- Department of Neurosurgery, Faculty of Medicine, Juntendo University, Tokyo, Japan
Correspondence Address:
Akihide Kondo
Department of Neurosurgery, Faculty of Medicine, Juntendo University, Tokyo, Japan
DOI:10.4103/sni.sni_146_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Akihide Kondo, Osamu Akiyama, Mario Suzuki, Hajime Arai. Prosthetic material degeneration over time as a possible factor in delayed recurrence of hemifacial spasm after successful microvascular decompression. 10-Sep-2018;9:187
How to cite this URL: Akihide Kondo, Osamu Akiyama, Mario Suzuki, Hajime Arai. Prosthetic material degeneration over time as a possible factor in delayed recurrence of hemifacial spasm after successful microvascular decompression. 10-Sep-2018;9:187. Available from: http://surgicalneurologyint.com/surgicalint-articles/8999/
Abstract
Background:The effectiveness of microvascular decompression in treating hemifacial spasm is widely accepted. However, some experience recurrence of hemifacial spasm after successful decompression surgery. Especially, delayed recurrence more than 5 years after surgery is rare and the cause of this phenomenon is unknown.
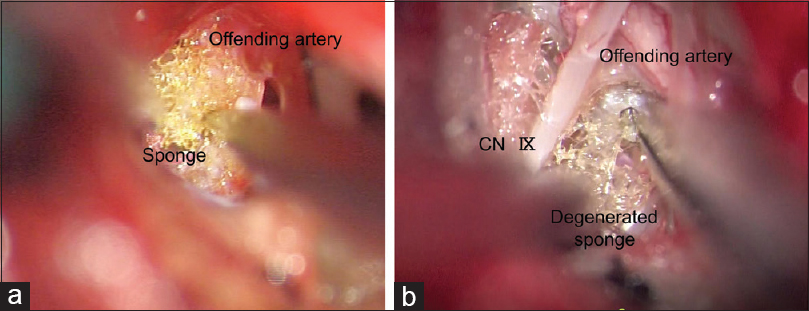
Case Description:A female underwent microvascular decompression to treat her hemifacial spasm 6 years ago. Six years later, her hemifacial spasm recurred and she underwent a second surgery. The second surgery revealed that the sponge had become fragile, losing the ability to absorb the impact of pulsatile compression of the offending artery on the root exit zone of her facial nerve.
Conclusion:We report a case in which degeneration of material, a sponge (polyurethane), used in decompression surgery caused delayed recurrence of hemifacial spasm. The selection of appropriate prosthetic materials is essential in such functional surgeries.
Keywords: Hemifacial spasm, microvascular decompression, prosthesis
INTRODUCTION
One of the standard treatments for hemifacial spasm is microvascular decompression. However, few reports have addressed the mechanism of recurrence after successful decompression surgery. Chang et al. concluded that recurrence after more than 5 years of surgery is rare.[
We encountered a case showing recurrence of hemifacial spasm 6 years after successful decompression surgery. Our surgical findings indicated prosthetic material degeneration over time resulting in loss of prosthetic function. We caution that a similar choice of prosthetic material for decompression may cause delayed recurrence of hemifacial spasm after initial success in decompression surgery.
CASE DESCRIPTION
A 48-year-old female had a 2-year history of right hemifacial spasm. She had been treated with clonazepam and other alternative therapies with limited effect. She was admitted to our hospital for microvascular decompression surgery for her hemifacial spasm. Preoperative magnetic resonance imaging (MRI) with T2-based cisternography revealed attachment of her right posterior inferior cerebellar artery (PICA) to her facial nerve exit zone. We carried out microvascular decompression surgery with a lateral suboccipital approach and placed a sponge (polyurethane) between the PICA and the brainstem, fixing them with fibrin glue [
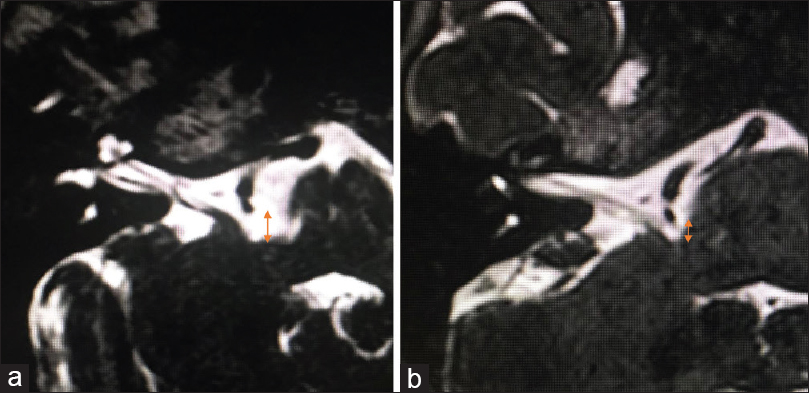
Figure 2
(a) T2-based cisternography immediately after the first surgery. The PICA was located far from the brainstem. (b) T2-based cisternography at the time of recurrence. The distance from the brainstem of PICA was narrowed when compared with that in
Six years after her surgery, she noticed a mild spasm in her superior orbicularis oculi muscle which spread to her prioral muscles and occasionally sustained a tonic state. She visited our department and underwent a MRI scan. T2-based cisternography showed a closed PICA running course compared with the MRI immediately after her initial surgery [
Using a lateral suboccipital approach through the previous incision and craniotomy, we dissected the arachnoid adhesion and confirmed that the sponge placed in the first surgery between the offending artery and the brainstem was not dislocated. However, the sponge was degenerated. The structure of the sponge was fragile and easy to collapse. The honeycomb structure or bubbles in the sponge were not preserved [
DISCUSSION
Microvascular decompression as a treatment for hemifacial spasm has been very safe due to the progress in intraoperative monitoring including auditory brainstem response and surgical techniques.[
Contrarily, the cause of delayed recurrence after initially successful decompression surgery has remained unclear. The major reasons proposed for delayed recurrence in previous reports included shift of prosthesis, vascular rerouting due to atherosclerosis, and incomplete decompression procedures.[
Sponge can be a good material to use in microvascular decompression.[
Because delayed recurrence of facial spasm is rare, it is challenging to detect and study. A recent report showed that fluoroscope-guided facial nerve block and pulsed radiofrequency treatment might be effective for patients with recurrent facial spasm.[
We report a case of delayed recurrence of hemifacial spasm after initial successful decompression surgery due to prosthetic material degeneration over time. Our report indicates that the use of similar materials may cause such delayed spasm recurrence after microvascular decompression surgery and highlights the need for use of appropriate prosthetic materials.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors are thankful to the patient for her co-operation. This study was supported by the Juntendo University Research Institute for Diseases of Old Age (Tokyo, Japan).
References
1. Barker FG, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD. Microvascular decompression for hemifacial spasm. J Neurosurg. 1995. 82: 201-10
2. Chang WS, Chung JC, Kim JP, Chung SS, Chang JW. Delayed recurrence of hemifacial spasm after successful microvascular decompression: Follow-up results at least 5 years after surgery. Acta Neurochir (Wien). 2012. 154: 1613-9
3. Dou NN, Zhong J, Liu MX, Xia L, Sun H, Li B. Teflon might be a factor accounting for a failed microvascular decompression in hemifacial spasm: A technical note. Stereotact Funct Neurosurg. 2016. 94: 154-8
4. Fargen KM, Blackburn S. Surgical decompression for optic neuropathy from carotid artery ectasia: Case report with technical considerations. World Neurosurg. 2014. 82: 239.e9-12
5. Jiang C, Xu W, Dai Y, Lu T, Jin W, Liang W. Failed microvascular decompression surgery for hemifacial spasm: A retrospective clinical study of reoperations. Acta Neurochir (Wien). 2017. 159: 259-63
6. Lin CF, Chen HH, Hernesniemi J, Lee CC, Liao CH, Chen SC. An easy adjustable method of ectatic vertebrobasilar artery transposition for microvascular decompression. Clin Neurol Neurosurg. 2012. 114: 951-6
7. Park HL, Lim SM, Kim TH, Kang KH, Kang H, Jung YH. Intractable hemifacial spasm treated by pulsed radiofrequency treatment. Korean J Pain. 2013. 26: 62-4
8. Rhee DJ, Kong DS, Park K, Lee JA. Frequency and prognosis of delayed facial palsy after microvascular decompression for hemifacial spasm. Acta Neurochir (Wien). 2006. 148: 839-43
9. Sindou MP. Microvascular decompression for primary hemifacial spasm. Importance of intraoperative neurophysiological monitoring. Acta Neurochir (Wien). 2005. 147: 1019-26
10. Xu XL, Zhen XK, Yuan Y, Liu HJ, Liu J, Xu J. Long-term outcome of repeat microvascular decompression for hemifacial spasm. World Neurosurg. 2018. 110: e989-97
11. Zhao H, Zhang X, Tang YD, Zhang Y, Ying TT, Zhu J. Operative complications of microvascular decompression for hemifacial spasm: Experience of 1548 cases. World Neurosurg. 2017. 107: 559-64