- Department of Neurosurgery, Kobari General Hospital, Yokouchi, Noda, Chiba, Japan
- Department of Neurosurgery, University of Tsukuba, Tsukuba, Ibaraki, Japan
Correspondence Address:
Hideaki Matsumura
Department of Neurosurgery, University of Tsukuba, Tsukuba, Ibaraki, Japan
DOI:10.4103/2152-7806.193726
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Matsumura H, Fujimori H, Sato N, Matsumura A. Paraplegia caused by cerebral contusions in the bilateral precentral gyri. Surg Neurol Int 09-Nov-2016;7:
How to cite this URL: Matsumura H, Fujimori H, Sato N, Matsumura A. Paraplegia caused by cerebral contusions in the bilateral precentral gyri. Surg Neurol Int 09-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/paraplegia-caused-cerebral-contusions-bilateral-precentral-gyri/
Abstract
Background:Paraplegia is mainly caused by spinal cord disease and rarely occurs due to head trauma. In this report, we describe a case of paraplegia caused by cerebral contusions in the bilateral precentral gyri.
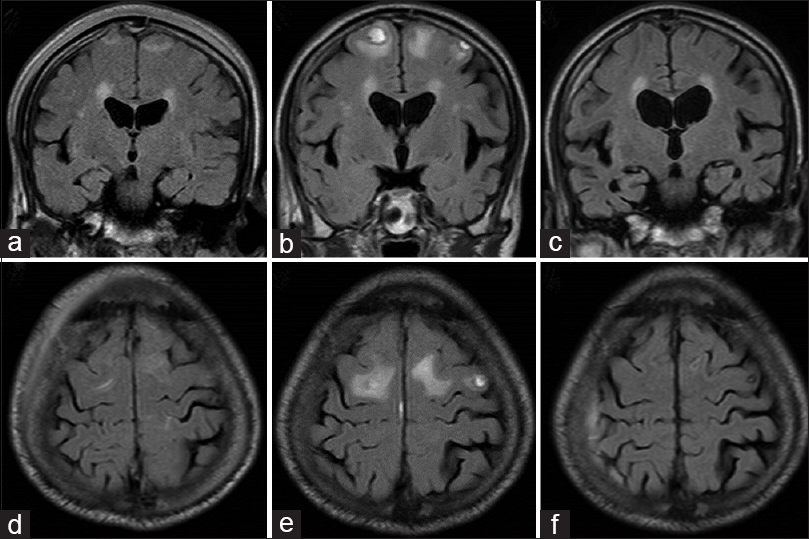
Case Description:A 72-year-old man was admitted to our hospital with mildly impaired consciousness and severe pure motor paralysis in both legs. He was healthy until the morning of the day, but his wife found him injured in front of his house upon returning home. He had a subcutaneous hematoma in his occipital region, and seemed to have slipped by accident. Computed tomography of the brain and magnetic resonance imaging (MRI) of his spinal cord revealed no apparent cause of the paraplegia, although an MRI of his brain clearly revealed cerebral contusions in the bilateral precentral gyri. The cerebral contusion was diagnosed as the cause of pure motor paralysis of lower extremities. He received rehabilitation, and manual muscle testing of his legs revealed improvements. In the subacute phase, the precentral gyrus lesion disappeared on MRI.
Conclusion:We must emphasize that cerebral contusion can be a differential diagnosis for paraplegia. In the acute phase, fluid-attenuated inversion recovery (FLAIR) MRI coronal and sagittal images are useful for identifying precentral gyri contusions. Paraplegia caused by a cerebral contusion may be misdiagnosed as a spinal concussion due to the disappearance of the precentral gyrus lesion on FLAIR MRI in the subacute phase.
Keywords: Bilateral precentral gyri contusions, head injury, paraplegia, pure motor paralysis, spinal concussion
INTRODUCTION
Paraplegia is most commonly caused by spinal cord conditions including traumatic injuries, degenerative diseases, tumors, and infections.[
CASE PRESENTATION
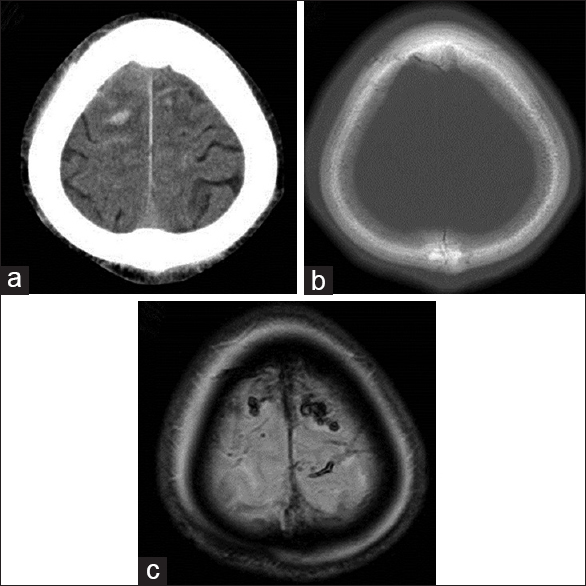
A 72-year-old Japanese male was transferred to our hospital with mildly impaired consciousness and gait disturbance. He was healthy until the morning of that day, but his wife found him injured in front of his house upon returning home. He had a subcutaneous hematoma in his occipital region, and seemed to have slipped by accident. In our initial evaluation, his Glasgow Coma Scale score was 13 (E3V4M6). He was unable to raise his legs or stand. A neurological examination revealed pure motor paralysis of the legs. There were no sensory disturbances. Manual muscle testing revealed scores of 5/5 for the upper limbs. However, these scores were 0/5 for the bilateral iliopsoas, tibialis anterior and tibialis posterior, 3/5 for both adductors and hamstrings, and 1/5 for both quadriceps femoris. Deep tendon jerks in both the lower and upper limbs were slightly diminished and without laterality. No significantly abnormal laboratory findings, including hypokalemia or an inflammation response, were noted in a general blood exam. Computed tomography (CT) of the brain revealed a subarachnoid hemorrhage, subdural hematoma, and contusions in his basal frontal lobes and superior frontoparietal lobes [Figure
Figure 1
Axial computed tomography image near the vertex on admission showing a hemorrhage and a peripheral low-density area (a). Axial bone window computed tomography image near the vertex revealing no fracture (b). Axial T2*-weighted magnetic resonance image clearly revealing cerebral contusions in the bilateral parasagittal region near the vertex (c)
DISCUSSION
We reported a case of paraplegia caused by cerebral contusions. Low-density areas were observed around the hemorrhage near the vertex in the initial CT that indicated a cerebral contusion. When a high-density lesion is located around the vertex, it may be difficult to distinguish between traumatic subarachnoid hemorrhage, subdural hematoma, and cerebral contusion on the first examination of the CT images [
In this patient, the lesion on FLAIR MRI first became exacerbated and then disappeared by 7 weeks [
We know of only one previous case report describing paraplegia[
The reasons that most patients recover from paralysis caused by cerebral contusions is not fully understood. There are several international studies regarding the prediction of the outcomes of patients with traumatic brain injuries.[
Paraplegia caused by a cerebral contusion may be misdiagnosed as a spinal concussion because lesions of the precentral gyrus on FLAIR MRI disappear in the subacute phase.
CONCLUSION
We conclude that bilateral cerebral contusions of the precentral gyri can cause paraplegia. Coronal MRI in the acute phase is useful in the diagnosis and the prediction of the functional prognosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ando K, Maruya J, Kanemaru Y, Nishimaki K, Minakawa T. [Pure motor monoparesis of a lower limb due to head injury: A case report]. Brain Nerve. 2012. 64: 1427-30
2. Besenski N. Traumatic injuries: Imaging of head injuries. Eur Radiol. 2002. 12: 1237-52
3. Besenski N, Broz R, Jadro-Santel D, Pavic D, Mikulic D. The course of the traumatising force in acceleration head injury: CT evidence. Neuroradiol. 1996. 38: S36-41
4. Gauge N, Sergides I, Wainwright K, Zebian B, Bhangoo R. Head injury: A rare cause of paraplegia. Injury Extra. 2010. 41: 112-3
5. Gentry LR, Godersky JC, Thompson B. MR imaging of head trauma: Review of the distribution and radiopathologic features of traumatic lesions. AJR Am J Roentgenol. 1988. 150: 663-72
6. Liliang PC, Liang CL, Chen HJ, Cheng CH. Vertex epidural haematoma presented with paraplegia. Injury. 2001. 32: 252-3
7. Majdan M, Lingsma HF, Nieboer D, Mauritz W, Rusnak M, Steyerberg EW. Performance of IMPACT, CRASH and Nijmegen models in predicting six month outcome of patients with severe or moderate TBI: An external validation study. Scand J Trauma Resusc Emerg Med. 2014. 22: 68-
8. Messori A, Pauri F, Rychlicki F, Veronesi V, Salvolini U. Acute posttraumatic paraplegia caused by epidural hematoma at the vertex. AJNR Am J Neuroradiol. 2001. 22: 1748-9
9. Moen KG, Skandsen T, Folvik M, Brezova V, Kvistad KA, Rydland J. A longitudinal MRI study of traumatic axonal injury in patients with moderate and severe traumatic brain injury. J Neurol Neurosurg Psychiatry. 2012. 83: 1193-200
10. New PW, Reeves RK, Smith E, Townson A, Eriks-Hoogland I, Gupta A. International retrospective comparison of inpatient rehabilitation for patients with spinal cord dysfunction epidemiology and clinical outcomes. Arch Phys Med Rehabil. 2015. 96: 1080-7
11. Parizel PM, Van Goethem JW, Ozsarlak O, Maes M, Phillips CD. New developments in the neuroradiological diagnosis of craniocerebral trauma. Eur Radiol. 2005. 15: 569-81
12. Ringelstein EB, Krieger D, Hunermann B. Evaluation by MRI of paraparesis and tetraparesis of undiagnosed aetiology. J Neurol. 1987. 234: 401-7
13. Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: What learns a worldwide literature survey?. Spinal Cord. 2006. 44: 523-9