- Department of Neurosurgery, University of California-Los Angeles, Seattle
- Department of Neurosurgery, University of Washington, Seattle
- Department of Neurosurgery, Division of Neurosurgery, Seattle Children’s Hospital, Seattle, Washington
- Department of Neurosurgery, University of Miami, Miller School of Medicine, Miami, Florida, USA
- Department of Neurosurgery, Division of Pediatric Surgery, Kaiser Permanente Los Angeles Medical Center, Los Angeles
- Department of Neurosurgery, Division of Pediatric Neurosurgery, Kaiser Permanente – Oakland Medical Center, Oakland, California
Correspondence Address:
Jason Hauptman
Department of Neurosurgery, University of Washington, Seattle
Department of Neurosurgery, Division of Neurosurgery, Seattle Children’s Hospital, Seattle, Washington
DOI:10.25259/SNI-26-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alexander M. Tucker, Peter Morgenstern, Daniel Diaz, Shaina Sedighim, Donald Shaul, Roman Sydorak, Mark Fedor, Amy Lee, Jason Hauptman. Neurosurgical management of Currarino syndrome: A case series and review of literature. 24-Apr-2019;10:70
How to cite this URL: Alexander M. Tucker, Peter Morgenstern, Daniel Diaz, Shaina Sedighim, Donald Shaul, Roman Sydorak, Mark Fedor, Amy Lee, Jason Hauptman. Neurosurgical management of Currarino syndrome: A case series and review of literature. 24-Apr-2019;10:70. Available from: http://surgicalneurologyint.com/surgicalint-articles/9283/
Abstract
Background:The Currarino syndrome (CS), defined by the triad of anorectal malformations, sacral bone deformities, and presacral masses, is rare. There are few surgical series that discuss conservative management versus the surgical approaches to these lesions. Here, we describe utilizing a combined anterior and posterior approach for resecting these lesions in four patients.
Methods:Four patients with CS were treated with two-stage approaches performed by a multidisciplinary team, including pediatric neurosurgery and general surgery. The first anterior laparoscopic approach mobilized the presacral mass from its ventral attachments. The second posterior procedure detethered the spinal cord, repaired the dural defect, and facilitated removal of the presacral mass.
Results:Gross total resection of all four presacral masses was accomplished without intraoperative complication; all patients clinically improved.
Conclusion:The CS is characterized by a large presacral mass. Here, one must rule out malignancy and also consider diagnosis/resection due to the risks for malignant transformation. The operative approach we described in four patients utilized standard anterior mobilization of the mass, followed by posterior detethering, dural repair, and ultimate resection.
Keywords: Currarino syndrome, presacral mass, tethered cord, ventral meningocele
INTRODUCTION
Currarino syndrome (CS) is a rare condition defined by a triad consisting of anorectal malformations, sacral bone deformities, and presacral masses.[
Although over 300 patients with Currarino’s triad have been reported/treated, there is no consensus regarding their optimal conservative versus surgical management.[
Different surgical approaches have been utilized.[
CASE SUMMARIES
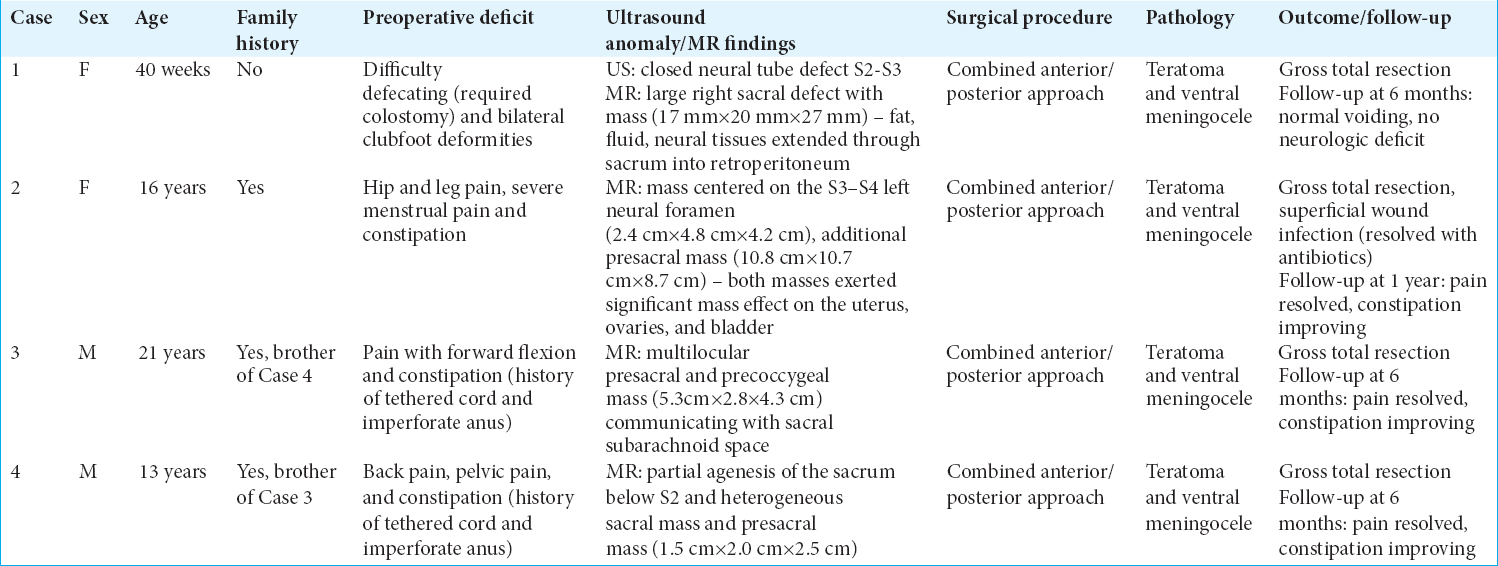
Four patients were included in this study [
Magnetic resonance studies and surgery
An magnetic resonance (MR) imaging scan was obtained on all patients and revealed presacral masses with sacral defects. All underwent a combined anterior/posterior approach performed by a multidisciplinary team including pediatric neurosurgery and general surgery. The pathology revealed each patient had both a sacral meningocele and teratoma. Only one patient had a perioperative complication consisting of a superficial wound infection treated successfully with antibiotics. Patients were followed an average of 8 postoperative months, by which time all exhibited improvement in their symptoms including the resolution of pelvic pain. Further, constipation resolved completely in one patient and improved but persisted in the other three. None demonstrated delayed neurological deterioration.
SUMMARY OF OPERATIVE TECHNIQUE
Anterior approach
Each patient was initially positioned supine, and laparoscopic access was obtained to the presacral mass. It was carefully dissected away from surrounding structures, with care taken to identify and preserve both ureters. The dissection was taken down to the anal canal and the levators. Following sufficient mobilization of the meningocele, the abdominal wounds were closed, and the patient was turned prone.
Posterior approach
Midline dissection was carried down to the sacrum where multiple sacral laminectomies were performed. A midline durotomy was created inferior to the level of the most caudal exiting nerve root. Detethering was achieved by sectioning the filum terminale. Next, the thecal sac was circumferentially dissected, allowing for identification of the fistula, leading to the anterior sacral meningocele. The dissection was then extended below the coccyx into the presacral space, where it was ventrally mobilized from the posterior sacrospinous ligaments and ultimately fully resected.
DISCUSSION
Patients with CS most commonly present with severe constipation after birth.[
The female-to-male ratio of CS is 2:1 in children and 6:1 in adults. The increased female predominance in adults may be partially due to the frequency of CS diagnosed for patients presenting with dysmenorrhea (e.g., patient 2). About >50% of patients with CS have a mutation of HLXB9 located at 7q36; such mutations have been observed in up to 90% of familial-associated CS.[
Utilizing a comprehensive, multidisciplinary team (oncology, pediatric surgery, and pediatric neurosurgery) and two-staged anterior/posterior surgical approaches, four patients with CS successfully underwent total resection of these lesions without any adverse events. We advocate early operative intervention for multiple reasons. First, symptoms can be improved with surgery. Second, early surgical intervention limits the risk of future, spontaneous rupture of the teratoma, resulting in meningitis, spinal abscesses, and/or malignant transformation. Third, surgical resection provides an accurate, confirmatory pathologic diagnosis.[
CONCLUSION
CS is a rare condition associated with a triad of findings. Symptomatic sacral masses should be promptly treated with anterior followed by posterior surgical resection. This provides an immediate pathologic diagnosis, while gross total resection can be safely accomplished without significant neurological injury. Alternatively, waiting and watching may result in not only a delay in diagnosis and the risk of malignant transformation but also increases the risk of permanent neurological injury.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barwick K. Anorectal presacral and sacral tumors. Gastroenterology. 1987. 92: 2046-7
2. Chakhalian D, Gunasekaran A, Gandhi G, Bradley L, Mizell J, Kazemi N. Multidisciplinary surgical treatment of presacral meningocele and teratoma in an adult with currarino triad. Surg Neurol Int. 2017. 8: 77-
3. Colombo F, Janous P, Buxton N. Carcinoid transformation of presacral dermoid cyst in patient with currarino syndrome:A case report. Br J Neurosurg. 2017. 14: 1-2
4. Crétolle C, Pelet A, Sanlaville D, Zérah M, Amiel J, Jaubert F. Spectrum of HLXB9 gene mutations in currarino syndrome and genotype-phenotype correlation. Hum Mutat. 2008. 29: 903-10
5. Emans PJ, Kootstra G, Marcelis CL, Beuls EA, van Heurn LW. The currarino triad:The variable expression. J Pediatr Surg. 2005. 40: 1238-42
6. Isik N, Elmaci I, Gokben B, Balak N, Tosyali N. Currarino triad:Surgical management and follow-up results of four correction of three cases. Pediatr Neurosurg. 2010. 46: 110-9
7. Kirks DR, Merten DF, Filston HC, Oakes WJ. The currarino triad:Complex of anorectal malformation, sacral bony abnormality, and presacral mass. Pediatr Radiol. 1984. 14: 220-5
8. Köchling J, Pistor G, Brands SM, Nasir R, Lanksch WR. The currarino syndrome hereditary transmitted syndrome of anorectal, sacral and presacral anomalies. Case report and review of the literature. Eur J Pediatr Surg. 1996. 6: 114-9