- University at Buffalo School of Medicine, Buffalo, New York, USA
- Section of Neurosurgery, University of Chicago, Evanston, Illinois, USA
- Division of Otolaryngology, Northshore University Health System, Evanston, Illinois, USA
- Department of Neurosurgery, Northshore University Health System, Evanston, Illinois, USA
Correspondence Address:
Ricky H. Wong
Department of Neurosurgery, Northshore University Health System, Evanston, Illinois, USA
DOI:10.4103/sni.sni_243_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Andrew K. Wong, Melissa M. Stamates, Anita P. Bhansali, Michael Shinners, Ricky H. Wong. Radiographic Assessment of the presigmoid retrolabyrinthine approach. 27-Jun-2017;8:129
How to cite this URL: Andrew K. Wong, Melissa M. Stamates, Anita P. Bhansali, Michael Shinners, Ricky H. Wong. Radiographic Assessment of the presigmoid retrolabyrinthine approach. 27-Jun-2017;8:129. Available from: http://surgicalneurologyint.com/surgicalint-articles/radiographic-assessment-of-the-presigmoid-retrolabyrinthine-approach/
Abstract
Background:Lesions of the petroclival fissure are difficult to access surgically. Both retrosigmoid and presigmoid retrolabyrinthine approaches have been described to successfully treat these complex tumors. The retrosigmoid approach offers quick and familiar access, whereas the presigmoid retrolabyrinthine approach reduces the operative distance and the need for cerebellar retraction. The presigmoid retrolabyrinthine approach, however, is constrained by anatomical limits that can be subject to patient variation. We sought to characterize the surgically relevant variation to guide preoperative assessment.
Methods:One hundred and seventy-seven high-resolution computed tomography scans of the head (without preexisting pathology) were reviewed. Three hundred and fifty-four temporal bone scans were analyzed for level of aeration, size of Trautmann's triangle dura, and petrous slope. Petrous slope is the angle between the anterior sigmoid sinus and the petroclival fissure at the level of the internal acoustic canal.
Results:Trautmann's triangle area had a mean of 185.15 mm2 (range 71.4–426.7 mm2). Petrous slope had a mean value of 149° (range 106–178°). Increasing aeration was found to be correlated with decreasing petrous slope and decreasing Trautmann's triangle area.
Conclusion:The presigmoid retrolabyrinthine approach is uniquely confined. Variations in temporal bone anatomy can have dramatic impacts on the operative time, risk profile, and final exposure. Preoperative assessment is critical in guiding the surgeon on the appropriateness of approach. Preoperative measurement of Trautmann's triangle, petrous slope, and aeration can help to reduce surgical morbidity.
Keywords: Petrocival, presigmoid, retrolabyrinthine, retrosigmoid, surgical anatomy, temporal bone
INTRODUCTION
Lesions of the petroclival region have been described as “formidable, untreatable, or both.”[
The decision to pursue a retrosigmoid versus a presigmoid retrolabyrinthine (henceforth referred to as presigmoid) approach has generally been predicated on patient anatomy, pathology (location and characteristics), and surgeon preference. Previously described specific preoperative radiographic anatomy includes level of petrous bone aeration and height of jugular bulb.[
Trautmann's triangle is an area of dura exposed via a retrolabyrinthine approach, and represents the posterior transpetrosal window to the posterior fossa that preserves hearing. It is bordered by the superior jugular bulb, the sinodural angle, and the posterior semicircular canal.[
Given that the individual variability of this operating space has been demonstrated only in small cadaveric studies,[
MATERIALS AND METHODS
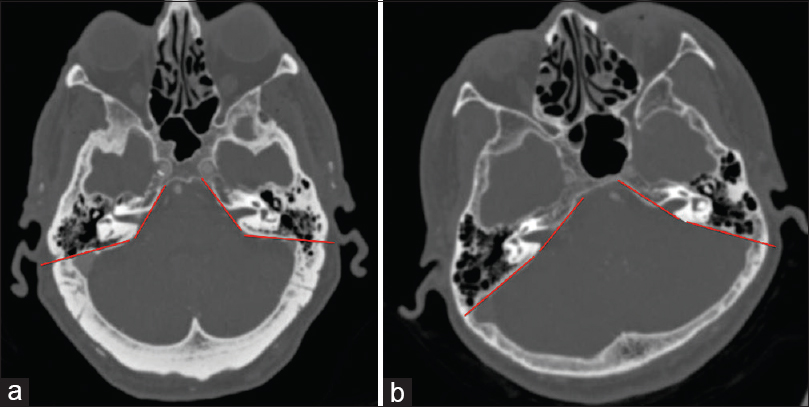
An institutional review board approval was obtained (EH15-319) to select a sample of 200 computed tomography (CT) scans obtained through the head according to a CT angiography protocol from the previous year. Twenty-three scans were excluded due to duplicate exams or temporal bone pathology. Three hundred and fifty-four total temporal bones were examined and data recorded. 0.6 mm thick slices in the axial and coronal planes of each scan were examined for distance from jugular bulb to petrous ridge (JB–PR), distance from posterior semicircular canal (PSCC) to sigmoid sinus (PSCC–SS), and the “petrous slope” defined as the angle between the anterior sigmoid sinus and the petroclival fissure at the level of the internal auditory canal (IAC) [
Because the boundaries of Trautmann's triangle generate a rhomboid-shaped safe zone of dura, the JB–PR and PSCC–SS distances were multiplied to generate an estimated area of dural exposure. This rhomboid area, level of aeration, and the measured petrous slope were analyzed for any statistical correlation.
RESULTS
In left-sided temporal bones, the distance between the jugular bulb (JB) and petrous ridge averaged 16.75 mm (range 9–25.1 mm); the average distance from PSCC to the anterior sigmoid sinus was 11.85 mm (range 6.57–23.25 mm) and the mean measured left petrous slope was 150.26° (range 106–178°). On right-sided temporal bones, the JB to petrous ridge height averaged 16.3 mm (range 9.5–30.7 mm), the distance from PSCC to anterior sigmoid sinus averaged 10.51 mm (range 4.66–19.5 mm) and the mean measured right petrous slope was 148.58° (range 116.2–178°). The area of Trautmann's triangle, calculated by multiplying the JB–PR and PSCC–SS distances for each temporal bone, averaged 185.15 mm2 (range 71.4–426.7 mm2).
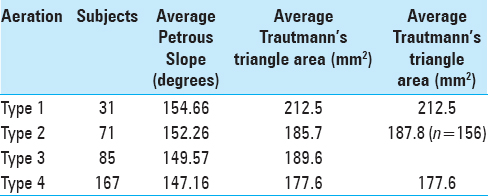
Increasing temporal bone aeration displayed a trend towards decreasing petrous slope values, however, this did not reach statistical significance [
DISCUSSION
In this study, we characterized individual variability in temporal bone anatomy in 177 patients. We captured this variation across three variables that we believe significantly impact surgical considerations when performing a presigmoid retrolabyrinthine approach. Significant ranges were found in aeration, Trautmann's triangle area (355.3 mm2), and petrous slope (72°). Moreover, there was a trend towards decreasing petrous slope and decreasing Trautmann's triangle area with increasing levels of aeration. This suggests that extension of aeration beyond the posterior border of the sigmoid sinus may portend a more difficult and less expansive presigmoid exposure. Aeration may play a more significant role in the presigmoid exposure than our measurement, particularly at extremes; other authors have found the position of the sigmoid sinus to carry more significance.[
In 1980, the retrolabyrinthine approach was described as the “direct”[
The technical elements of a presigmoid approach make it susceptible to three specific anatomic characteristics – level of temporal bone aeration, size of Trautmann's triangle, and the angle of the petrous slope. Significant temporal bone aeration can facilitate intraoperative identification of anatomic landmarks (labyrinth, fallopian canal) and can dramatically reduce the exposure time. A poorly aerated or sclerotic temporal bone, on the other hand, can make adequate exposure both treacherous and time consuming.
Variation in the height of the jugular bulb has been well described.[
DeMelo et al. described a laterally displaced sigmoid sinus as requiring a more technically demanding mastoidectomy with a narrow surgical corridor to the petroclival region when compared to a medially displaced sigmoid sinus. They noted a theoretical increased risk of injury to the facial nerve because of its close relation with the sigmoid sinus.[
Our large analysis of 177 computed tomography scans of 354 temporal bones attempted to establish a simple and reliable method of systematically assessing the presigmoid retrolabyrinthine approach using preoperative imaging. We found three factors that varied considerably among individuals – aeration, Trautmann's triangle area, and petrous slope. Interestingly, increasing levels of aeration decreased the petrous slope and decreased the area of Trautmann's triangle. The indirect relationship of decreasing petrous slope with decreasing Trautmann's triangle area confirms previous cadaveric analysis on the impact of sigmoid sinus anatomy on Trautmann's triangle.[
CONCLUSIONS
The presigmoid, retrolabyrinthine approach represents a versatile skull base technique to access the lateral and ventrolateral posterior fossa. While it shortens the working distance and reduces the need for cerebellar retraction, it requires additional time for petrosal bone drilling and increases the risk of spinal fluid leak and hearing loss. Careful preoperative planning is critical to reduce the inherent risks, plan technique modifications (and prepare for the additional time required), and ensure the appropriateness of the approach altogether. Calculating Trautmann's triangle area, the petrous slope, and the extent of aeration can nuance the skull base surgeon's considerations when deciding on whom and how to perform the presigmoid approach.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Mefty O, Fox JL, Smith RR. Petrosal approach for petroclival meningiomas. Neurosurgery. 1988. 22: 510-7
2. Aslan A, Falcioni M, Russo A, De Donato G, Balyan FR, Taibah A. Anatomical considerations of high jugular bulb in lateral skull base surgery. J Laryngol Otol. 1997. 111: 333-6
3. Behari S, Tyagi I, Banerji D, Kumar V, Jaiswal AK, Phadke RV. Postauricular, transpetrous, presigmoid approach for extensive skull base tumors in the petroclival region: The successes and the travails. Acta Neurochir (Wien). 2010. 152: 1633-45
4. Bento RF, De Brito RV, Sanchez TG, Miniti A. The transmastoid retrolabyrinthine approach in vestibular schwannoma surgery. Otolaryngol Head Neck Surg. 2002. 127: 437-41
5. Bento RF, Monteiro TA, Tsuji RK, Gomez MQ, Hausen Pinna M, Goffi-Gomez MV. Retrolabyrinthine approach for surgical placement of auditory brainstem implants in children. Acta Otolaryngol. 2012. 132: 462-6
6. Colasanti R, Tailor AR, Lamki T, Zhang J, Ammirati M. Maximizing the petroclival region exposure via a suboccipital retrosigmoid approach: Where is the intrapetrous internal carotid artery?. Neurosurgery. 2015. 11: 329-36
7. d’Avella D, Mazzoni A, Zanoletti E, Martini A. Microsurgical endoscopy-assisted presigmoid retrolabyrinthine approach as a minimally invasive surgical option for the treatment of medium to large vestibular schwannoma. Acta Neurochir (Wien). 2013. 155: 671-3
8. de Melo JOJ, Klescoski JJ, Nunes CF, Cabral GA, Lapenta MA, Landeiro JA. Predicting the presigmoid retrolabyrinthine space using a sigmoid sinus tomography classification: A cadaveric study. Surgical Neurol Int. 2014. 5: 131-
9. Hakuba A, Nishimura S, Inoue Y. Transpetrosal-transtentorial approach and its application in the therapy of retrochiasmatic craniopharyngiomas. Surg Neurol. 1985. 24: 405-15
10. Han SJ, Song MH, Kim J, Lee WS, Lee HK. Classification of temporal bone pneumatization based on sigmoid sinus using computed tomography. Clin Radiol. 2007. 62: 1110-8
11. Kawase T, Toya S, Shiobara R, Mine T. Transpetrosal approach for aneurysms of the lower basilar artery. J Neurosurg. 1985. 63: 857-61
12. Kinney SE, Hughes GB, Little JR. Retrolabyrinthine transtentorial approach to lesions of the anterior cerebellopontine angle. Am J Otol. 1992. 13: 426-30
13. Kusumi M, Fukushima T, Aliabadi H, Mehta AI, Noro S, Rosen CL. Microplate-bridge technique for watertight dural closures in the combined petrosal approach. Neurosurgery. 2012. 70: 264-9
14. Leung R, Samy RN, Leach JL, Murugappan S, Stredney D, Wiet G. Radiographic anatomy of the infracochlear approach to the petrous apex for computer-assisted surgery. Otol Neurotol. 2010. 31: 419-23
15. Meneses MS, Moreira AL, Bordignon KC, Pedrozo AA, Ramina R, Nikoski JG. Surgical approaches to the petrous apex: Distances and relations with cranial morphology. Skull Base. 2004. 14: 9-19
16. Ramina R, Neto MC, Fernandes YB, Silva EB, Mattei TA, Aguiar PH. Surgical removal of small petroclival meningiomas. Acta Neurochir (Wien). 2008. 150: 431-8
17. Rhoton AL, Tedeschi H. Lateral approaches to the cerebellopontine angle and petroclival region (honored guest lecture). Clin Neurosurg. 1994. 41: 517-45
18. Russell SM, Roland JT, Golfinos JG. Retrolabyrinthine craniectomy: The unsung hero of skull base surgery. Skull Base. 2004. 14: 63-71
19. Samii M, Ammirati M, Mahran A, Bini W, Sepehrnia A. Surgery of petroclival meningiomas: Report of 24 cases. Neurosurgery. 1989. 24: 12-7
20. Samii M, Tatagiba M, Carvalho GA. Resection of large petroclival meningiomas by the simple retrosigmoid route. J Clin Neurosci. 1999. 6: 27-30
21. Sarmiento PB, Eslait FG. Surgical classification of variations in the anatomy of the sigmoid sinus. Otolaryngol Head Neck Surg. 2004. 131: 192-9
22. Silverstein H, McDaniel A, Wazen J, Norrell H. Retrolabyrinthine vestibular neurectomy with simultaneous monitoring of eighth nerve and brain stem auditory evoked potentials. Otolaryngol Head Neck Surg. 1985. 93: 736-42
23. Silverstein H, Norrell H. Retrolabyrinthine surgery: A direct approach to the cerebellopontine angle. Otolaryngol Head Neck Surg. 1980. 88: 462-9
24. Siwanuwatn R, Deshmukh P, Figueiredo EG, Crawford NR, Spetzler RF, Preul MC. Quantitative analysis of the working area and angle of attack for the retrosigmoid, combined petrosal, and transcochlear approaches to the petroclival region. J Neurosurg. 2006. 104: 137-42
25. Spallone A, Makhmudov UB, Mukhamedjanov DJ, Tcherekajev VA. Petroclival meningioma. An attempt to define the role of skull base approaches in their surgical management. Surg Neurol. 1999. 51: 412-9
26. Tahara A, de Santana PA, Calfat Maldaun MV, Panagopoulos AT, da Silva AN, Zicarelli CA. Petroclival meningiomas: Surgical management and common complications. J Clin Neurosci. 2009. 16: 655-9
27. Tedeschi H, Rhoton AL. Lateral approaches to the petroclival region. Surg Neurol. 1994. 41: 180-216
28. Tubbs RS, Griessenauer C, Loukas M, Ansari SF, Fritsch MH, Cohen-Gadol AA. Trautmann's triangle anatomy with application to posterior transpetrosal and other related skull base procedures. Clin Anat. 2014. 27: 994-8
29. Velho V, Agarwal V, Mally R, Palande DA. Posterior fossa meningioma “our experience” in 64 cases. Asian J Neurosurg. 2012. 7: 116-24
30. Woo CK, Wie CE, Park SH, Kong SK, Lee IW, Goh EK. Radiologic analysis of high jugular bulb by computed tomography. Otol Neurotol. 2012. 33: 1283-7