- Winthrop University Hospital, Mineola, New York, USA
- Colgate University, Hamilton, NY, USA
Correspondence Address:
M. M. Stecker
Colgate University, Hamilton, NY, USA
DOI:10.4103/2152-7806.199558
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: M. M. Stecker, M. Stecker, J. Falotico. Predictive model of length of stay and discharge destination in neuroscience admissions. 06-Feb-2017;8:17
How to cite this URL: M. M. Stecker, M. Stecker, J. Falotico. Predictive model of length of stay and discharge destination in neuroscience admissions. 06-Feb-2017;8:17. Available from: http://surgicalneurologyint.com/surgicalint-articles/predictive-model-of-length-of-stay-and-discharge-destination-in-neuroscience-admissions/
Abstract
Background:The purpose of this study was to try and determine the best predictors of hospital length of stay and discharge destination in patients admitted to a neuroscience service.
Methods:Valid data was collected for 170 patients. Variables included age, gender, location prior to admission, principle diagnosis, various physiological measurements upon admission, comorbidity, independence in various activities of daily living prior to admission, length of stay, and disposition upon discharge. Study design was a correlational descriptive study performed through the analysis of data and the development and validation of statistically significant factors in determining the length of stay.
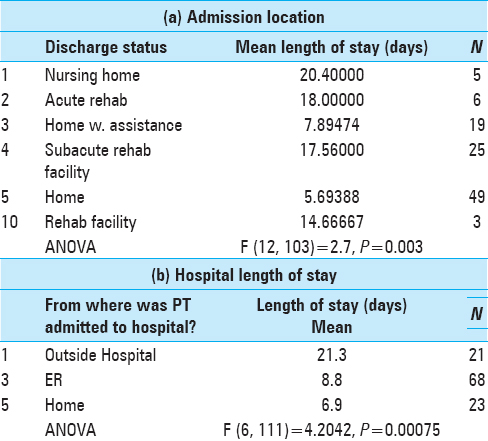
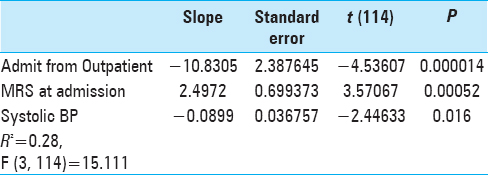
Results:All factors with a strong (P
Conclusions:Functional status at admission, specifically, a higher modified Rankin score and a lower systolic blood pressure along with the acquisition of deep vein thrombosis, catheter associated urinary tract infections, intubation, and admission to an intensive care unit all have a statistically significant effect on the hospital length of stay.
Keywords: Comorbidity, functional status, length of stay
INTRODUCTION
A valid estimation of hospital length of stay (LOS) and accurately predicted discharge destinations can help significantly improve hospital discharge planning and resource efficiency. This information can also be useful for caregivers in their preparation of post-discharge care. The development of a predictive model that is efficient and easy to use may lead to improving patient care within a neuroscience service line. Various studies have linked a wide range of sociodemographic and clinical factors to both LOS and discharge destination.[
A Swedish population-based cohort study examined the factors that influenced acute and total LOS for 298 first-ever stroke patients.[
A retrospective cohort study in an acute hospital rehabilitation center in Singapore determined the predictors of LOS in 491 stroke patients.[
Simonet[
The cited studies clearly support the predictive nature of certain sociodemographic and clinical factors with regards to LOS and discharge destination. Using this information and adapting the elements of the Charlson Comorbidity Index[
Objective
The objective of this study was to determine the best predictors of hospital LOS and discharge destination in patients admitted to a neuroscience unit.
MATERIALS AND METHODS
This study was approved by the Winthrop University Hospital Institutional Review Board (#661464-3).
Data collection
Data from patients’ medical record was obtained using the NSAQ [
Study design
This study was a retrospective correlational descriptive study. The dependent variables were the LOS and discharge destination. The independent variables were principle diagnosis, age, physiology on admission, comorbidities, etc., as described above.
Sample
The sample for this study was a convenience sample of patients admitted to any and all units within a neuroscience service line in a 590 bed metropolitan area hospital.
Inclusion criteria
Adult patients admitted to the neuroscience service from November 2014 to September 2015.
Exclusion criteria
Patients under the age of 18 and patients whose complete data were unavailable.
Statistical analysis
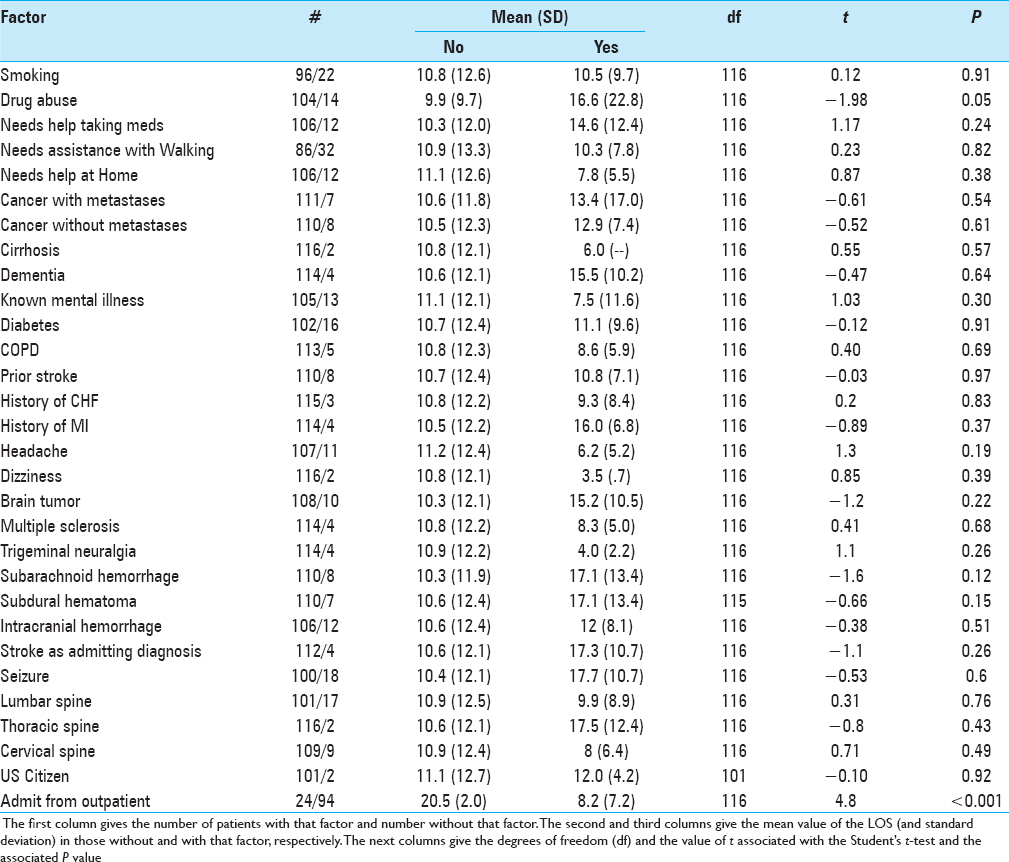
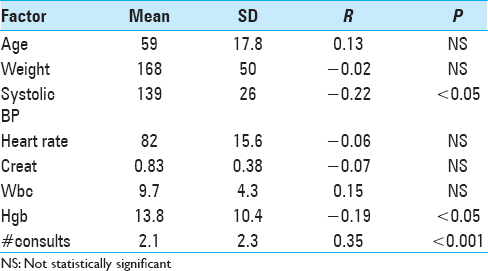
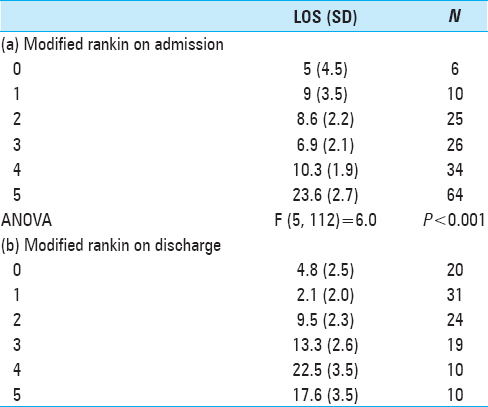
There were 50 binary factors. For each of these a t-test was performed to determine whether the LOS was longer when the factor was present. Using the Bonferroni correction, the significance level for these univariable tests was chosen at. 05/50 or <0.001. For the variables with multiple levels such as the mRS at admission or discharge or the discharge status, an analysis of variance (ANOVA) test was used to determine whether the value of that factor affected LOS. Again a P value of <0.001 was chosen for the significance level. For those variables that took on either many levels or continuous values, a Spearman rank correlation between the variable and the LOS was performed and the significance of the correlation was computed. All variables available on admission with P < 0.05 in the univariate analyses were then entered into a forward stepwise linear regression against the LOS with F to enter of 2 and F to remove of 1 (Statistica, Statsoft Tulsa, OK, USA).
RESULTS
In order to see which of these variables available on admission are most useful in predicting LOS, all of the factors with a strong (P < 0.05) relationship with the LOS were entered into a forward stepwise linear regression with LOS as the dependent variable.
DISCUSSION
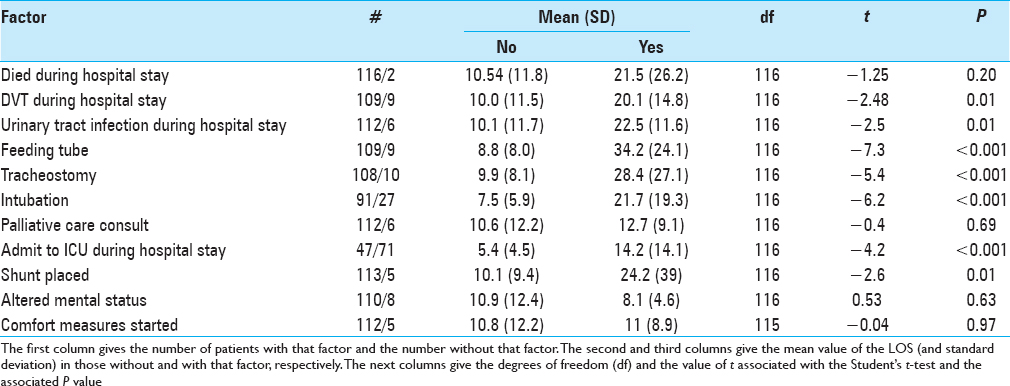
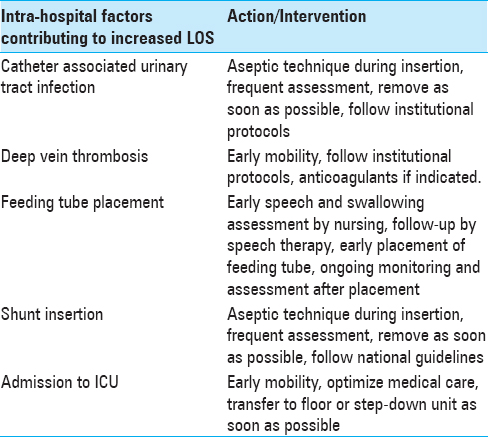
Many factors describing what happened during the hospital stay have a significant relation to the length of stay. The statistically significant factors are discussed below.
Deep venous thrombosis, Cauti, feeding tube placement, intubation, admission to intensive care unit, and shunt insertion
These factors were all determined to have an effect on LOS, and the current literature supports these findings. Okere et al.[
George et al.[
Dasenbrock, et al.[
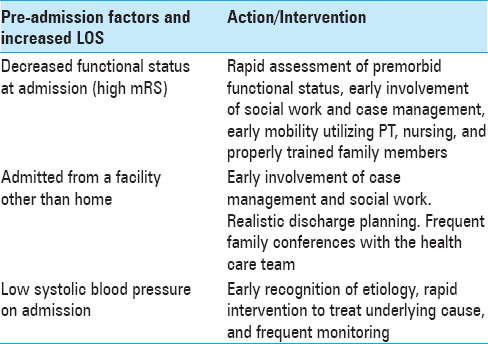
In addition to events that occurred in hospital and their relationship to LOS, the factors at admission that are important are discussed below.
mRS
Saxena et al.[
Sapsosnik et al.[
Dasenbrock et al.[
Patients admitted from another facility (outpatient or inpatient)
Data from this study indicated that patients had a prolonged LOS if they were admitted from other locations such as rehabilitation or nursing home. This data was also validated by the Dasenbrock study,[
Lower systolic blood pressue on admission
In this study, a lower systolic blood pressure at admission was found to be an independent predictor for prolonged LOS. While this finding is not supported in current literature, this variable presents an opportunity for further research into whether this information can be useful in a future model. For example, low systolic blood pressure can signal early stages of sepsis, adverse coronary events, and reduced renal function (except in the case of severe proteinuria[
Intervening to decrease preventable complications
While no institution can escape adverse outcomes, all providers can intervene to prevent complications that can increase LOS. Please refer to Tables
CONCLUSIONS
A number of factors demonstrate that certain circumstances during a hospital stay, whether at admission or occurring during the hospital stay itself, can prolong a patient's length of stay putting them at risk for increased morbidity and/or mortality. These factors include lower systolic blood pressure on admission, higher mRS or decreased functional capacity at admission, the acquisition of a DVT or CAUTI, and being intubated and/or admitted to an ICU can have deleterious effects on patients’ hospital stays. Being vigilant and proactive in recognizing and treating these conditions can help mitigate adverse events and poor outcomes in patients hospitalized on a neuroscience service.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to acknowledge Rebecca Corolian, Sara Zulfiqar and Jaani Gandhi for their help with this manuscript.
References
1. Appelros P. Prediction of length of stay for stroke patients. Acta Neurol Scand. 2007. 116: 15-9
2. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994. 47: 1245-51
3. Dasenbrock HH, Liu KX, Devine CA, Chavakula V, Smith TR, Gormley WB. Length of hospital stay after craniotomy for tumor: A National Surgical Quality Improvement Program analysis. Neurosurg Focus. 2015. 39: E12-
4. De la Garza-Ramos R, Goodwin CR, Abu-Bonsrah N, Jain A, Miller AK, Neuman BJ. Prolonged length of stay after posterior surgery for cervical spondylotic myelopathy in patients over 65 years of age. J Clin Neurosci. 2016. 31: 137-41
5. DeLuzio MR, Keshava HB, Wang Z, Boffa DJ, Detterbeck FC, Kim AW. A model for predicting prolonged length of stay in patients undergoing anatomical lung resection: A National Surgical Quality Improvement Program (NSQIP) database study. Interact Cardiovasc Thorac Surg. 2016. 23: 208-15
6. George A, Boehme AK, Siegler JE, Monlezun D, Fowler BD, Shaban A. Hospital-Acquired Infection Underlies Poor Functional Outcome in Patients with Prolonged Length of Stay. ISRN Stroke 2013. 2013. p.
7. Kawakami K, Hiroshima R, Takaoka H, Koenuma N, Mochizuki T. Risk Factors Affecting Length of Hospital Stay After Total Knee Arthroplasty in Rheumatoid Arthritis and Osteoarthritis Patients. Ann Rheum Dis. 2015. 74: 1064-5
8. Okere AN, Renier CM, Frye A. Predictors of Hospital Length of Stay and Readmissions in Ischemic Stroke Patients and the Impact of Inpatient Medication Management. J Stroke Cerebrovasc Dis. 2016. 25: 1939-51
9. Rosenthal VD, Dwivedy A, Calderón ME, Esen S, Hernández HT, Abouqal R. Time-dependent analysis of length of stay and mortality due to urinary tract infections in ten developing countries: INICC findings. J Infect. 2011. 62: 136-41
10. Saposnik G, Webster F, O’Callaghan C, Hachinski V. Optimizing discharge planning: Clinical predictors of longer stay after recombinant tissue plasminogen activator for acute stroke. Stroke. 2005. 36: 147-50
11. Saxena A, Prasad RN, Verma K, Saxena S. Factors Predicting Length of Hospital Stay in Acute Stroke Patients Admitted in a Rural Tertiary Care Hospital. J Gerontol Geriatr Res. S5: 003-
12. Simonet ML, Kossovsky MP, Chopard P, Sigaud P, Perneger TV, Gaspoz JM. A predictive score to identify hospitalized patients’ risk of discharge to a post-acute care facility. BMC Health Serv Res. 2008. 8: 154-
13. Suarez JI, Zaidat OO, Suri MF, Feen ES, Lynch G, Hickman J. Length of stay and mortality in neurocritically ill patients: Impact of a specialized neurocritical care team. Crit Care Med. 2004. 32: 2311-7
14. Tan WS, Heng BH, Chua KS, Chan KF. Factors predicting inpatient rehabilitation length of stay of acute stroke patients in Singapore. Arch Phys Med Rehabil. 2009. 90: 1202-7
15. Weber MA, Bakris GL, Hester A, Weir MR, Hua TA, Zapp D. Systolic Blood Pressure and Cardiovascular Outcomes During Treatment of Hypertension. Am J Med. 2013. 126: 501-8