- Department of Neurosurgery, Postgraduate Institute of Medical Education & Research (PGIMER), Chandigarh, India
DOI:10.25259/SNI-38-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Pravin Salunke, Madhivanan Karthigeyan, Puneet Malik. Foramen magnum decompression without bone removal: C1–C2 posterior fixation for Chiari with congenital atlantoaxial dislocation/basilar invagination. 26-Mar-2019;10:38
How to cite this URL: Pravin Salunke, Madhivanan Karthigeyan, Puneet Malik. Foramen magnum decompression without bone removal: C1–C2 posterior fixation for Chiari with congenital atlantoaxial dislocation/basilar invagination. 26-Mar-2019;10:38. Available from: http://surgicalneurologyint.com/surgicalint-articles/9246/
Abstract
Background: Atlantoaxial dislocation (AAD) and basilar invagination (BI) may coexist with Chiari malformations (CM) and a small posterior fossa volume. These are typically treated with craniovertebral junction fusion and foramen magnum decompression (FMD). Here, we evaluated whether C1–C2 posterior reduction and fixation (which possibly opens up the ventral foramen magnum) would effectively treat AAD and CM without additionally performing FMD.
Methods: This is a retrospective analysis of 38 patients with BI, AAD, and CM who underwent C1–C2 posterior reduction and fusion without FMD. Baseline and follow-up clinical, demographic, and radiological data were evaluated.
Results: The vast majority of patients (91.9%) improved both clinically and radiographically following C1–C2 fixation alone; none later required direct FMD. Notably, AAD was irreducible in 25 (65.8%) patients. Preoperatively, syringomyelia was present in 28 (73.7%) patients and showed resolution. In 3 (8.1%) patients, resolution of syrinxes did not translate into clinical improvement. Of interest, 5 patients who sustained inadvertent dural lacerations exhibited transient postoperative neurological worsening.
Conclusions: Posterior C1–C2 distraction and fusion alone effectively treated AAD, BI, accompanied by CM. The procedure sufficiently distracted the dens, reversed dural tenting, and restored the posterior fossa volume while relieving ventral brainstem compression making FMD unnecessary. Surgeons should, however, be aware that inadvertent dural lacerations might contribute to unwanted neurological deterioration.
Keywords: Atlantoaxial dislocation, basilar invagination, C1–C2 distraction, chiari, foramen magnum decompression, syrinx, ventral decompression
INTRODUCTION
Chiari malformations (CM), associated with a reduced volume of the posterior fossa, are typically treated with foramen magnum decompression (FMD) (i.e., to enlarge the posterior fossa volume).[
In this study, we, therefore, evaluated whether C1–C2 distraction and arthrodesis obviated the need for additional FMD.
MATERIALS AND METHODS
Patient data
In this retrospective analysis (2015–2017), 38 patients with AAD/BI and CM underwent C1–C2 fixation without FMD (neither bony nor dural decompression). Patients averaged 40.5 years of age and demonstrated a mean modified Japanese Orthopaedic Association (JOA) score at the time of presentation of 11.3 [
Computed tomography (CT) and CT angiography (CTA): Preoperative findings
Preoperative CT studies were utilized to evaluate the craniovertebral junction, while CTA additionally documented any anomalous vertebral arteries [
Magnetic resonance imaging (MRI) findings
MRI confirmed the diagnosis of CM, syringomyelia, and the degree of cervicomedullary compression. For those with an intact C1 arch, the extent of tonsillar descent of at least 5 mm below the FM while for those with assimilated C1 arches, any descent of the tonsils below the posterior arch of C1 was considered CM.
Perioperative and operative considerations
About 48-h before surgery, cervical traction was applied. The AAD was reducible in 13 (34.2%) patients but was irreducible in 25 (65.8%) who underwent intraoperative reduction.
All patients then had C1–C2 posterior reduction and fusion.[
Clinical and MR/CT follow-up
At 6 postoperative months, the thin slice CT documented bony fusion, while the MRI scans documented the extent of cephalad cerebellar tonsil migration, the degree of cerebrospinal fluid (CSF) flow across foramen magnum, and whether there was the resolution of the syrinxes.
Statistical analysis
Statistical Package for the Social Sciences version 21 (IBM Corp., New York, USA) was used for the data analysis. The mean preoperative and follow-up modified JOA score were compared using the paired t-test. P < 0.05 was considered significant.
RESULTS
After C1–C2 fusion, satisfactory reduction and realignment were achieved in all cases [Figures
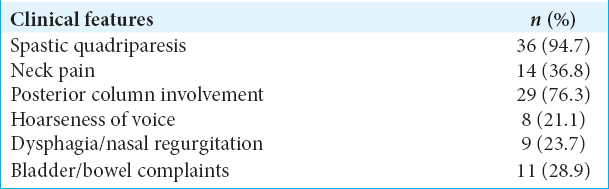
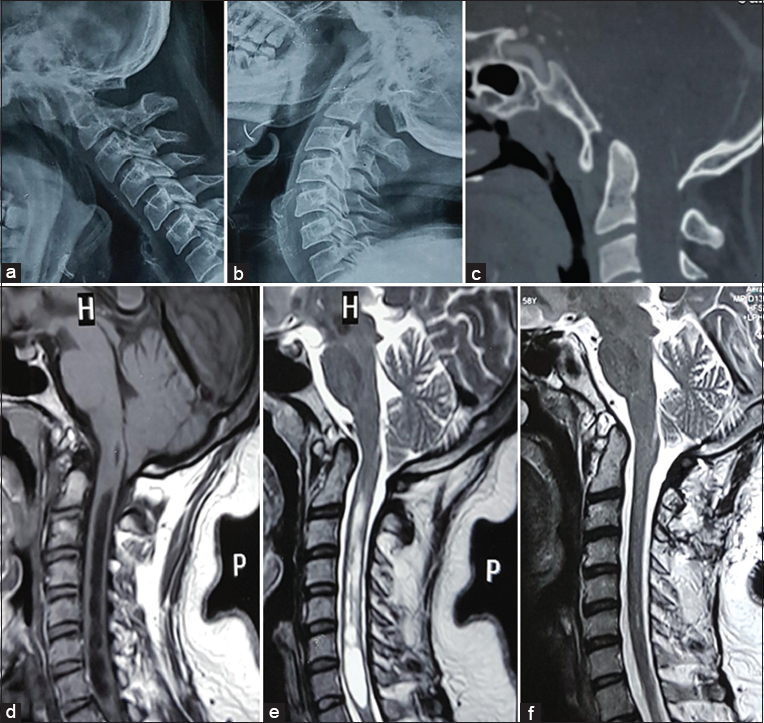
Figure 1
(a) Preoperative midsagittal computed tomography (CT); basilar invagination and atlantoaxial dislocation (AAD) with segmentation defects. (b) Postoperative CT; reduction of deformity with intact foramen magnum margin. (c) Preoperative T2-weighted sagittal magnetic resonance imaging; Chiari malformations and syringomyelia. (d) Follow-up imaging (6-months) shows significant resolution of the syrinx.
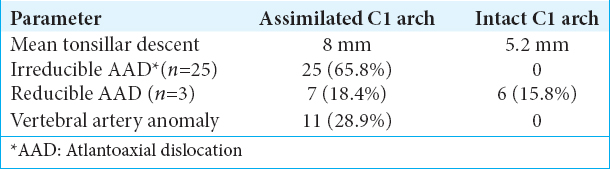
Figure 2
(a) Computed tomography (CT) shows basilar invagination and atlantoaxial dislocation with segmentation defects. (b) Postoperative CT after distraction and realignment of dens. (c) T1-weighted magnetic resonance imaging (MRI) shows Chiari with crowding of posterior fossa structures. (d and e) Postoperative MRI; T1-weighted (d) and T2-weighted (e) show ascent of tonsils and the opening of cerebrospinal fluid space.
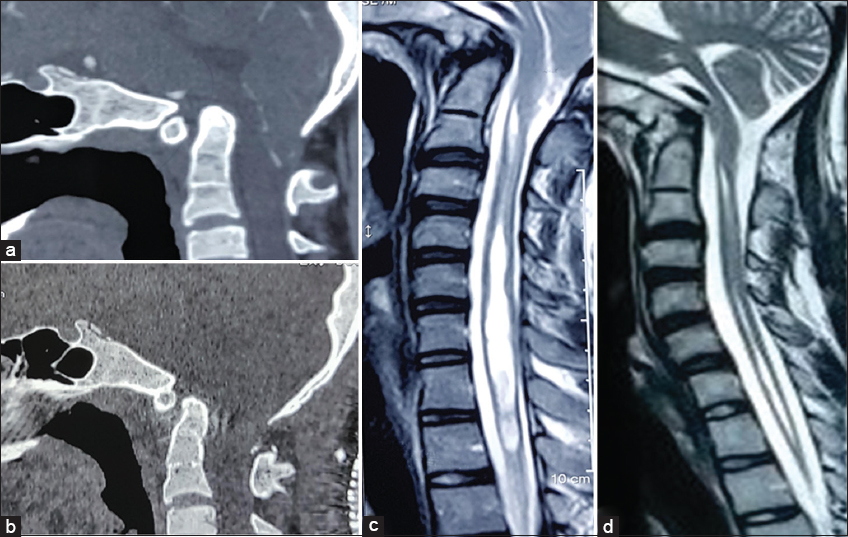
Figure 3
(a and b) Preoperative dynamic radiographs show reducible atlantoaxial dislocation (AAD). (c) Midsagittal computed tomography demonstrates basilar invagination and AAD; C1 is assimilated. (d and e) T1 (d) and T2 (e) weighted magnetic resonance imaging (MRI); Chiari with crowded posterior fossa and syrinx. (f) Follow-up MRI (12 months) shows ascent of tonsils and striking resolution of the syrinx.
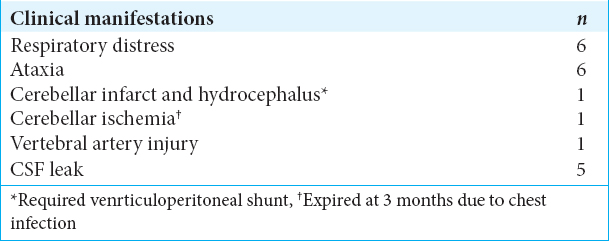
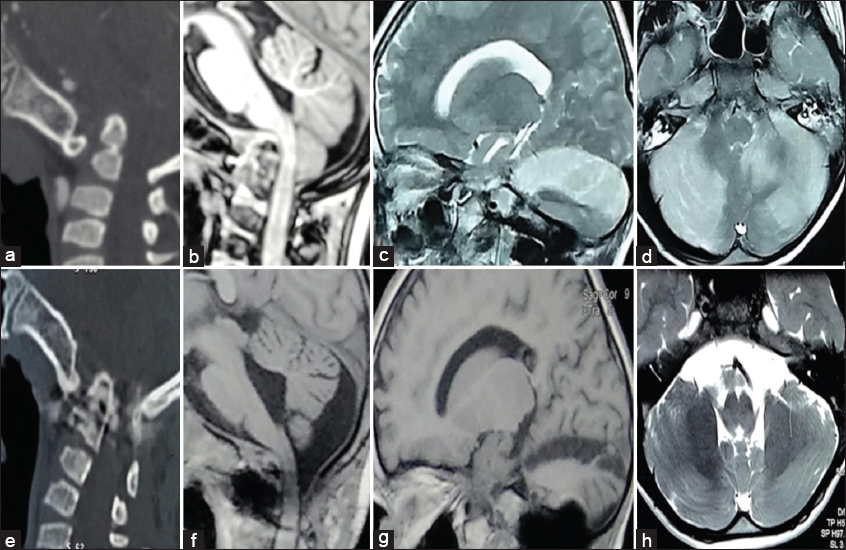
Immediate postoperative complications
Six patients exhibited transient neurological worsening on postoperative days 2–3 [
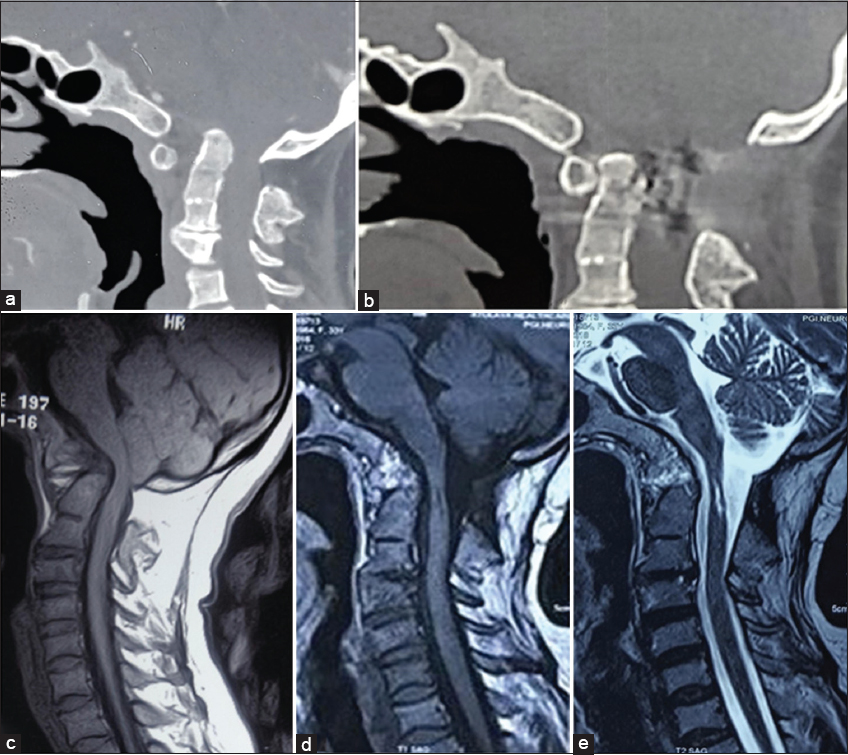
Figure 4
Postoperative course with the inadvertent dural opening. Preoperative computed tomography (CT) (a) depicts BI with atlantoaxial dislocation; T1-weighted magnetic resonance imaging (MRI) (b) shows Chiari. (c and d) MRI show acute cerebellar infarcts in the postoperative period. (e) Postoperative CT shows a reduction of the deformity. (f-h) On follow-up, there is the ascent of tonsils with the good restoration of CSF space (f) and resolving infarcts (g-h).
Long-term outcome
Fusion was documented in 37 of 38 patients from 11 to 40 months postoperatively; of interest, none required additional FMD. The mean improved modified JOA score of 13.6 (P < 0.01) was seen in 34 patients (91.9%) who showed neurological improvement. Their MRI studies also documented ascent of the tonsils with the restoration of CSF space and resolution of syrinxes [Figures
DISCUSSION
AAD/BI with CM was successfully managed in this series utilizing posterior C1–C2 reduction and fusion without FMD.[
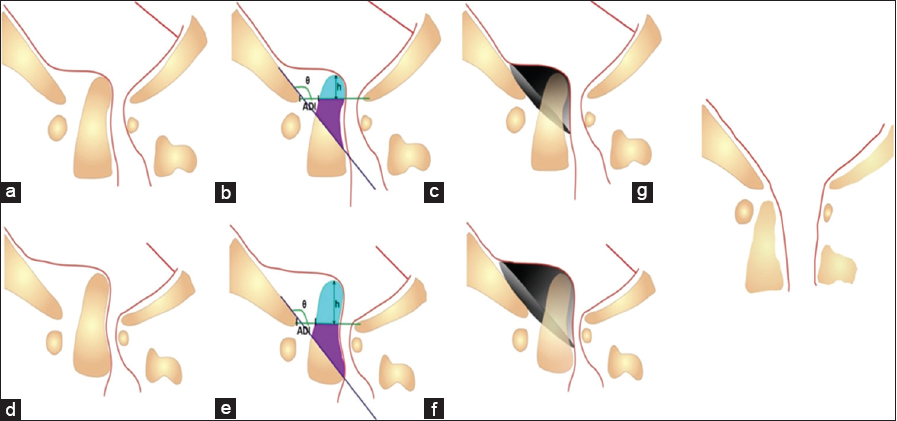
Mathematical formula to estimate the reduction in posterior fossa volume secondary to encroachment by dens in AAD/BI and the rationale of surgery
The absolute volume of conical dens that violates the Wackenheim’s clivus canal line is given by the formula πd2 [VD/12 + tan(180-θ)·d/8], d being the diameter of dens at the level of FM and VD, the height of dens that invaginates above FM. The effective reduction in posterior fossa volume is far greater than the absolute volume of dens and is approximately π [VD·cos(180-θ) + ADI·sin(180-θ)]3/3·tan(180-θ) where θ is the Boogaard’s angle and ADI is the atlantodental interval [
Figure 5
Dural indentation in basilar invagination (BI) with Chiari. (a-c), moderate and (d-f), severe dislocation. A portion of dens that lies above foramen magnum (FM) and that violates Wackenheim’s line is marked in different colors (b and e). This causes ventral compression. However, the actual volume of posterior fossa (PF) (gray cone) that is reduced is far more than the volume of dens alone (c and f). C1–C2 distraction and reduction not only relieves ventral compression but also restores PF vol. PF volume is given by Boogaard’s angle (θ), atlantodental interval and height of dens (vertical dislocation) that invaginates above FM (h). (g) Normal anatomy.
CONCLUSIONS
C1–C2 fusion without FMD adequately addressed AAD, BI with CM in 38 patients in this series. Distraction, reduction, and C1–C2 arthrodesis increased the posterior fossa volume resulting in adequate ventral cervicomedullary junction decompression without the need for additional FMD.
Compliance with ethical standards
The procedures performed were in accordance with the ethical standards of the Institutional Ethics Committee and with the 1975 Helsinki declaration and its later amendments.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Behari S, Kalra SK, Kiran Kumar MV, Salunke P, Jaiswal AK, Jain VK. Chiari I malformation associated with atlanto-axial dislocation: Focussing on the anterior cervico-medullary compression. Acta Neurochir (Wien). 2007. 149: 41-50
2. Goel A, Sathe P, Shah A. Atlantoaxial fixation for basilar invagination without obvious atlantoaxial instability (Group B basilar invagination): Outcome analysis of 63 surgically treated cases. World Neurosurg. 2017. 99: 164-70
3. Goel A. Is atlantoaxial instability the cause of chiari malformation? Outcome analysis of 65 patients treated by atlantoaxial fixation. J Neurosurg Spine. 2015. 22: 116-27
4. Kennedy BC, Kelly KM, Phan MQ, Bruce SS, McDowell MM, Anderson RC. Outcomes after suboccipital decompression without dural opening in children with chiari malformation Type I. J Neurosurg Pediatr. 2015. 16: 150-8
5. Salunke P, Sahoo S, Khandelwal NK, Ghuman MS. Technique for direct posterior reduction in irreducible atlantoaxial dislocation: Multi-planar realignment of C1-2. Clin Neurol Neurosurg. 2015. 131: 47-53
6. Salunke P, Sahoo SK, Deepak AN, Ghuman MS, Khandelwal NK. Comprehensive drilling of the C1-2 facets to achieve direct posterior reduction in irreducible atlantoaxial dislocation. J Neurosurg Spine. 2015. 23: 294-302
7. Salunke P, Sahoo SK, Deepak AN, Khandelwal NK. Redefining congenital atlantoaxial dislocation: Objective assessment in each plane before and after operation. World Neurosurg. 2016. 95: 156-64
8. Salunke P, Sahoo SK, Sood S, Mukherjee KK, Gupta SK. Focusing on the delayed complications of fusing occipital squama to cervical spine for stabilization of congenital atlantoaxial dislocation and basilar invagination. Clin Neurol Neurosurg. 2016. 145: 19-27
9. Wang S, Wang C, Yan M, Zhou H, Jiang L. Syringomyelia with irreducible atlantoaxial dislocation, basilar invagination and chiari I malformation. Eur Spine J. 2010. 19: 361-6
10. Wang Z, Wang X, Jian F, Zhang C, Wu H, Chen Z. The changes of syrinx volume after posterior reduction and fixation of basilar invagination and atlantoaxial dislocation with syringomyelia. Eur Spine J. 2017. 26: 1019-27