- Pars Advanced and Minimally Invasive Medical Manners Research Center, Pars Hospital, Iran University of Medical Sciences, Tehran, Iran.
DOI:10.25259/SNI_478_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abolfazl Rahimizadeh, Nima Mohsenikabir, Naser Asgari. Iatrogenic lumbar giant pseudomeningocele: A report of two cases. 01-Nov-2019;10:213
How to cite this URL: Abolfazl Rahimizadeh, Nima Mohsenikabir, Naser Asgari. Iatrogenic lumbar giant pseudomeningocele: A report of two cases. 01-Nov-2019;10:213. Available from: http://surgicalneurologyint.com/surgicalint-articles/9731/
Abstract
Background:Iatrogenic lumbar pseudomeningoceles are an uncommon complication of lumbar spinal surgeries. This pathology is an extradural, encapsulated, and cerebrospinal fluid collection which develops as a consequence of an inadvertent, unrepaired dural tear. If a pseudomeningocele grows beyond 8 cm in length, it may be classified as “giant.”
Case Description:Two adult females with giant pseudomeningoceles due to remote lumbar laminectomy were presented. Both patients were surgically managed.
Conclusion:Iatrogenic lumbar giant pseudomeningocele is rare. Notably, their surgical management is similar to that utilized to treat routine pseudomeningoceles.
Keywords: Complication, Dural tear, Giant pseudocyst, Iatrogenic pseudomeningocele, Incidental durotomy, Lumbar discectomy, Lumbar laminectomy
INTRODUCTION
Iatrogenic pseudomeningocele following spinal surgery is defined as an extradural cystic collection of cerebrospinal fluid (CSF) without a dural covering that results from a breach in the dural-arachnoid layer.[
Size of pseudomeningoceles
Most lumbar pseudomeningoceles are below 5 cm in size, but rarely, they may become “giant” when over 8 cm.[
CASE DESCRIPTION
Case 1
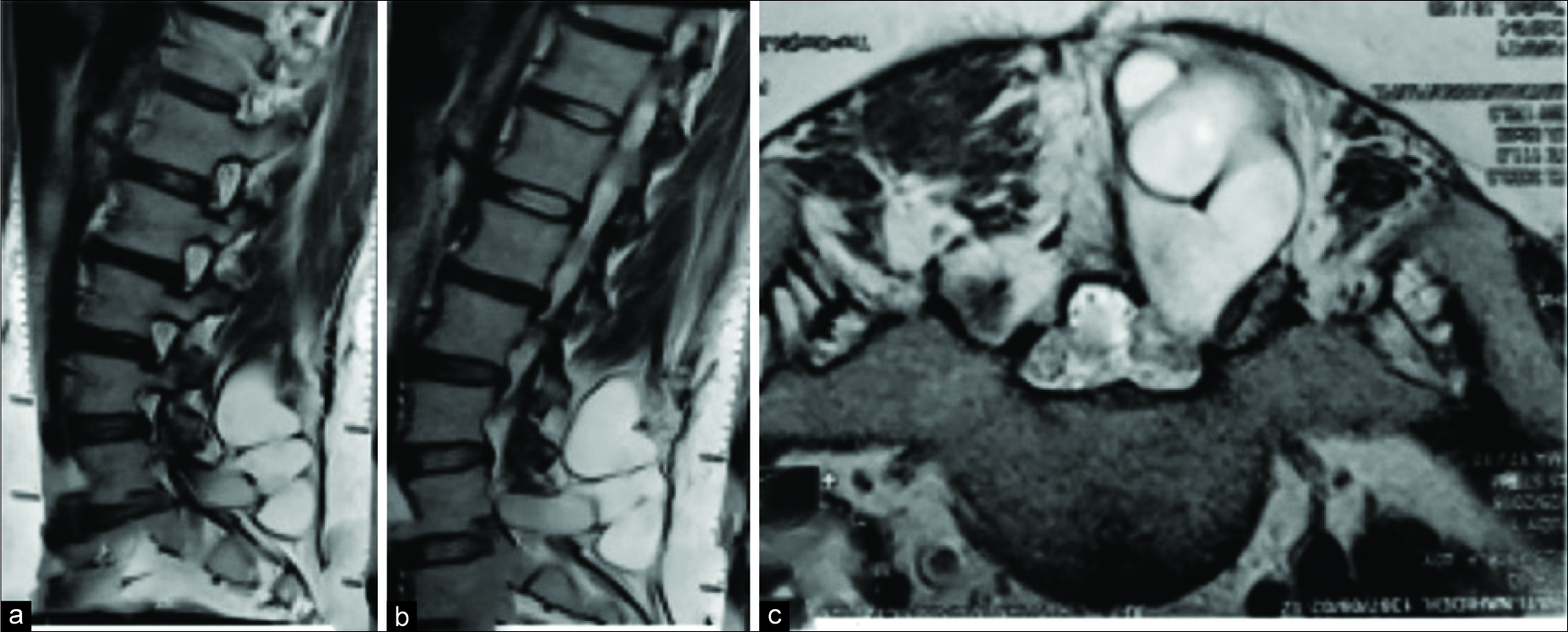
A 30-year-old female had a lumbar laminectomy for a left-sided L5-S1 disc herniation. One year later, she developed recurrent lumbar complaints thought to be due to a recurrent disc herniation. However, the preoperative magnetic resonance imaging (MRI) showed a large/giant pseudomeningocele that extended from L4 to S2 (e.g., total length of 8.9 cm) [
Case 2
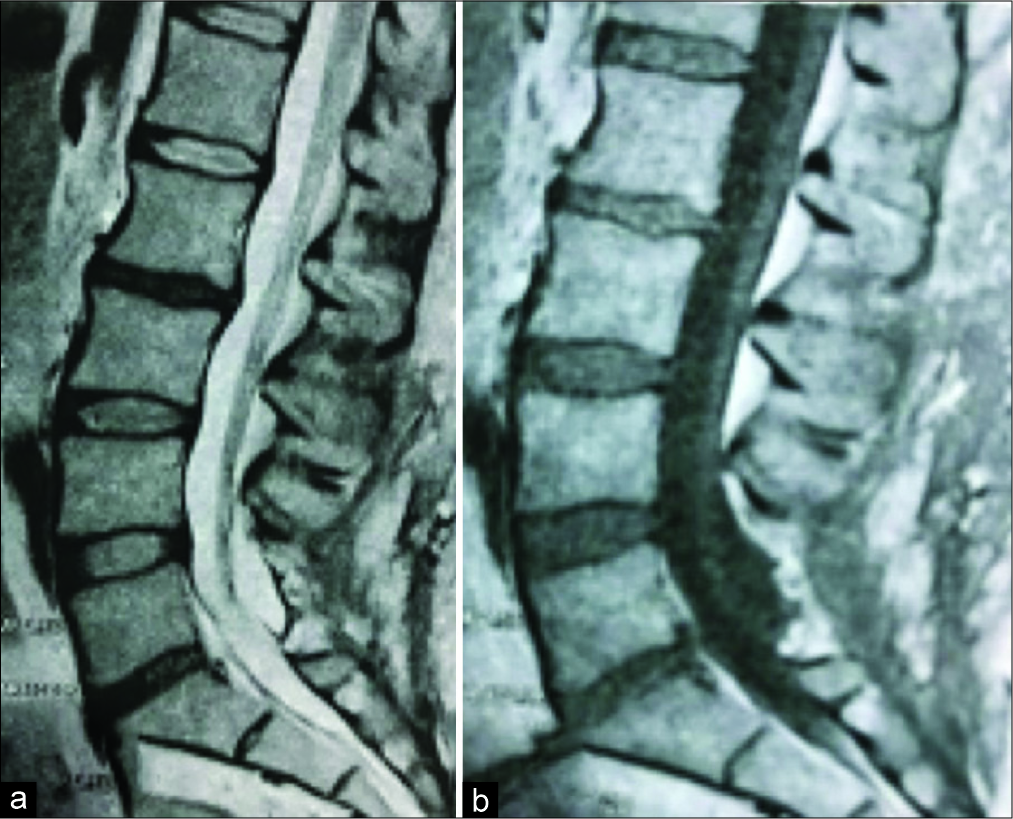
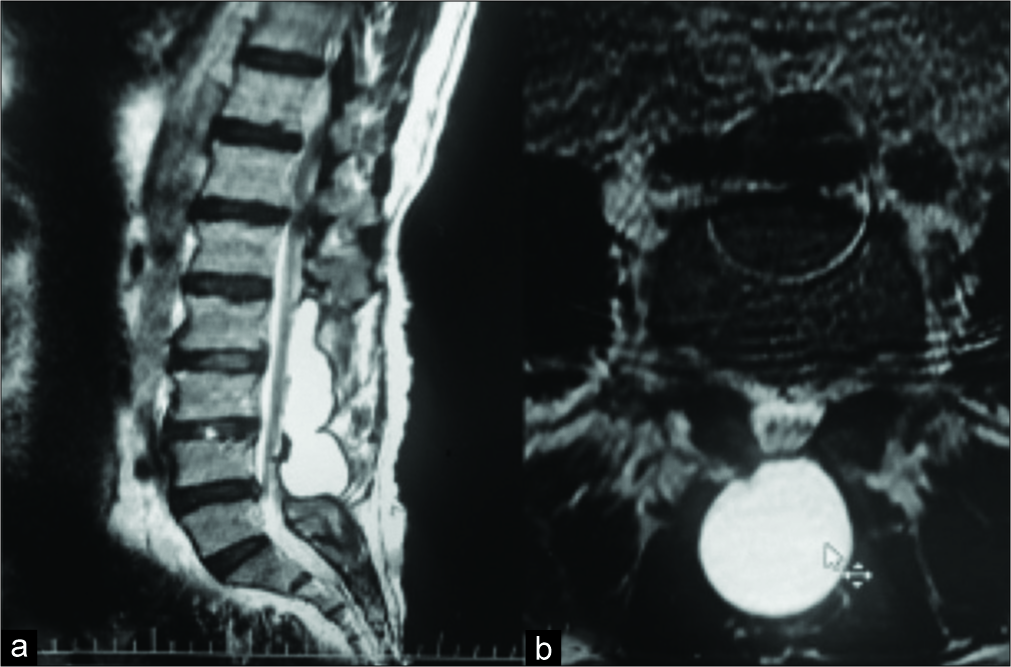
A 51-year-old female originally had a multilevel laminectomy for lumbar stenosis. Eighteen months later, she presented with a history of 3 months of intractable lower back pain and right L4. The lumbar MRI showed a giant pseudomeningocele extending from L2 to L5; it was 12 cm in length, arising from a defect at the L3-L4 level [
DISCUSSION
Unnoticed dural tears with an intact arachnoid which possess a ball valve mechanism will result in the development of a true cyst lined with arachnoid tissue; this iatrogenic cyst is a “true meningocele.”[
Imaging
In plain radiographs, erosion of the surrounding bones might be seen for long-standing cases. Rarely, the wall of the cyst may undergo ossification.[
Management
For asymptomatic cases, one may wait for spontaneous resolution of the pseudomeningoceles; this may occur within 3 months to a few years following the diagnosis.[
CONCLUSION
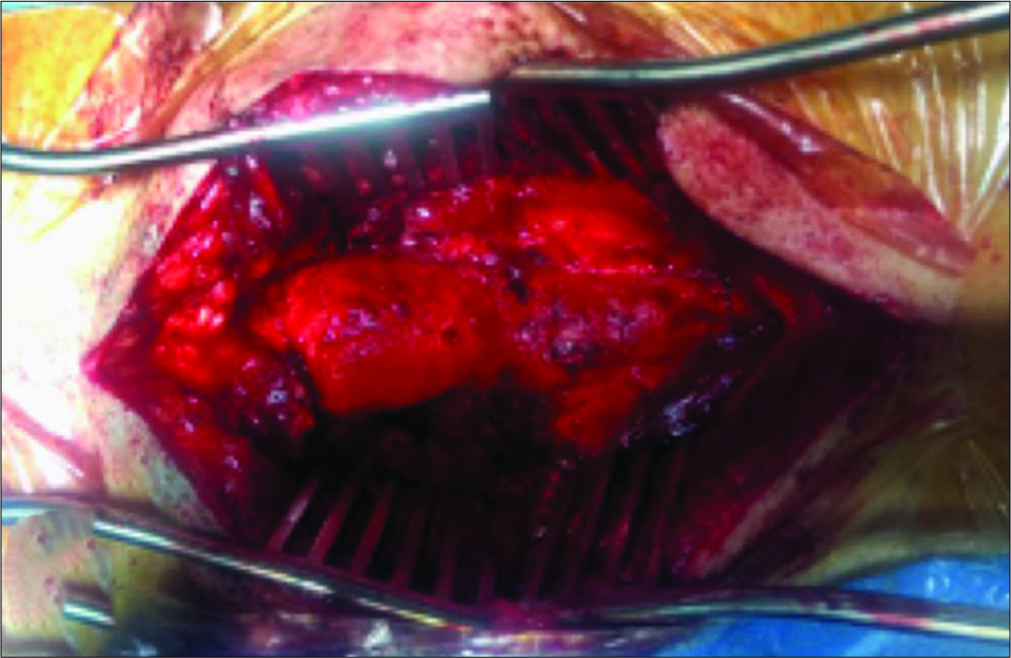
Incidental dural tears with CSF leakage during lumbar laminectomy should be properly addressed, as if ignored or not found, they may result in the formation of a pseudomeningocele. Lumbar pseudomeningoceles may become symptomatic years later (e.g., LBP/radiculopathy) and warrant appropriate lumbar surgical intervention consisting of localization of the nerve roots extruding from the dural sac, delivery of the roots intradurally, and closure of the dural defect.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Edrus SA, Mohamed Mukari SA, Ganesan D, Ramli N. Ossified lumbar pseudomeningocele: Imaging findings. Spine J. 2011. 11: 796-7
2. Enke O, Dannaway J, Tait M, New CH. Giant lumbar pseudomeningocele after revision lumbar laminectomy: A case report and review of the literature. Spinal Cord Ser Cases. 2018. 4: 82-
3. Hyndman OR, Gerber WF. Spinal extradural cysts, congenital and acquired; report of cases. J Neurosurg. 1946. 3: 474-86
4. Macki M, Lo SF, Bydon M, Kaloostian P, Bydon A. Post-surgical thoracic pseudomeningocele causing spinal cord compression. J Clin Neurosci. 2014. 21: 367-72
5. Rahimizadeh A, Kaghazchi M, Rahimizadeh A. Post-laminectomy pseudomeningocele: Report of three cases and review of the literature. World Spinal Column J. 2014. 4: 103-8
6. Rahimizadeh A, Soufiani H, Rahimizadeh S. Remote cervical pseudomeningocele following anterior cervical corpectomy and fusion: Report of a case and review of the literature. Int J Spine Surg. 2016. 10: 36-
7. Solomon P, Sekharappa V, Krishnan V, David KS. Spontaneous resolution of postoperative lumbar pseudomeningoceles: A report of four cases. Indian J Orthop. 2013. 47: 417-21
8. Weng YJ, Cheng CC, Li YY, Huang TJ, Hsu RW. Management of giant pseudomeningoceles after spinal surgery. BMC Musculoskelet Disord. 2010. 11: 53-







Jim Ausman
Posted December 1, 2019, 7:00 am
Thank you for sending SNI these case reports and your excellent results