- Department of Neurosurgery, PGIMER, Chandigarh, India
- Department of Ophthalmology, PGIMER, Chandigarh, India
Correspondence Address:
Pravin Salunke
Department of Ophthalmology, PGIMER, Chandigarh, India
DOI:10.4103/2152-7806.157622
Copyright: © 2015 Sodhi SBH This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Singh Sodhi HB, Salunke P, Kaur S, Singh R. Missing the ‘window’ might shut the light forever: Central retinal artery occlusion following spine surgery. Surg Neurol Int 25-May-2015;6:86
How to cite this URL: Singh Sodhi HB, Salunke P, Kaur S, Singh R. Missing the ‘window’ might shut the light forever: Central retinal artery occlusion following spine surgery. Surg Neurol Int 25-May-2015;6:86. Available from: http://surgicalneurologyint.com/surgicalint_articles/missing-window-might-shut-light-forever-central-retinal/
Dear Editor,
The occurrence of postoperative visual loss (POVL) after spine surgery in prone position, although rare, has been described.[
We present a case with unilateral visual loss due to central retinal artery occlusion (CRAO) after surgery in prone position that was detected a few hours after surgery and improved only partially. Apart from various causes and preventive measures, this manuscript highlights the factors that may delay the detection of POVL following spinal surgery, making the treatment less effective.
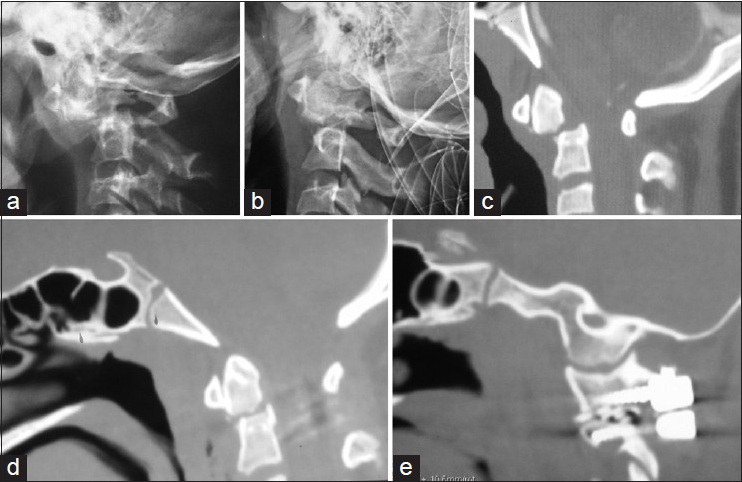
A 13-year-old child presented 4 weeks posttrauma with complaints of gradually progressive spastic quadriparesis and neck pain. On neurological examination, patient had spastic quadriparesis with grade 3/5 power in all four limbs. Radiological examination revealed nonunited C2-dens fracture with cord compression, which could not be reduced on traction [Figure
Figure 1
(a) X-ray Cranio-vertebral junction lateral view showing type II odonotid fracture with atlantoaxial dislocation. (b) Incomplete reduction of dislocation despite traction. (c) Midsagittal CT image showing fracture and dislocation. (d and e) Postoperative midsagittal and parasagittal images showing complete reduction and the strong construct
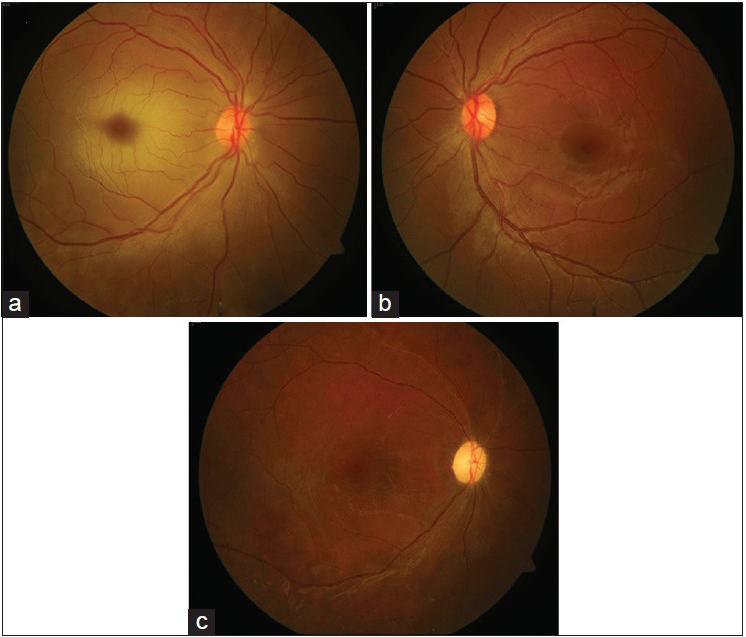
Three hours later when patient recovered from sedative effect, he complained of complete vision loss in the right eye. There was no peri-orbital swelling, edema, ecchymosis, proptosis, or any other sign of venous fullness. Ocular examination revealed no perception of light in the right eye and 20/20 in the left eye. Lids and adnexa were normal, with intraocular pressure of 12 and 14 mmHg in right and left eye, respectively, by Perkins applanation tonometer. There was presence of relative afferent pupillary defect (RAPD) in the right eye, with normal direct and weak consensual reflex in the left eye. Posterior segment examination in the right eye revealed the presence of cherry red spot with pale retina and gross retinal vascular attenuation [
Figure 2
(a) Fundus picture of the right eye on presentation showed the presence of normal disc and vasculature but pale retina with cherry red spot on the macula. (b) Left eye examination was normal. (c) Fundus picture of the right eye 6 weeks later with pale disc and sclerosed attenuated retinal vessels. The retina had regained its normal color but the foveal reflex was dull
Patient was immediately given a digital massage and inhalation in a plastic bag. Anterior chamber paracentesis was done bedside to restore blood flow to the retina and patient was given oral acetazolamide 500 mg stat.
After the emergency measures, there was no change in the symptoms of the patient. Patient was kept under follow up on serial fundus imaging. The systemic work up of the patient was normal and there was no evidence of any hypercoagulopathy (blood profile, coagulogram and serum homocysteine levels were normal). Patient could count fingers close to the face at follow-up examination at 3 weeks. There was presence of RAPD, with disc pallor and severe arterial attenuation, and resolution of cherry red spot. At the last follow-up examination at 6 weeks, patient is reading 20/120 in the right eye [
The incidence of POVL after surgery in prone position ranges from 0.028% to 0.2%, and is a devastating complication with debilitating consequences for the patient. [
The present case had CRAO with partial improvement in vision over 6 weeks, starting from 48 h postsurgery. The cause of CRAO in this patient remains elusive as none of the risk factors described in literature were evident in our case. The surgical time and intraoperative blood loss in the present case were significantly low, along with no signs suggestive of direct pressure over the globe. There were no intraoperative events leading on to systemic hypotension and patient had no previous cardiac history as well.
A remote possibility is of a thrombus in vertebral artery (VA), due to trauma that can throw emboli during manipulation of facets. A normal VA on preoperative CT angiogram almost rules out this possibility. There is a possibility of fat embolism that might have occurred during the intrafracture distraction. Fat embolism has been described as a cause of CRAO. [
The treatment of CRAO is digital massage, carbonic anhydrase inhibitors, and anterior chamber paracentesis. These measures are known to alter the natural course of CRAO but only if implemented within the correct time window of 2–4 h. Irreversible retinal damage occurs after the retina is ischemic for 90–100 min. [
POVL remains an unfortunate and infrequent morbid event occurring in patients undergoing spine surgery. Despite taking all precautions like proper positioning and avoiding blood loss, the surgeon may encounter such a dreaded complication in few cases. In certain instances the visual loss may be reversible, provided it is detected early. Caution needs to be practiced before instituting opiate analgesia especially in spinal surgeries in prone position, lest such complications be missed. Treatment after the window period has elapsed may not bear desirable results.
References
1. Baig MN, Lubow M, Immesoete P, Bergese SD, Hamdy EA, Mendel E. Vision loss after spine surgery: Review of the literature and recommendations. Neurosurg Focus. 2007. 23: E15-
2. Hayreh SS, Kolder HE, Weingeist TA. Central retinal artery occlusion and retinal tolerance time. Ophthalmology. 1980. 87: 75-8
3. Kim KE, Ahn SJ, Woo SJ, Kim N, Hwang JM. Central retinal artery occlusion caused by fat embolism following endoscopic sinus surgery. J Neuroophthalmol. 2013. 33: 149-50
4. Salunke P, Futane S, Sahoo SK, Ghuman MS, Khandelwal N. Operative nuances tosafeguard anomalous vertebral artery without compromising the surgery for congenital atlantoaxial dislocation: Untying a tough knot between vessel and bone. J Neurosurg Spine. 2014. 20: 5-10
5. Salunke P, Sahoo S, Khandelwal NK, Ghuman MS. Technique for direct posterior reduction in irreducible atlantoaxial dislocation: Multi-planar realignment of C1-2. Clin Neurol Neurosurg. 2015. 131C: 47-53
6. Quraishi NA, Wolinsky JP, Gokaslan ZL. Transient bilateral post-operative visual loss in spinal surgery. Eur Spine J. 2012. 21: S495-8
7. Zimmerer S, Koehler M, Turtschi S, Palmowski-Wolfe A, Girard T. Amaurosis after spine surgery: Survey of the literature and discussion of one case. Eur Spine J. 2011. 20: 171-6