- Section of Neurosurgery, Department of Surgery, Providence Hospital and Medical Centers, Southfield and Novi, Southfield, MI, USA
- Michigan Spine and Brain Surgeons, PLLC, Southfield, MI, USA
- Department of Radiology, Providence Hospital and Medical Centers, Southfield, MI, USA
Correspondence Address:
Lee Sandquist
Michigan Spine and Brain Surgeons, PLLC, Southfield, MI, USA
DOI:10.4103/2152-7806.159383
Copyright: © 2015 Sandquist L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Sandquist L, Carr D, Tong D, Gonda R, Soo TM. Preventing proximal junctional failure in long segmental instrumented cases of adult degenerative scoliosis using a multilevel stabilization screw technique. Surg Neurol Int 25-Jun-2015;6:112
How to cite this URL: Sandquist L, Carr D, Tong D, Gonda R, Soo TM. Preventing proximal junctional failure in long segmental instrumented cases of adult degenerative scoliosis using a multilevel stabilization screw technique. Surg Neurol Int 25-Jun-2015;6:112. Available from: http://surgicalneurologyint.com/surgicalint_articles/preventing-proximal-junctional-failure-long-segmental/
Abstract
Background:The authors sought to demonstrate the safety and effectiveness of the multilevel stabilization screw (MLSS) technique in decreasing the incidence of proximal junctional failure in long segmental instrumented fusions for adult degenerative scoliosis.
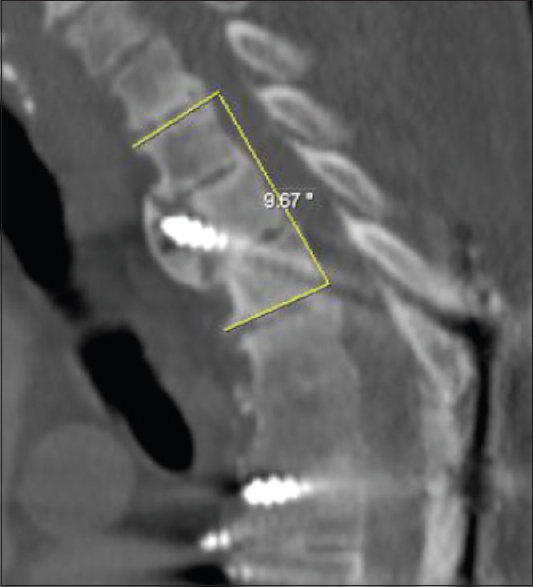
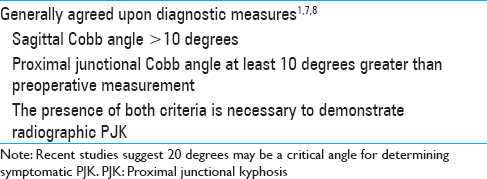
Methods:Institutional review board approval was obtained and all patients with adult spinal deformity who underwent the MLSS technique were analyzed. A neuro-radiologist and spine-focused neurosurgeon not involved with the surgical treatment performed radiographic analysis. Proximal junctional angle was defined as the caudal endplate of the upper instrumented vertebra (UIV) to the cephalad endplate of two supradjacent vertebrae above the UIV. The UIV is defined as the most cephalad vertebra completed captured by the instrumentation. Abnormal proximal junctional kyphosis (PJK) was defined as proximal junctional sagittal Cobb angle >10 degrees and proximal junction sagittal Cobb angle at least 10 degrees greater than the preoperative measurement. The presence of both is criteria necessary to be considered abnormal.
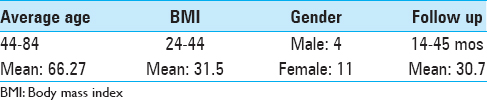
Results:Twenty patients with degenerative scoliosis underwent the MLSS technique with the upper-instrumented vertebrae in the proximal thoracic spine. Fifteen patients met inclusion criteria with greater than 12 months radiographic and clinical follow up. Three patients were excluded due to lack of follow up imaging and two patients were excluded due to the inability to measure the UIV. Age range was 44–84 years with a mean of 66. Eleven of the 15 patients were over the age of 60 at the time of surgery. The male-to-female ratio was 4:11. Body mass index (BMI) range was 24–44 with a mean of 31.5 units. The follow up period ranged from 14 to 58 months with an average follow up of 30 months. The mean change in Cobb angle at the proximal junction was 4.00 degrees with a range from -0.92 to 9.13 degrees. There were no fractures or instrumentation failures at or near the proximal junction. There was no revision surgeries performed for proximal junctional failure. Retrospective clinical questionnaires revealed that surgical expectations were met in 15 of 19 patients surveyed, 79%. One patient was not reachable for a postoperative phone interview. In patients who were not satisfied with their overall experience, the change in Cobb angle ranged from -0.92 to 9.13 degrees with an average change of 3.90 degrees. Whereas patients reporting an overall positive experience had a change in Cobb angle range from -0.12 to 8.07 degrees with an average change of 4.05 degrees.
Conclusion:PJK and failure are well-recognized suboptimal outcomes of long-segmental fusions of the thoracolumbar spine that can lead to significant neurological morbidity and costly revision surgeries. With no known proximal junction failures to date, the MLSS technique has shown promising results in preventing adverse proximal junctional conditions and can be safely performed under fluoroscopy guidance. Future direction includes a comparative study establishing the relative risk of developing PJK with this novel technique versus a traditional long-segmental thoracolumbar fusion.
Keywords: Degenerative scoliosis, long-segmented thoracolumbar instrumentation, proximal junction kyphosis, proximal junctional failure
INTRODUCTION
Adult degenerative scoliosis is a spinal deformity in a skeletally mature individual with a coronal curve that measures >10 degrees using the Cobb method.[
Proximal junctional kyphosis (PJK) and failure has led to the 26–39% requirement for revision surgery within six postoperative months. Multiple risk factors including age greater than 55 and elevated body mass index (BMI) as well as biomechanical hypotheses such as altered integrity of ligamentous and muscular structures have been implicated in the need for second operations.[
This report is to present a technical description and preliminary results of the multilevel stabilization screw (MLSS) technique designed to reduce the incidence of PJK for long-segmental thoracolumbar fusion surgery.
MATERIALS AND METHODS
Institutional review board approval was obtained and all patients with adult spinal deformity who underwent the MLSS technique at a single institution were analyzed.
Inclusion criteria and data collection
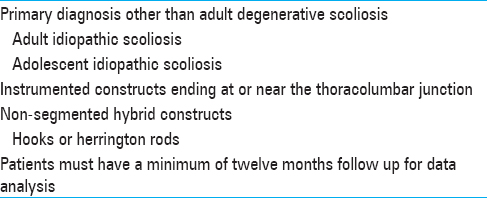
All MLSS procedures were performed at a single institution from 2009 to 2012. Only adults with degenerative scoliosis underwent segmental instrumentation utilizing the MLSS technique with a proximal upper instrumented vertebrae (UIV) in the upper thoracic spine to avoid PJK were included in the study. There were multiple exclusion criteria [
Radiographic analysis
Two independent analysts, a neuro-radiologist and spine-focused neurosurgeon, retrospectively evaluated 20 radiographic studies in a blinded fashion. Cobb angle measurements were performed on sagittal reconstructed CT scans and lateral radiographs.[
Surgical technique
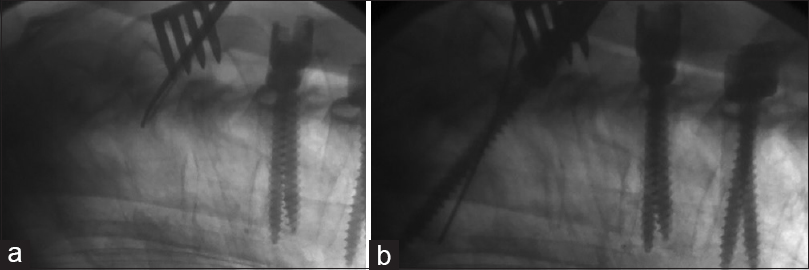
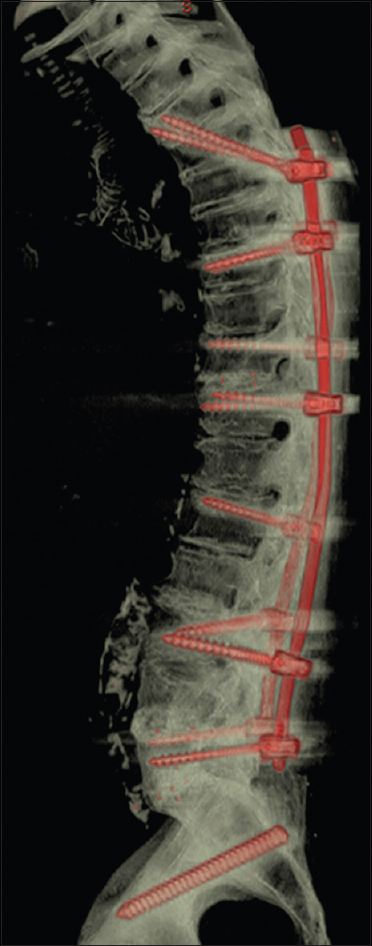
Unique to the MLSS is the preservation of the posterior elements at the cephalad end of the thoracic construct. Soft tissue dissection is carried out to allow for adequate exposure of the inferior lateral aspect of the most superior pedicles involved in the instrumentation. Biplane fluoroscopy guidance is used to ensure achievement of optimal placement. The most superior pedicle screw is started at the inferior lateral aspect of the pedicle. It is directed in a superior and oblique trajectory, which allows for limited dissection of supporting tissue structures. Advancement under fluoroscopy guidance ensures the neural foramina superior and inferior are not encroached upon and the medial cortex of the pedicle is well visualized during instrumentation [
In the AP trajectory, instrumentation should not cross the midline to avoid a medial wall breach of the pedicle and also to prevent screw overlap. The starting point and trajectory capture the pedicle of the vertebra at the same level as well as the vertebral bodies one to two levels superior to the screws’ starting point. A total of four to six cortical surfaces are incorporated into the construct throughout the length of the screw adding to the strength against pullout [
RESULTS
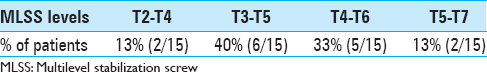
The MLSS screw was placed most often through the T4 vertebral body, T3-T5 at the cephalad end of the construct [
There were no fractures or instrumentation failures at or near the proximal junction when using the MLSS technique. There was no revision surgeries performed for proximal junctional failure.
DISCUSSION
Unique to the MLSS is the preservation of the posterior elements at the cephalad end of the thoracic construct. It is well documented that extension soft tissue dissection and disruption of the posterior tension band is a significant risk factor for developing PJK [
However, this study is not without limitations. Ideally, prospectively gathered outcome measures specific to degenerative scoliosis, such as Scoliosis Research Society or Oswestry disability index, would provide a more relevant view of patient satisfaction. The overall initial sample size is small and the lack of long-term follow up with many patients further diminishes the subject population included in the analysis. Preferably, a larger sample size with multiple surgeons at multiple institutions would increase the credibility of the technique's effectiveness. PJK and failure are well-recognized suboptimal outcomes of long-segmental fusions of the thoracolumbar spine that can lead to significant neurological morbidity and costly revision surgeries.[
References
1. Bridwell KH, Lenke LG, Cho SK, Pahys JM, Zebala LP, Dorward IG. Proximal junctional kyphosis in primary adult deformity surgery: Evaluation of 20 degrees as a critical angle. Neurosurgery. 2013. 72: 899-906
2. Gstoettner M, Sekyra K, Walochnik N, Winter P, Wachter R, Bach CM. Inter- and intraobserver reliability assessment of the Cobb angle: Manual versus digital measurement tools. Eur Spine J. 2007. 16: 1587-92
3. Gupta MC, Wijesekera S, Sossan A, Martin L, Vogel LC, Boakes JL. Reliability of radiographic parameters in neuromuscular scoliosis. Spine. 2007. 32: 691-5
4. Ha Y, Maruo K, Racine L, Schairer WW, Hu SS, Deviren V. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: A comparison of proximal and distal upper instrumented vertebrae: Clinical article. J Neurosurg Spine. 2013. 19: 360-9
5. Hart RA, McCarthy I, Ames CP, Shaffrey CI, Hamilton DK, Hostin R. Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am. 2013. 24: 213-8
6. Hart R, McCarthy I, O’Brien M, Bess S, Line B, Adjei OB. Identification of decision criteria for revision surgery among patients with proximal junctional failure after surgical treatment of spinal deformity. Spine. 2013. 38: E1223-7
7. Hostin R, McCarthy I, O’Brien M, Bess S, Line B, Boachie-Adjei O. Incidence, mode, and location of acute proximal junctional failures following surgical treatment for adult spinal deformity. Spine. 2013. 38: 1008-15
8. Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: Minimum five-year follow-up. Spine. 2008. 33: 2179-84
9. Lapp MA, Bridwell KH, Lenke LG, Daniel Riew K, Linville DA, Eck KR. Long-term complications in adult spinal deformity patients having combined surgery a comparison of primary to revision patients. Spine. 2001. 26: 973-83
10. McClendon J, O’shaughnessy BA, Sugrue PA, Neal CJ, Acosta FL, Koski TR. Techniques for operative correction of proximal junctional kyphosis of the upper thoracic spine. Spine. 2012. 37: 292-303
11. Silva FE, Lenke LG. Adult degenerative scoliosis: Evaluation and management. Neurosurg Focus. 2010. 28: E1-
12. Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis. Spine. 2011. 36: E60-8