- Department of Neurosurgery, Hamad General Hospital, Doha, Qatar
- Department of Radiology, Hamad General Hospital, Doha, Qatar
Correspondence Address:
Kazim Mohammed
Department of Neurosurgery, Hamad General Hospital, Doha, Qatar
DOI:10.4103/sni.sni_37_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kazim Mohammed, Javeed Iqbal, Hussein Kamel, John Mathew, Ghanem Al-Sulaiti. Obstructive hydrocephalus and facial nerve palsy secondary to vertebrobasilar dolichoectasia: Case Report. 07-Mar-2018;9:60
How to cite this URL: Kazim Mohammed, Javeed Iqbal, Hussein Kamel, John Mathew, Ghanem Al-Sulaiti. Obstructive hydrocephalus and facial nerve palsy secondary to vertebrobasilar dolichoectasia: Case Report. 07-Mar-2018;9:60. Available from: http://surgicalneurologyint.com/surgicalint-articles/obstructive-hydrocephalus-and-facial-nerve-palsy-secondary-to-vertebrobasilar-dolichoectasia-case-report/
Abstract
Background:Symptomatic hydrocephalus due to vertebrobasilar dolichoectasia is a rare occurrence.
Case Description:We report a patient who presented with acute confusion and vomiting. Neuroimaging revealed elongated and tortuous basilar artery indenting and elevating the floor of third ventricle causing obstructive hydrocephalus. Initially, the patient was treated with external ventricular drain and then with ventriculo-peritoneal shunt.
Conclusion:We suggest prompt surgical intervention upon diagnosis as a first choice of treatment in order to avoid further complications.
Keywords: Facial nerve palsy, hydrocephalus, vertebro-basilar dolichoectasia, vp shunt
INTRODUCTION
Vertebrobasilar dolichoectasia (VBD), also known as dilative arteriopathy, is tortuosity, elongation, and dilatation of the vertebral/basilar arteries or their junction. VBD is a known clinical entity with a patient presentation ranging from severe symptoms such as ischemic/hemorrhagic stroke, thromboembolic lesions, or with cranial nerve compression. They may also have varied clinical presentations, which includes tic douloureux, neuralgia, tinnitus, vertigo, motor or sensory deficits, ataxia, dementia, headache, migraine, leukoencephalopathy, central sleep apnea, and cerebellar dysfunctions; patients may also be asymptomatic[
CASE REPORT
Our patient is a 51-year-old Filipino female who had been recently diagnosed with hypertension, non-compliant with medication, presented to the emergency department with acute confusion for 1 day and repeated vomiting. There was no history of loss of consciousness or seizures. On admission, her blood pressure was 198/120 mm Hg, pulse was 92/min, and respiratory rate was 20/min. On examination, her glasgow coma scale (GCS) was 14/15, pupils were 3 mm, equal and reactive bilaterally. No evident cranial nerve palsy was observed. There was no papilledema.
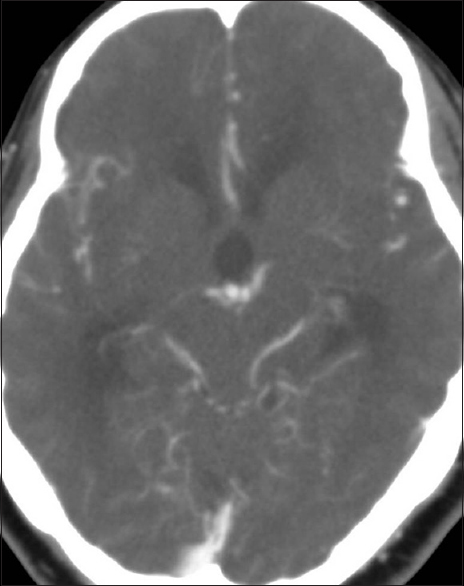
Patient underwent CT scan brain and CT angiogram (CTA), which showed dilatation of both lateral and the third ventricles with periventricular hypo densities suggestive of transependymal cerebrospinal fluid (CSF) permeation. No intracranial hemorrhage was seen [
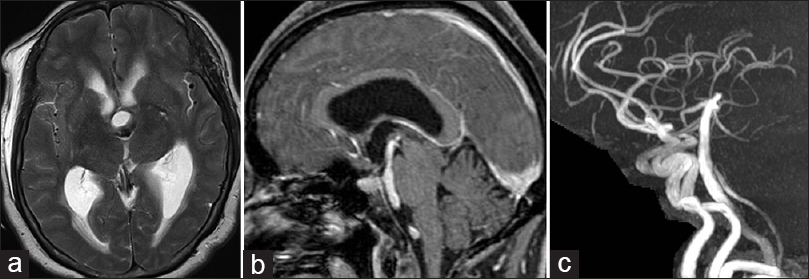
The following day, we performed MRI with MR angiogram (MRA) and CSF flow studies. This revealed residual dilatation of both lateral and the anterior part of the third ventricle [
Figure 2
(a) Axial T2W, MRI image at almost a similar level showing, residual ventricular dilation and mild periventricular edema after insertion of the ventricular drain (small associated right frontal sub-galial collection). Note the basilar artery bifurcation (black arrow) indenting the posterior end of the dilated third ventricle. (b) Sagittal contrast-enhanced T1W image showing the elongated basilar artery (black arrow) elevating and causing compression and collapse of the posterior third ventricle. Contrast this with the dilated anterior third ventricle (white arrow). (c) Lateral MIP of a Time of Flight (TOF) MRA confirming the elevation of the basilar bifurcation (black arrow) above the carotid syphon (white arrow) normally situated lateral to the sella turcica
On retrospect, the third ventricular compression and the elevation of the basilar bifurcation was overlooked on the initial CTA. MRI and MRA were useful in settling the diagnosis.
Finally, the external ventricular drain was converted to ventriculo-peritoneal shunt and was subsequently discharged.
DISCUSSION
The incidence of intracranial dolichoectasia varies between 0.06–5.8%. Dolichoectasia is most common in the vertebral and basilar arteries.[
Normally, the bifurcation of the basilar artery is located in the interpeduncular cistern adjacent to the dorsum sellae or in the suprasellar cistern below the level of the floor of third ventricle.
The diagnostic criteria for VBD is a basilar artery >4.5 mm in diameter, deviation of any portion of both arteries more than 10 mm from its shortest expected course, a basilar artery length >29.5 mm or intracranial vertebral length >23.5 mm.[
Vertical elongation of the vertebrobasilar arteries can be graded, according to Smoker et al.,[
0: at or below dorsum sellae
1: Within suprasellar cistern
2: at the level of third ventricle floor
3: indenting and elevating floor of the third ventricle.
Passero et al.[
Symptomatic patients with normal caliber but tortuous basilar artery are more likely to have isolated cranial nerve involvement, where as the patient with marked basilar artery dilation were far more likely to present with compressive or ischemic neurological deficits.[
VBD is an ischemic stroke risk factor. Intracranial VBD shows much more frequent occurrence of small vessel disease in stroke patients. The small blood vessel disease damage is dominated by multi-lacunar infarction, leukoriasis, and etat crible’. Intracranial bleeding in patients with VBD is not uncommon as previously believed.[
Hydrocephalus in VBD can be due to compression of the third ventricle due to ecstatic elongated basilar artery. Only few cases of hydrocephalus due to direct compression of the aqueduct, foramen of Monro, or the third ventricle have been reported in the literature. Another peculiar mechanism of hydrocephalus by “Water Hammering” effect due to the pulsatile blood in the ecstatic vessels which creates CSF flow impairment through the third ventricle has been described.[
Zisimopoulou et al. in their study suggested that the underlying mechanism for obstructive hydrocephalus due to vertebrobasilar dolichoectasia are both a water-hammer effect and a direct compression of adjacent structures.[
In our patient, there was a very high vertebral fusion to form the basilar artery. The basilar artery ran 18.4 above the dorsum sellae. Its maximum diameter reached 4.1mm. Since the obstruction was at the level of third ventricle, the patient benefitted from uni-ventricular shunt. Only few reported cases with obstruction at the level of foramen of Monroe required biventricular shunt.
Although the diagnosis was evident on the MR and MRA, it could not be seen on the initial CTA. Thin layer scans of high-resolution CT can to some extent avoid misdiagnosis caused by petrous bone artifacts - as suggested by Yong-Jie Yuan et al. in their study.[
For an unclear reason, most of the cases of hydrocephalus complicating VBD have been reported from India. It is not clear whether VBD or its complications are more common in the Indian subcontinent or if this was simply a reporting bias.
Also, it is not clear why the VIIth nerve palsy was noted only following the ventricular shunt insertion. We believe that since it was subtle it might be there since start but was noticed only when the patient was evaluated thoroughly the following morning after the emergency shunt insertion. This is supported by the fact that the facial nerve palsy was on the right – the same to which the basilar artery is deviated.
CONCLUSION
Hydrocephalus is a rare but important presentation of VBD. This condition must be suspected whenever supra-tentorial hydrocephalus is evident in the presence of VBD. Review of the literature shows that VBD can have significant consequences and highlights the importance of identifying this finding, if present, whenever reporting on brain imaging studies. MRI or MRA are useful in confirming the diagnosis, if not digital subtraction angiography. Prompt surgical intervention upon diagnosis should be considered as a first choice of treatment in order to avoid further complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Hassoun HK, Aubaid HN, Zwain AM. Vertebrobasilar Dolichoectasia: Clinical Neuroimaging Correlation. The Iraqi Postgraduate Medical Journal. 2015. 14:
2. Kansal R1, Mahore A, Dange N, Kukreja S. Dolichoectasia of vertebrobasilar arteries as a cause of hydrocephalus. J Neurosci Rural Pract. 2011. 2: 62-4
3. Resta M, Gentile A, Cuonzo FD, Vinjau E, Brindicci D, Carella A. Clinical- angiographic correlations in 132 patients with megadolichovertebrobasilar anomaly. Neuroradiology. 1984. 26: 213-
4. Siddiqi A, Chew NS, Miszkiel K. Vertebrobasilar dolichoectasia: A rare cause of obstructive hydrocephalus. B J Radiol. 2008. 81: e123-6
5. Smoker WR, Price MJ, Keyes WD, Corbett JJ, Gentry LR. High-resolution computed tomography of the basilar artery 1. Normal size and position. AJNR Am J Neuroradiol. 1986. 7: 55-60
6. Passero SG. Natural history of vertebrobasilar dolichoectasia. J Neurology. 2008. 70: 66-72
7. Titlic M, Tonkic A, Jukic I, Kolic K, Dolic K. Clinical manifestations of vertebrobasilar dolichoectasia. Bratisl Lek Listy. 2008. 109: 528-30
8. Ubogu EE, Zaidat OO. Vertebrobasilar dolichoectasia diagnosed by magnetic resonance angiography and risk of stroke and death: A cohort study. J Neurology Neurosurg Psychiatry. 2004. 75: 22-6
9. Zisimopoulou V, Ntouniadaki A, Aggelidakis P, Siatouni A, Gatzonis S, Tavernarakis A. Vertebrobasilar Dolichoectasia Induced Hydrocephalus: the Water-Hammer Effect. Clin Pract. 2015. 24;5: 749-
10. Yuan YJ, Xu K, Luo Q, Yu JL. Research Progress on Vertebrobasilar Dolichoectasia. Int J Int J Med Sci. 2014. 11: 1039-48
11. Yu Y, Mosely IF, Pullicino P, McDonald WI. The clinical picture of ectasia of the intracerebral arteries. J Neurology, Neurosurg Psychiatry. 1982. 45: 29-36