- Department of Neurologic Surgery, Mayo Clinic, Rochester, MN, USA
- Department of Neurosurgery, Tokyo Metropolitan Police Hospital, Tokyo, Japan
- Department of Pathology, Tokyo Metropolitan Police Hospital, Tokyo, Japan
Correspondence Address:
Satoshi Kiyofuji
Department of Neurosurgery, Tokyo Metropolitan Police Hospital, Tokyo, Japan
DOI:10.4103/sni.sni_344_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Satoshi Kiyofuji, Christopher S. Graffeo, Munehiro Yokoyama, Shigeo Sora. Intramedullary and intratumoral hemorrhage in spinal hemangioblastoma: Case report and review of literature. 04-Dec-2018;9:250
How to cite this URL: Satoshi Kiyofuji, Christopher S. Graffeo, Munehiro Yokoyama, Shigeo Sora. Intramedullary and intratumoral hemorrhage in spinal hemangioblastoma: Case report and review of literature. 04-Dec-2018;9:250. Available from: http://surgicalneurologyint.com/?post_type=surgicalint_articles&p=9112
Abstract
Background:Intramedullary hemorrhages involving spinal hemangioblastomas are rare. They are frequently associated with devastating neurologic outcomes, despite with emergent surgical intervention. Here, we presented an example of an intramedullary hemorrhage occurring in a spinal hemangioblastoma, where the patient markedly improved with surgery. Additionally, the appropriate literature was reviewed (including intraoperative video).
Case Description:A 49-year-old female with a 4-year history of tingling in the left lower extremity presented with vomiting, stepwise worsening of bilateral scapular pain, new upper motor neuron signs, and severe sensory loss bilaterally below C4 on the left and T4 on the right. The magnetic resonance imaging demonstrated a well-circumscribed, uniformly enhancing intramedullary tumor at the C2 level with hyperintensity on the T2 study consistent with acute hemorrhage and cord edema. An urgent C2 laminectomy was performed for gross total tumor resection. Intraoperatively, intramedullary hemorrhage was identified anterior to the tumor mass and was confirmed histopathologically. Postoperatively, the patient had no new sensorimotor deficits and fully recovered within two postoperative months.
Conclusions:Patients presenting with acute intramedullary hemorrhage within hemangioblastomas of the spinal cord may demonstrate significant postoperative neurological recovery.
Keywords: Hemangioblastoma, intramedullary hemorrhage, intramedullary spine tumor, intratumor hemorrhage, isolated spine hemangioblastoma
INTRODUCTION
Hemangioblastomas are the third most frequent spinal cord tumors after ependymomas and astrocytomas and account for 2–15% of all intramedullary tumors.[
CASE PRESENTATION
Patient history
A 49-year-old female presented with 1 week of bilateral scapular pain, and 1 day of worsening of the scapular pain accompanied by vomiting. Her neurological examination revealed no gross weakness but moderate dysesthesias (5/10) below the C4 spinal level on the left, and T4 on the right. Vibratory sensation was decreased in both lower extremities, left more than right, and she exhibited diffuse hyperreflexia throughout the upper and lower extremities.
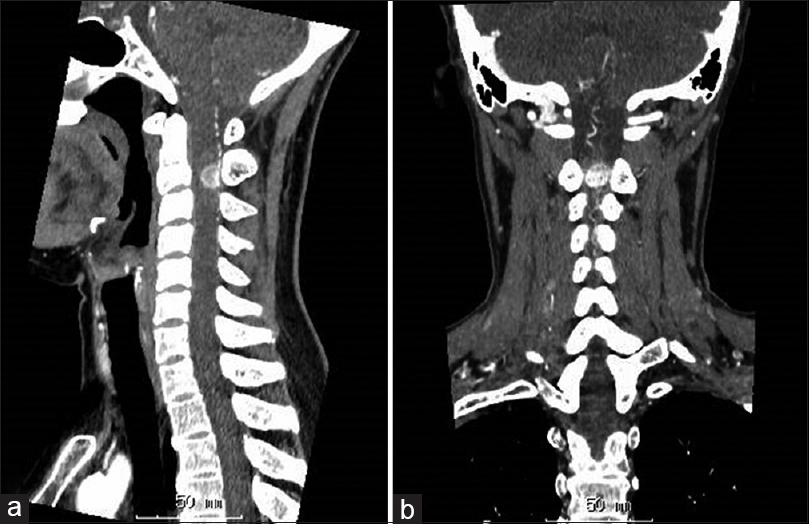
MR and computed tomography imaging
The cervical magnetic resonance imaging (MRI) demonstrated a uniformly contrast-enhancing mixed -density intramedullary spinal tumor, with confluent T2 hyperintensity noted from the upper cervical spine to the T1 level. A region of low signal intensity on T2* was identified within and extending from the anterior limit of the tumor, suggestive of acute hemorrhage into an intramedullary hemangioblastoma [Figures
Surgery
The patient underwent an immediate C1–C3 laminectomy performed under microscope visualization and with intraoperative monitoring (e.g., somatosensory-evoked potential and motor-evoked potential monitoring).
Upon opening of the arachnoid, the tumor was immediately apparent on the dorsal surface of the spinal cord, associated with multiple neoplastic vessels. Indocyanine green (ICG) angiography was performed (15 mg IV) and identified five major feeding arteries and two draining veins. Temporary clips were applied to the feeding arteries, and the operation was paused for 10 min to confirm stability of the electrical potentials. Vessels were then cut and cauterized, followed by circumferential resection of tumor. Frank intramedullary hemorrhage was noted anterior to the tumor itself and removed. Repeat ICG injection was negative for residual circulation to the tumor and demonstrated only subtle distal drainage through the remaining draining vein, which was cauterized. Ultimately, a complete en-bloc resection was achieved [
Postoperative course
Postoperatively, the patient demonstrated no motor deficit, but an increased severity of the left upper and lower extremity sensory disturbance. Successive postoperative MRI studies demonstrated complete resection of the tumor [
Histology
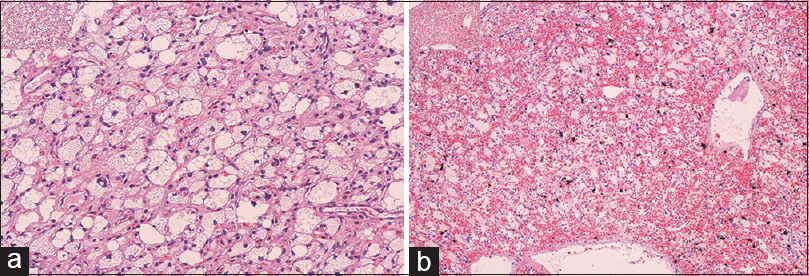
The final histopathology was consistent with a hemangioblastoma with intratumor hemorrhage (WHO grade I; Figure
DISCUSSION
A patient with a cervical spinal hemangioblastoma accompanied by an acute intramedullary hemorrhage had preserved motor function but a severe residual sensory deficit below the T5 level following surgical decompression. Roonprapunt et al. described 19 patients with intramedullary spine hemangioblastomas, accompanied by edema, syrinx formation, and/or tumor cysts presenting in an indolent fashion over 29.8 months; the patients did well following surgical resection/decompression.[
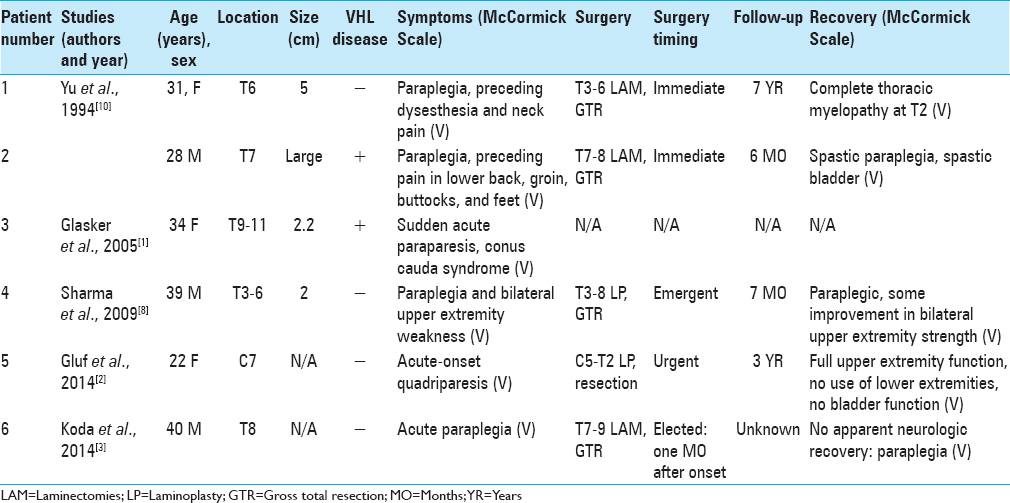
When these lesions hemorrhage, it typically occurs into the subarachnoid space rather than within the cord itself (e.g., intramedullary). Five prior reports describe six patients with intramedullary hemangioblastomas presenting with intratumoral hemorrhages [
Surgical indications for intramedullary hemangiobastomas with acute intratumoral hemorrhages
It is unclear whether patients with spinal intramedullary hemorrhages within hemangioblastomas benefit from surgery. Excepting one report from Koda et al.,[
Steiger et al. conclude in their review of 20 patients that the benefits of early surgery for patients with moderate-to-severe deficits were effectively zero.[
CONCLUSIONS
Intramedullary hemorrhages within spine hemangioblastomas are rare. Surgery is optimized by utilizing intraoperative monitoring and vascular visualization techniques (e.g., intraoperative ICG angiography). This case and literature review demonstrated that surgery may result in favorable postoperative neurological outcomes.
DISCLOSURE
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Glasker S, Van Velthoven V. Risk of hemorrhage in hemangioblastomas of the central nervous system. Neurosurgery. 2005. 57: 71-6
2. Gluf WM, Dailey AT. Hemorrhagic intramedullary hemangioblastoma of the cervical spinal cord presenting with acute-onset quadriparesis: Case report and review of the literature. J Spinal Cord Med. 2014. 37: 791-4
3. Koda M, Mannoji C, Itabashi T, Kita T, Murakami M, Yamazaki M. Intramedullary hemorrhage caused by spinal cord hemangioblastoma: A case report. BMC Res Notes. 2014. 7: 823-
4. Lonser RR, Oldfield EH. Spinal cord hemangioblastomas. Neurosurg Clin N Am. 2006. 17: 37-44
5. Montano N, Papacci F, Trevisi G, Fernandez E. Factors affecting functional outcome in patients with intramedullary spinal cord tumors: Results from a literature analysis. Acta Neurol Belg. 2017. 117: 277-82
6. Roonprapunt C, Silvera VM, Setton A, Freed D, Epstein FJ, Jallo GI. Surgical management of isolated hemangioblastomas of the spinal cord. Neurosurgery. 2001. 49: 321-7
7. Samartzis D, Gillis CC, Shih P, O’Toole JE, Fessler RG. Intramedullary spinal cord tumors: Part I-epidemiology, pathophysiology, and diagnosis. Global Spine J. 2015. 5: 425-35
8. Sharma GK, Kucia EJ, Spetzler RF. Spontaneous intramedullary hemorrhage of spinal hemangioblastoma: Case report. Neurosurgery. 2009. 65: E627-8
9. Steiger HJ, Turowski B, Hanggi D. Prognostic factors for the outcome of surgical and conservative treatment of symptomatic spinal cord cavernous malformations: A review of a series of 20 patients. Neurosurg Focus. 2010. 29: E13-
10. Yu JS, Short MP, Schumacher J, Chapman PH, Harsh GRt. Intramedullary hemorrhage in spinal cord hemangioblastoma. Report of two cases. J Neurosurg. 1994. 81: 937-40