- Department of Neurosurgery, Nanoori Suwon Hospital, Suwon, Korea
- Department of Neurosurgery, Nanoori Hospital, Seoul, Korea
- Department of Neurosurgery, Nanoori Incheon Hospital, Incheon, Korea
- Department of Nanoori Medical Research, Nanoori Hospital, Seoul, Korea
Correspondence Address:
Nitin Adsul
Department of Nanoori Medical Research, Nanoori Hospital, Seoul, Korea
DOI:10.4103/sni.sni_262_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hyeun Sung Kim, Nitin Adsul, Yoon Seok Ju, Ki Joon Kim, Sung Ho Choi, Jeong Hoon Kim, Sung Kyun Chung, Jeong-Hoon Choi, Jee-Soo Jang, Il-Tae Jang, Seong-Hoon Oh, Jae Eun Park, Sol Lee. Lumbar chronic subdural hematoma mimicking an intradural extramedullary tumor: A case report. 26-Sep-2017;8:231
How to cite this URL: Hyeun Sung Kim, Nitin Adsul, Yoon Seok Ju, Ki Joon Kim, Sung Ho Choi, Jeong Hoon Kim, Sung Kyun Chung, Jeong-Hoon Choi, Jee-Soo Jang, Il-Tae Jang, Seong-Hoon Oh, Jae Eun Park, Sol Lee. Lumbar chronic subdural hematoma mimicking an intradural extramedullary tumor: A case report. 26-Sep-2017;8:231. Available from: http://surgicalneurologyint.com/surgicalint-articles/lumbar-chronic-subdural-hematoma-mimicking-an-intradural-extramedullary-tumor-a-case-report/
Abstract
Background:Chronic spinal subdural hematomas are extremely rare with only 28 cases reported in the literature. Nevertheless, they should be considered among the differential diagnoses for spinal intradural/extramedullary lesions.
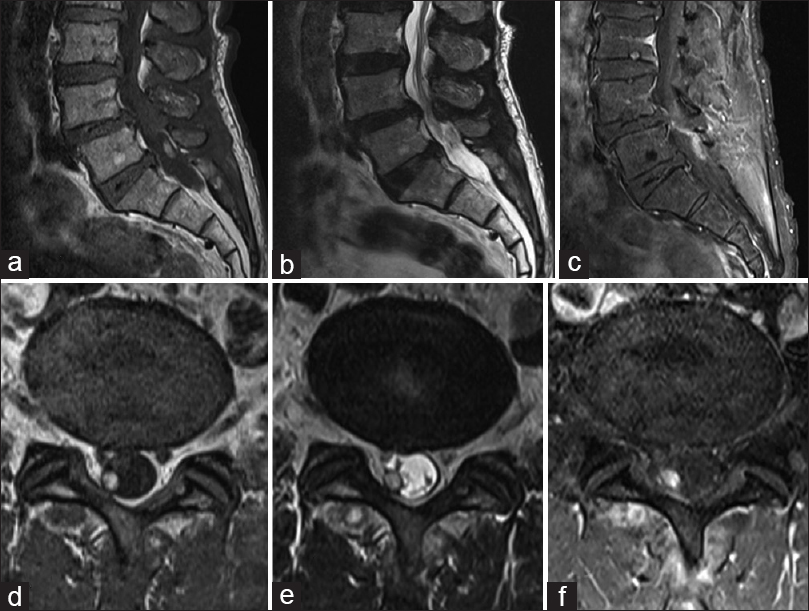
Case Report:A 65-year-old male presented with progressive back pain and right S1 radiculopathy. Magnetic resonance imaging scan revealed a right-sided posterolateral intradural/extramedullary lesion at the L5–S1 level. It was hyperintense on T1 and hypointense on T2-weighted images; on the short TI inversion recovery sequence it was hyperintense. The lesion was excised through a right L5 hemilaminectomy, and the patient was neurologically intact postoperatively. Histopathology revealed a chronic subdural hematoma.
Conclusion:Chronic spinal subdural hematoma can mimic intradural extramedullary spinal tumors even in the absence of trauma and/or coagulopathies.
Keywords: Chronic, intradural extramedullary tumor, spinal subdural hematoma
INTRODUCTION
Spinal subdural hematomas (SDHs) are rare, accounting for only 4.1% of all spinal hemorrhages.[
CASE REPORT
Clinical and radiographic presentation
In the absence of trauma or a history of coagulopathy, a 65-year-old male presented with a progressive right lower extremity L5/S1 radiculopathy.
On physical examination, straight leg raising was positive on the right side at 70 degrees and the right Achilles response was absent; there was no sensory or motor deficit.
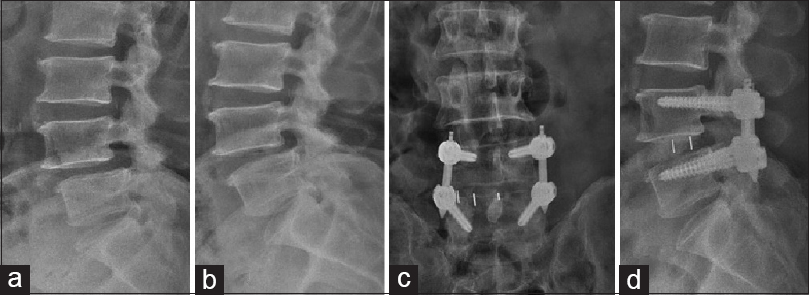
Standing lateral dynamic X-rays showed a grade 1 listhesis at the L4–L5 level [Figure
Surgery
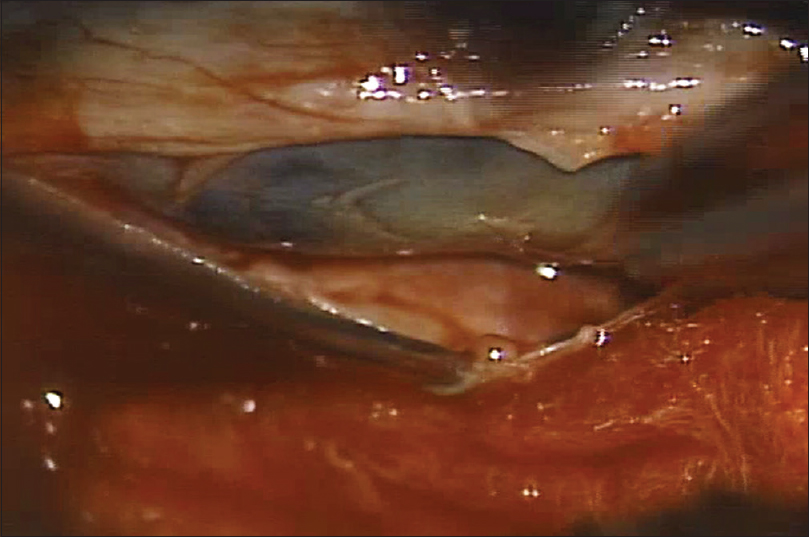
The patient underwent a right L5 microscope-assisted hemilaminectomy. When the dura was opened longitudinally, it revealed a dark blood clot within a semi-transparent neomembrane [
Histopathology
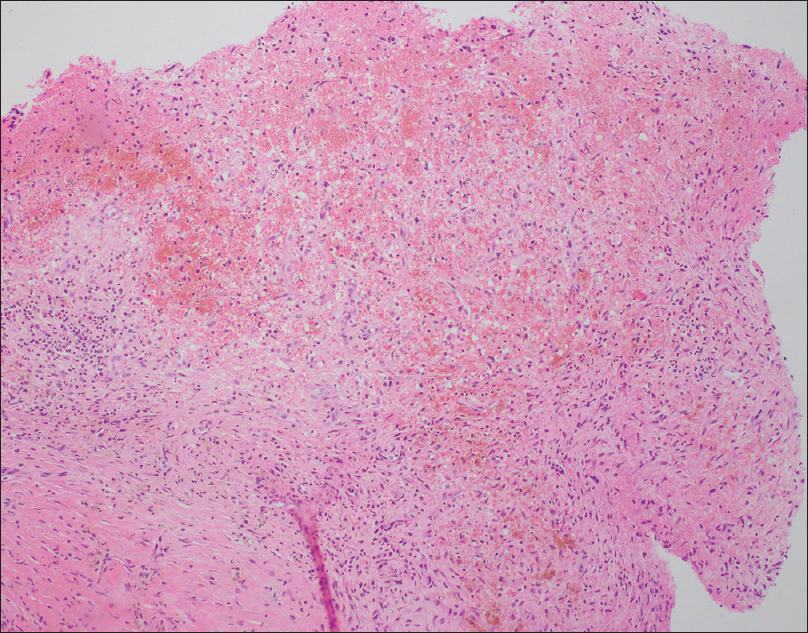
Histopathology showed membranes with loose connective tissue containing scattered lymphocytes, siderophages, many eosinophils within areas of hemorrhage, and spindly, fibroblasts. These findings confirmed the diagnosis of a chronic SDH [
DISCUSSION
Spontaneous spinal SDHs without coagulopathy are rare conditions. There are two major theories regarding the etiology of these lesions. First, they may be attributed to cranial subarachnoid hemorrhages (SAH) that have extended into the spinal subarachnoid space and spinal subdural space by exceeding or lacerating the arachnoid membrane. Second, minor trauma increases both the intrathoracic pressure and intraluminal pressure of the vessels in the subarachnoid space. When cerebrospinal fluid pressure momentarily lags behind the intravascular pressure, vessels may ruptures resulting in SAH.[
MRI is the best imaging modality for diagnosing spinal SDH. The radiological differential diagnoses include schwannoma, meningioma, intradural lipoma, and spinal SDH. There are no definite guidelines for the management of these lesions. Those without neurological deficits may be treated with nonoperative management and serial MRI monitoring.
The operative treatment for spinal SDH includes wide laminectomy for evacuation of the hematoma.[
CONCLUSION
The differentiate diagnosis for spinal intradural/extramedullary lesions should include chronic spinal SDH even without the history of trauma or coagulopathies. The early diagnosis and treatment of these lesions optimizes outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abuzayed B, Oğuzoğlu SA, Dashti R, Ozyurt E. Spinal chronic subdural hematoma mimicking intradural tumor in a patient with history of Hemophilia A: Case report. Turk Neurosurg. 2009. 19: 189-91
2. Jung H-S, Jeon I, Kim SW. Spontaneous Spinal Subdural Hematoma with Simultaneous Cranial Subarachnoid Hemorrhage. J Korean Neurosurg Soc. 2015. 57: 371-5
3. Kang HS, Chung CK, Kim HJ. Spontaneous spinal subdural hematoma with spontaneous resolution. Spinal Cord. 2000. 38: 192-6
4. Khosla VK, Kak VK, Mathuriya SN. Chronic spinal subdural hematomas. Report of two cases. J Neurosurg. 1985. 63: 636-9
5. Kim HY, Ju CI, Kim SW. Acute cervical spinal subdural hematoma not related to head injury. J Korean Neurosurg Soc. 2010. 47: 467-9