T. Keller, Sebastien Froelich, Khaled M. Aziz. Drilling of the marginal tubercle to enhance exposure via mini pterional approach: An anatomical study and clinical series of 25 sphenoid wing meningiomas. 12-Dec-2016;7:
How to cite this URL: Nouman Aldahak, Mohamed El Tantowy, Derrick Dupre, Alexander Yu, Jeffrey T. Keller, Sebastien Froelich, Khaled M. Aziz. Drilling of the marginal tubercle to enhance exposure via mini pterional approach: An anatomical study and clinical series of 25 sphenoid wing meningiomas. 12-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/drilling-of-the-marginal-tubercle-to-enhance-exposure-via-mini-pterional-approach-an-anatomical-study-and-clinical-series-of-25-sphenoid-wing-meningiomas/
Abstract
Background:The marginal tubercle (MT) of zygomatic bone can be an obstacle in the standard mini pterional (MPT) craniotomy; we aim to evaluate the effect of drilling this MT in enhancing the exposure of MPT craniotomy for resection of sphenoid wing meningiomas (SWMs).
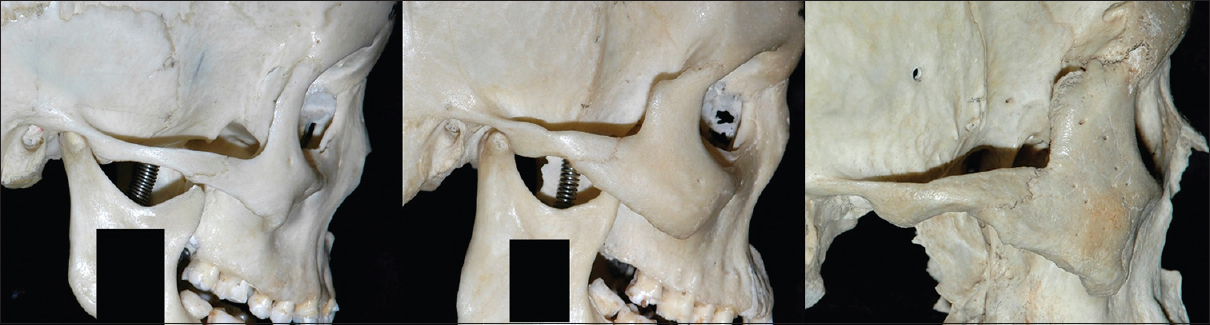
Methods:The authors utilized 60 dry skulls to perform the anatomical part of the study. The MT size was reflected by the AB distance, wherein point A is the most prominent part of MT and point B is located on the orbital rim in the same axial plane as point A. The authors analyzed the effect of MT size in masking the sphenozygomatic suture (SZS), which is the most anterior part of the MPT craniotomy. One silicon-injected embalmed specimen was used to demonstrate other modifications to the standard MPT approach. The results of the anatomical analysis were translated into the second part of the study, which consisted of the resection of 25 SWMs.
Results:The MT obscured visualization when the AB distance measured 13 mm or greater. In the clinical series of SWMs, drilling such prominent MT maximized exposure during MPT approach.
Conclusion:The MPT approach could be used for the resection of SWMs. Drilling of prominent MTs can enhance and optimize exposure to SWMs through standard MPT approaches.
Keywords: Anatomic study, meningioma, minimally invasive neurosurgery, minipterional approach, skull base, surgical technique
INTRODUCTION
The minipterional (MPT) approach was first described by Figueiredo et al.[
Because of its small bony exposure, the MPT approach requires maximization of craniotomy by removing all obstacles that can hinder the microscopic view.
The marginal tubercle (MT) of the zygomatic bone (processus marginalis) is an elevation on the posterior border of the frontal processes of the zygomatic bone, just above the angle between the frontal and temporal processes of the zygoma.[
Sphenoid wing meningiomas (SWMs) account for approximately 20% of supratentorial meningiomas.[
Various surgical approaches have traditionally been used for the resection of SWMs, including frontolateral,[
The authors aim to determine if the MT could be an obstacle in the standard mini pterional MPT approach. Second, to evaluate the effect of drilling the MT for increased exposure during resection of SWMs.
MATERIALS AND METHODS
The study is comprises two parts: The first one is anatomical; the authors analyzed the degree to which the MT obscures the surgical window in the standard MPT approach. The second part aims to translate the results of the anatomical part of the study into a series of 25 SWMs where the MPT approach was used. However, two additional technical modifications have been added to the standard MPT approach based upon the authors’ experience in skull base surgery.
Anatomical study
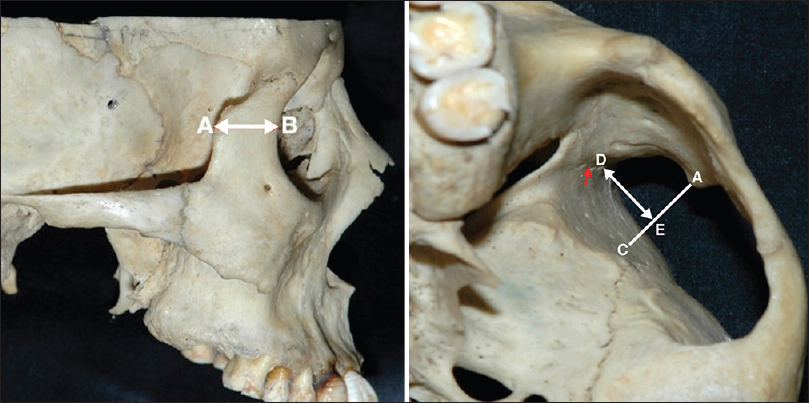
This anatomical study was performed in the Mayfield skull base laboratory in the University of Cincinnati, Ohio, USA. Sixty dried skulls were utilized bilaterally (120 cranial hemispheres). We identified the size of MT by the AB line, wherein the point A is the most prominent part of MT. The point B represents the intersection of a line drawn on axial plane from point A to the anterior edge of frontal processes of zygomatic bone “orbital rim” [
From point A, a line is drawn perpendicular on the extracranial surface of greater sphenoid wing; the intersection is referred to as point C [
Starting from the sphenozygomatic suture (SZS), which is the most anterior part of the MPT craniotomy, a perpendicular line is drawn to intersect the AC line at point E; this line is referred to as ED, wherein the point D is the starting point on the SZS [
The ED line represents the part of bone flap masked by the MT. This area is termed the marginal recess (MR). The relationship between AB distance (MT Size) and ED distance (MR size) was analyzed in order to determine the size of MT, from which this bony projection becomes an obstacle in MPT approach.
Two other modifications to the standard MPT approach were added, these modifications are demonstrated on a silicon-injected embalmed head specimen. The dissection study was performed in the skull base laboratory in Allegheny General Hospital, Pittsburgh, USA.
Clinical series of sphenoid wing meningiomas
Utilizing the MPT approach, 25 patients with SWMs underwent microsurgical resection between July 2006 and February 2016. Surgeries were performed in Allegheny General Hospital, Pittsburgh, Pennsylvania, USA by a single surgeon (KA). AB distance was measured on the preoperative computed tomography (CT). MT was drilled in some cases according to the results of the anatomical study in order to enhance the surgical exposure. The value of an additional exposure offered by MT drilling was evaluated by the surgeon's impression and comfort during the surgery.
RESULTS
Anatomical study
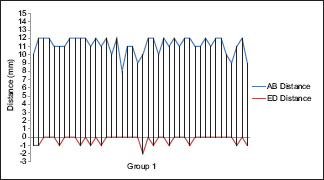
The SZS was visualized in an unobscured, straight-on perpendicular fashion when ED (MR) was 0 or less [
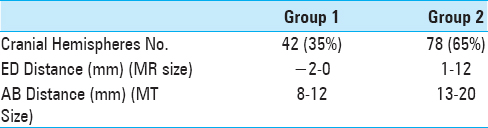
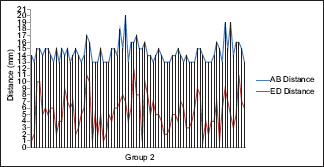
To demonstrate this, the authors divided the craniums into two groups; Group 1, where the ED distance measured 0 or less, and Group 2, where the ED distance measured 1 mm or greater [
The authors noted a relationship between AB (MT size) and ED (MR size). The bigger AB was, the bigger ED was. In essence, the more prominent the MT was, the more anterior the SZS was (Chart
Forty-two of 120 cranial hemispheres (35%) were assigned to Group 1. In this group, the MT size ranged 8–12 mm. Group 2 included 78 (65%) cranial hemispheres. In this group, MR size ranged between 1 and 12 mm, which implies that the anterior perpendicular surgical view is hidden at least 1 mm by the MT. The AB distance ranged in this group between 13 and 20 mm.
Because of the direct correlation between MT and MR, and by looking at the results of Group 2, the authors concluded that the straight perpendicular surgical view on the anterior limit of MPT approach (SZS) is hidden by at least 1 mm when the AB distance measured 13 mm or more. In these cases, drilling the MT should be considered to enhance surgical exposure. These results were subsequently translated into the clinical series.
Clinical series
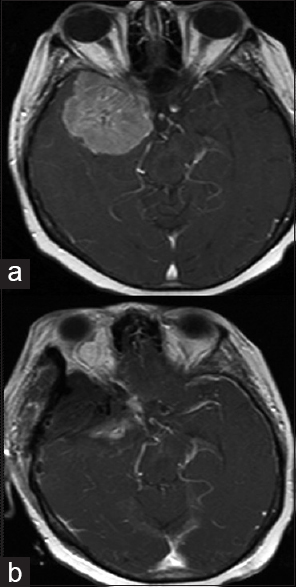
Utilizing the MPT approach, 25 patients with SWMs underwent microsurgical resection. There were 16 females and 9 males, with an age range of 26 to 85 years (mean = 60.2). Eleven patients had lateral SWMs, 7 had middle SWMs, 5 were en-plaque meningiomas, and 2 were sphenocavernous meningiomas. Tumor size ranged from 2.2 cm to 6 cm in maximum diameter (mean: 3.6 cm). Simpson grade one resection was achieved in 22 (88%) patients. The 2 patients with sphenocavernous meningiomas had Simpson grade 4 resection (excision did not extend beyond the lateral wall of cavernous sinus). One patient with en plaque meningioma had Simpson grade 4 resection due to erosion of sphenoid bone and extension into the nasal cavity.
Preoperative CT scans were used to measure the AB distance. Drilling the MT was considered when the AB distance was 13 mm or more. In result, MT was drilled in 13 out of 25 patients. At the time of surgery, exposure enhancement was subjectively recorded by the surgeon (KA). [
Operative technique
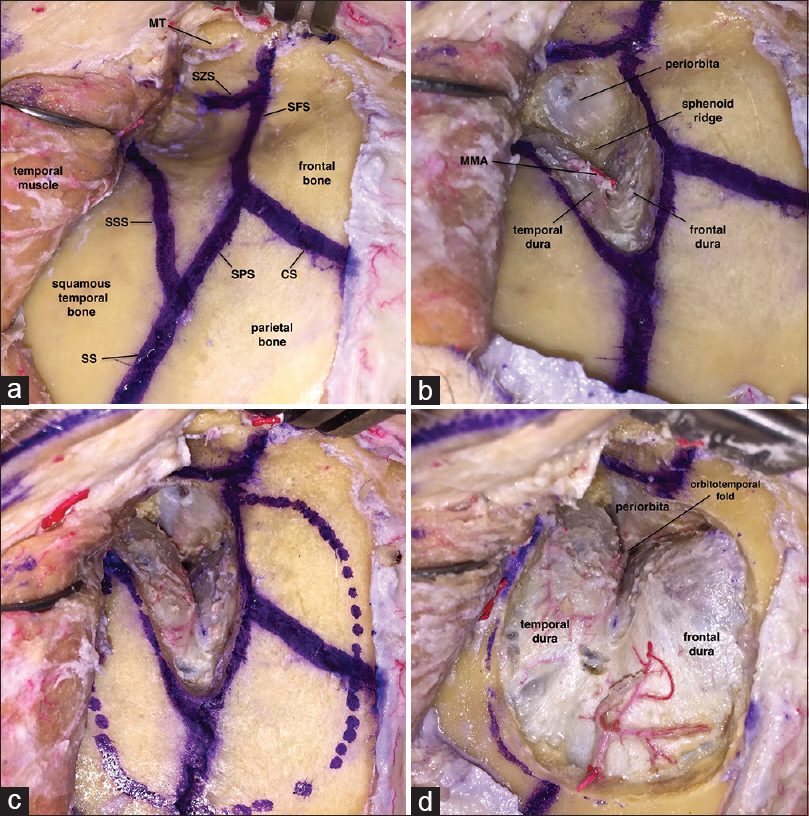
Position: Same as traditional pterional approach[ All patients were electrophysiologically monitored utilizing somatosensory evoked potentials (SSEP) and motor evoked potentials (MEP) Skin incision and soft tissue dissection stage: Same as traditional MPT approach.[ A sphenoid keyhole is placed at the sphenoidal component of the pterion. The authors enlarged the keyhole by drilling the whole extracranial surface of the greater wing of sphenoid. Drilling continues until the temporal dura, frontal dura, and periorbita are exposed [ The large keyhole allows for sphenoid ridge drilling before elevation of the bone flap [ The marginal tubercle is drilled when the AB distance is 13 mm or more, according to preoperative CT scan measurements The authors perform an extradural flattening to orbital roof without orbital osteotomy to minimize the brain retraction Centering it over the meningioma and Sylvian fissure, the dura is opened in a semi-lunar fashion and reflected anteriorly Following the intracranial part of the surgery, the bone defect is repaired using titanium mesh and/or bone cement. Temporalis muscle and fascia are reattached along a muscle cuff using absorbable running sutures. Subgaleal/submuscular drains are left behind to prevent fluid collections.
Figure 4
Cadaver photos illustrating the authors’ technique keyhole. (a) Bone exposure for a left-side standard MPT approach; (b) keyhole enlargement by drilling the extracranial surface of sphenoid wing; (c) drilling sphenoid ridge before performing the craniotomy; (d) craniotomy. CS = coronal suture; SS = squamosal suture; SFS = sphenofrontal suture; SPS = sphenoparietal suture; SSS = sphenosquamosal suture; SZS = sphenozygomatic suture; MT = marginal tubercle, MMA = middle meningeal artery
Complications
One patient had postoperative epidural hematoma requiring surgical evacuation and was discharged home 1 week later without any clinical sequelae. One patient developed a pseudomeningocele, which resolved after placement of a lumbar drain for 3 days, draining at 10 cc/h. This patient was discharged home 6 days postoperatively without neurological sequelae. One patient with radiation-induced multiple meningiomas (left sphenoid wing, right parasagittal and right cerebellopontine angle) and ventriculomegaly underwent MPT approach for resection of lateral SWM, and a Simpson grade 1 resection was achieved. Three days later, the patient developed pseudomeningocele and cerebrospinal fluid (CSF) leak. Lumbar drain was placed and CSF was diverted at 10 cc/h for 6 days. Owing to inability to wean the drain, the decision was made to place a ventriculoperitoneal shunt as a more permanent solution to the CSF leak. Prior to discharge, the patient developed a pulmonary embolus (PE) requiring mechanical ventilation, from which he later fully recovered and were discharged home without any neurologic sequelae (total hospital stay was 23 day).
Hospital stay ranged from 3 to 23 days, with an average of 4.28 days. Twenty of 25 patients (80%) were hospitalized for 3 days postoperatively. One patient stayed for 4 and another for 6 days due to social reasons. Three patients had postoperative complication and stayed for 8, 6, and 23 days as mentioned above.
No approach-related complication was noted in any of the patients. Both patient and surgeon were satisfied with cosmetic results during the follow-up visit in all cases.
DISCUSSION
The standard pterional approach is among the most popular approaches in contemporary neurosurgery. Because of the extent of dissection involved with the standard pterional approach, adverse outcomes have been described and include injury of the frontal branch of the facial nerve, temporalis muscle dysfunction, temopromandibular joint pain, frontal sinus violation, and poor cosmetic results.[
Figueiredo et al.[
Based upon the author's experience in skull base surgery, two modifications to the standard MPT approach were added. First, after placing a burr hole on the sphenoid component of pterion, the cranial surface of greater wing of sphenoid is drilled up to the frontosphenoidal, the sphenosquamosal, and the sphenoparietal sutures. Thereafter, drilling on the sphenoid ridge is continued to obtain a large keyhole, permitting a safe dissection of the dura in all directions.
The second modification consists of an extradural flattening to orbital roof without need of orbital osteotomy. This maneuver enhances the surgical field and provides less brain traction.
In addition to these modifications, the authors noted that the MT could be an obstacle to reach the maximum anterior exposure. Because of this, the authors performed the anatomical study aiming to better understand the effect of this anatomical projection in mimicking the view in the MPT approach. The result of the anatomical study concluded that the MT should be drilled when the AB distance measures 13 mm or more.
To translate these results into operating room, AB distance was measured on preoperative CT scan. The surgeon stated that the maximum anterior exposure while resecting a SWM was better after performing a drilling of prominent MT where the AB distance is 13 mm or more.
Simpson grade 1 resection was not achieved in 3 cases, however, it is felt this is not related to lack of surgical exposure. In 2 cases, where the meningioma extended into the cavernous sinus, the partial resection was anticipated preoperatively. The other case was an en plaque meningioma extending into the nasal cavity by erosion of the sphenoid bone; the total surgical removal was not possible by a single transcranial approach, and needed a combination with endonasal route.
CONCLUSION
The MPT approach, when supported by several modifications, could be used for the resection of SWMs. Drilling of the MT should be considered in some cases to enhance and optimize exposure; thus, to achieve the principle of the MPT approach by creating an optimum balance between the craniotomy size and surgical exposure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abdel Aziz KM, Bhatia S, Tantawy MH, Sekula R, Keller JT, Froelich S. 2011. Minimally invasive transpalpebral “eyelid” approach to the anterior cranial base. Neurosurgery. 2011. 69: ons195-206
2. Al-Mefty O. Supraorbital-pterional approach to skull base lesions. Neurosurgery. 1987. 21: 474-7
3. Badie B. Cosmetic reconstruction of temporal defect following pterional [corrected] craniotomy. Surg Neurol. 1996. 45: 383-4
4. Basso A, Carrizo A, Kreutel A, Martino A, Cerisola J, Torrieri A, Amezua L. Surgical treatment of the spheno-orbital tumors (author's transl). Neurochirurgie. 1978. 24: 71-82
5. Caplan JM, Papadimitriou K, Yang W, Colby GP, Coon AL, Olivi A. 2014. The minipterional craniotomy for anterior circulation aneurysms: Initial experience with 72 patients. Neurosurgery. 2014. 10: 200-6
6. Carrizo A, Basso A. Current surgical treatment for sphenoorbital meningiomas. Surg Neurol. 1998. 50: 574-8
7. Cunningham DJ, Robinson A.editors. Ossa Zygomatica. Cunningham's textbook of anatomy. London: 1918. p. 153-
8. Cushing H, Eisenhardt L.editorsMeningiomas: Their Classification, Regional Behaviour, Life History, and Surgical End Results. Springfield, Illinois: Charles C Thomas; 1938. p.
9. Dolenc V. Microsurgical removal of large sphenoidal bone meningiomas. Acta Neurochir Suppl. 1979. 28: 391-6
10. Figueiredo EG, Deshmukh P, Nakaji P, Crusius MU, Crawford N, Spetzler RF. 2007. The minipterional craniotomy: Technical description and anatomic assessment. Neurosurgery. 2007. 61: 256-64
11. Figueiredo EG, Deshmukh V, Nakaji P, Deshmukh P, Crusius MU, Crawford N. An anatomical evaluation of the mini-supraorbital approach and comparison with standard craniotomies. Neurosurgery. 2006. 59: ONS212-20
12. Harland SP, Hussein A, Gullan RW. Modification of the standard pterional approach for aneurysms of the anterior circle of Willis. Br J Neurosurg. 1996. 10: 149-53
13. Hernesniemi J, Ishii K, Niemela M, Smrcka M, Kivipelto L, Fujiki M. Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl. 2005. 94: 17-21
14. Kattner KA, Fukushima T. Management of vascular invasion during radical resection of medial sphenoid wing meningiomas. Skull Base. 2001. 11: 99-104
15. Salcman M, Kempe LG.editors. Pterional or Frontotemporal Craniotomy, Opening and Closure. Operative Neurosurgery. New York: Springer-Verlag; 2004. 1: 3-17
16. Langevin CJ, Hanasono MM, Riina HA, Stieg PE, Spinelli HM. Lateral transzygomatic approach to sphenoid wing meningiomas. Neurosurgery. 2010. 67: 377-84
17. McDermott MW, Durity FA, Rootman J, Woodhurst WB. Combined frontotemporal-orbitozygomatic approach for tumors of the sphenoid wing and orbit. Neurosurgery. 1990. 26: 107-116
18. Morris H.editors. The Zygomatic. Morris's Human anatomy. Part 1. Philadelphia: P. Blakiston's Son and Co; 1907. p. 84-
19. Nakamura M, Roser F, Jacobs C, Vorkapic P, Samii M. 2006. Medial sphenoid wing meningiomas: Clinical outcome and recurrence rate. Neurosurgery. 2006. 58: 626-39
20. Nathal E, Gomez-Amador JL. Anatomic and surgical basis of the sphenoid ridge keyhole approach for cerebral aneurysms. Neurosurgery. 2005. 56: 178-85
21. Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005. 57: 242-55
22. Schick U, Bleyen J, Bani A, Hassler W. Management of meningiomas en plaque of the sphenoid wing. J Neurosurg. 2006. 104: 208-14
23. Sughrue ME, Rutkowski MJ, Chen CJ, Shangari G, Kane AJ, Parsa AT. Modern surgical outcomes following surgery for sphenoid wing meningiomas. J Neurosurg. 2013. 119: 86-93
24. van Lindert E, Perneczky A, Fries G, Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms: Concept and technique. Surg Neurol. 1998. 49: 481-9
25. Welling LC, Figueiredo EG, Wen HT, Gomes MQ, Bor-Seng-Shu E, Casarolli C. Prospective randomized study comparing clinical, functional, and aesthetic results of minipterional and classic pterional craniotomies. J Neurosurg. 2015. 122: 1012-9