- Department of Neurosurgery, Mitsui Memorial Hospital, Tokyo, Japan
- Department of Neurosurgery, Tokyo University, Tokyo, Japan
Correspondence Address:
Saiko Watanabe
Department of Neurosurgery, Mitsui Memorial Hospital, Tokyo, Japan
DOI:10.4103/2152-7806.194498
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Saiko Watanabe, Kenichi Amagasaki, Naoyuki Shono, Hiroshi Nakaguchi. Fibrin glue injection into the hematoma cavity for refractory chronic subdural hematoma: A case report. 21-Nov-2016;7:
How to cite this URL: Saiko Watanabe, Kenichi Amagasaki, Naoyuki Shono, Hiroshi Nakaguchi. Fibrin glue injection into the hematoma cavity for refractory chronic subdural hematoma: A case report. 21-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/fibrin-glue-injection-into-the-hematoma-cavity-for-refractory-chronic-subdural-hematoma-a-case-report/
Abstract
Background:Repeat burr hole irrigation and drainage has been effective in most cases of recurrent chronic subdural hematoma (CSDH), however, refractory cases require further procedures or other interventions.
Case Description:An 85-year-old male presented with left CSDH, which recurred five times. The hematoma was irrigated and drained through a left frontal burr hole during the first to third surgery and through a left parietal burr hole during the fourth and fifth surgery. The hematoma had no septation and was well-evacuated during each surgery. Antiplatelet therapy for preventing ischemic heart disease was stopped after the second surgery, the hematoma cavity was irrigated with artificial cerebrospinal fluid at the third surgery, and the direction of the drainage tube was changed to reduce the postoperative subdural air collection at the fourth surgery. However, none of these interventions was effective. He was successfully treated by fibrin glue injection into the hematoma cavity after the fifth surgery.
Conclusion:This procedure may be effective for refractory CSDH in elderly patients.
Keywords: Chronic subdural hematoma, fibrin glue, recurrence, refractory
INTRODUCTION
Chronic subdural hematoma (CSDH) is the most common disorder encountered in daily neurosurgical practice, and the incidence increases with higher age.[
CASE REPORT
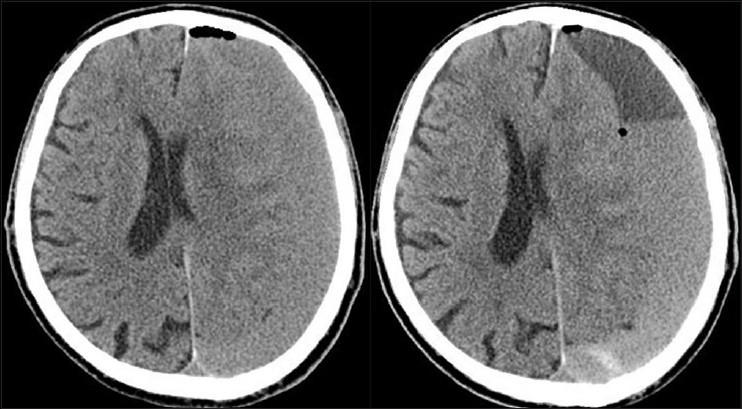
An 85-year-old male, who had been able to walk with a wheeled walker and had no definitive cognitive problem, was admitted to our hospital because of mild disturbance of consciousness and right hemiparesis. He had no history of head trauma but had been taking oral antiplatelet agent for previous ischemic heart disease. Computed tomography (CT) revealed left CSDH with moderate rightward midline shift [
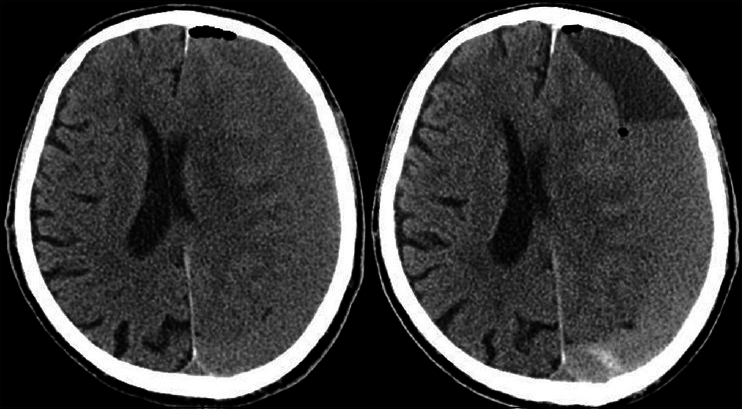
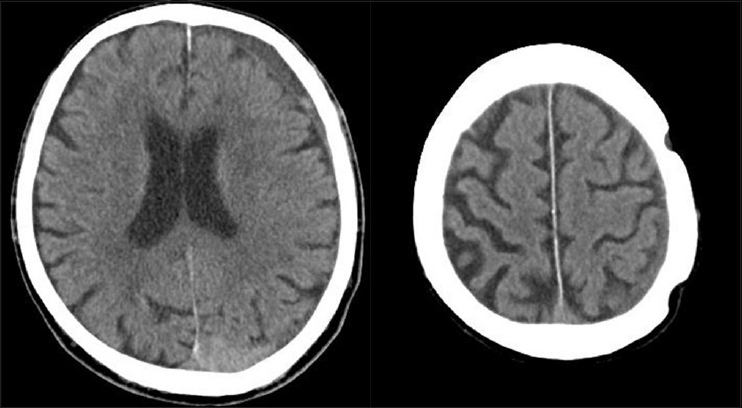
Figure 3
CT scans obtained before (left) and 1 day after (right) the fourth surgery. The tip of the drainage tube is placed on the frontal side and the subdural air collection is reduced compared to the finding after the first surgery (
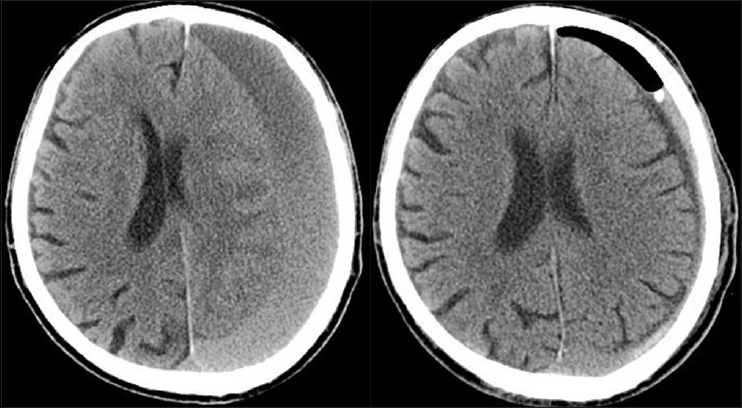
Fifth surgery was supplemented by a simple noninvasive treatment, fibrin glue injection into the hematoma cavity through the drainage tube. Fifth irrigation and drainage through the former parietal burr hole was performed, the hematoma was removed and the cavity thoroughly irrigated, and then a drainage tube was placed anteriorly toward the frontal tip, minimizing the hematoma cavity. On the following day, CT confirmed the collapsed hematoma cavity with minimum air collection [
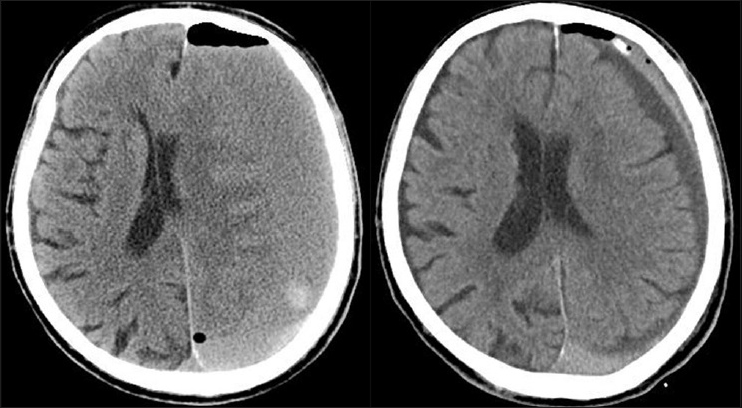
Figure 5
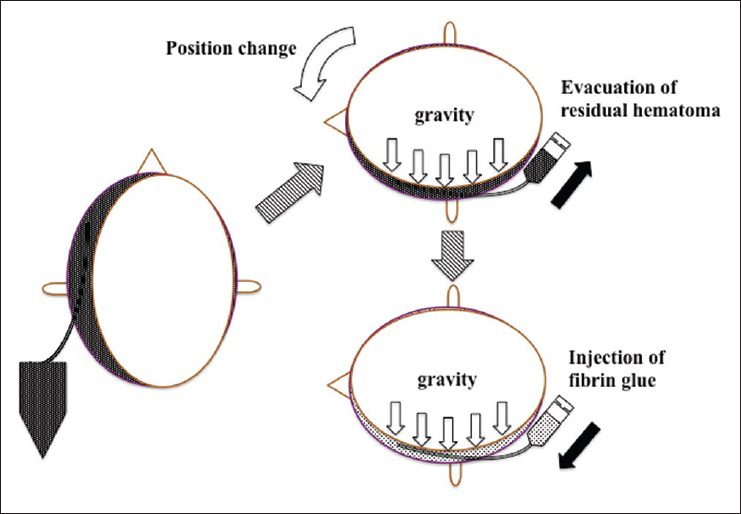
The patient was placed in the left lateral position. Through the drainage tube, 12 ml of the residual hematoma was evacuated, and then they were injected in order of 5 ml of solution A of fibrin glue, few ml of saline, and 5 ml of solution B. Finally, the drainage tube was slowly pulled away during flushing with a few ml of saline
DISCUSSION
CSDH is generally considered to be benign. The goal of the treatment is to return the patients to previous daily life regardless of age, and is successful in most patients. However, the recurrence rates are not particularly low,[
Various therapeutic options with burr hole surgery have been described to reduce the recurrence of CSDH, including postoperative drainage,[
In our case, the antiplatelet therapy was stopped after the second surgery, the hematoma cavity was irrigated with artificial CSF at the third surgery, and the drainage tube was inserted in the frontal direction to reduce postoperative subdural air collection during the fourth surgery. However, none of these interventions was effective. Therefore, some other therapeutic option was required. Possible procedures include craniotomy with removal of the outer membrane,[
Pathological studies of the outer membrane have suggested that the membrane proliferates with vascularization with or without inflammatory change.[
Review of the postoperative course of our case before the fifth surgery showed that the hematoma had a smooth density gradient with no septation, and each surgical evacuation of the hematoma had been effective. These findings implied that large areas of the outer and inner membranes were exposed in the single hematoma cavity after drainage. Therefore, fibrin glue injection could be effective for hemostasis as well as to maintain collapse of the cavity. However, various tactics have been considered to accomplish maximum spread of the limited volume of fibrin glue over the large area of membrane. The subdural dead space should be minimized and deep placement of the drainage tube in the cavity should be advantageous for optimum injection of the fibrin glue. Therefore, the drainage tube was intentionally inserted deeply toward the frontal tip to reduce air collection during the fifth surgery [
The observed effectiveness of fibrin glue injection for the prevention of further recurrence in our case may suggest the pathophysiology of the development and evolution of CSDH. Presumably, a cycle of microbleeding with changes in coagulation and fibrinolysis in the hematoma cavity occurs during proliferation of the outer membrane.[
After the present case, we have had no other patients suffering from refractory CSDH with the need for fibrin glue injection. We recognize the limitation of single case presentation and further study is needed to validate this technique. However, we believe that fibrin glue injection is an effective treatment option for recurrent CSDH. This therapy may depend on optimal placement of the drainage tube with adequate evacuation of hematoma, but is minimally invasive and may be suitable for refractory cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adachi A, Higuchi Y, Fujikawa A, Machida T, Sueyoshi S, Harigaya K. Risk factors in chronic subdural hematoma: Comparison of irrigation with artificial cerebrospinal fluid and normal saline in a cohort analysis. PLoS One. 2014. 9: e103703-
2. Borger V, Vatter H, Oszvald A, Marquardt G, Seifert V, Guresir E. Chronic subdural haematoma in elderly patients: A retrospective analysis of 322 patients between the ages of 65-94 years. Acta Neurochir. 2012. 154: 1549-54
3. Chon KH, Lee JM, Koh EJ, Choi HY. Independent predictors for recurrence of chronic subdural hematoma. Acta Neurochir. 2012. 154: 1541-8
4. Hellwig D, Kuhn TJ, Bauer BL, List-Hellwig E. Endoscopic treatment of septated chronic subdural hematoma. Surg Neurol. 1996. 45: 272-7
5. Karibe H, Kameyama M, Kawase M, Hirano T, Kawaguchi T, Tominaga T. Epidemiology of chronic subdural hematomas. No Shinkei Geka. 2011. 39: 1149-53
6. Kawakami Y, Chikama M, Tamiya T, Shimamura Y. Coagulation and fibrinolysis in chronic subdural hematoma. Neurosurgery. 1989. 25: 25-9
7. Leroy HA, Aboukais R, Reyns N, Bourgeois P, Labreuche J, Duhamel A. Predictors of functional outcomes and recurrence of chronic subdural hematomas. J Clin Neurosci. 2015. 22: 1895-900
8. Liu W, Bakker NA, Groen RJ. Chronic subdural hematoma: A systematic review and meta-analysis of surgical procedures. J Neurosurg. 2014. 121: 665-73
9. Mandai S, Sakurai M, Matsumoto Y. Middle meningeal artery embolization for refractory chronic subdural hematoma. Case report. J Neurosurg. 2000. 93: 686-8
10. Markwalder TM. Chronic subdural hematomas: A review. J Neurosurg. 1981. 54: 637-45
11. Mino M, Nishimura S, Hori E, Kohama M, Yonezawa S, Midorikawa H. Efficacy of middle meningeal artery embolization in the treatment of refractory chronic subdural hematoma. Surg Neurol Int. 2010. 1: 78-
12. Miranda LB, Braxton E, Hobbs J, Quigley MR. Chronic subdural hematoma in the elderly: Not a benign disease. J Neurosurg. 2011. 114: 72-6
13. Misra M, Salazar JL, Bloom DM. Subdural-peritoneal shunt: Treatment for bilateral chronic subdural hematoma. Surg Neurol. 1996. 46: 378-83
14. Nagahori T, Nishijima M, Takaku A. Histological study of the outer membrane of chronic subdural hematoma: Possible mechanism for expansion of hematoma cavity. No Shinkei Geka. 1993. 21: 697-701
15. Nakaguchi H, Tanishima T, Yoshimasu N. Relationship between drainage catheter location and postoperative recurrence of chronic subdural hematoma after burr-hole irrigation and closed-system drainage. J Neurosurg. 2000. 93: 791-5
16. Sato M, Iwatsuki K, Akiyama C, Kumura E, Yoshimine T. Implantation of a reservoir for refractory chronic subdural hematoma. Neurosurgery. 2001. 48: 1297-301
17. Schwarz F, Loos F, Dunisch P, Sakr Y, Safatli DA, Kalff R. Risk factors for reoperation after initial burr hole trephination in chronic subdural hematomas. Clin Neurol Neurosurg. 2015. 138: 66-71
18. Shimamura N, Ogasawara Y, Naraoka M, Ohnkuma H. Irrigation with thrombin solution reduces recurrence of chronic subdural hematoma in high-risk patients: Preliminary report. J Neurotrauma. 2009. 26: 1929-33
19. Takayama M, Terui K, Oiwa Y. Retrospective statistical analysis of clinical factors of recurrence in chronic subdural hematoma: Correlation between univariate and multivariate analysis. No Shinkei Geka. 2012. 40: 871-6
20. Tanaka T, Fujimoto S, Saitoh K, Satoh S, Nagamatsu K, Midorikawa H. Superselective angiographic findings of ipsilateral middle meningeal artery of chronic subdural hematoma in adults. No Shinkei Geka. 1998. 26: 339-47
21. Torihashi K, Sadamasa N, Yoshida K, Narumi O, Chin M, Yamagata S. Independent predictors for recurrence of chronic subdural hematoma: A review of 343 consecutive surgical cases. Neurosurgery. 2008. 63: 1125-9
22. Wada M, Yamakami I, Higuchi Y, Tanaka M, Suda S, Ono J. Influence of antiplatelet therapy on postoperative recurrence of chronic subdural hematoma: A multicenter retrospective study in 719 patients. Clin Neurol Neurosurg. 2014. 120: 49-54