- Division of Neurosurgery, Ascension Providence Hospital, College of Human Medicine, Michigan State University, Michigan, United States
Correspondence Address:
Dejan Slavnic
Division of Neurosurgery, Ascension Providence Hospital, College of Human Medicine, Michigan State University, Michigan, United States
DOI:10.25259/SNI-137-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Dejan Slavnic, Doris Tong, Ryan Barrett, Teck-Mun Soo. Repair of encephalocele and cerebrospinal fluid leak with the use of bone morphogenetic protein: A case report. 24-Apr-2019;10:55
How to cite this URL: Dejan Slavnic, Doris Tong, Ryan Barrett, Teck-Mun Soo. Repair of encephalocele and cerebrospinal fluid leak with the use of bone morphogenetic protein: A case report. 24-Apr-2019;10:55. Available from: http://surgicalneurologyint.com/surgicalint-articles/9297/
Abstract
Background:Encephaloceles are rare phenomena which occur when brain parenchyma herniates through a skull defect which, if left untreated, may lead to significant issues such as cerebrospinal fluid (CSF) fistulas, meningitis, and intractable seizures. Due to the rarity and variety in size and location of encephaloceles, no standard technique has been established for the resultant defect. Herein, we demonstrate the safe and effective use of bone morphogenetic protein (BMP) in the repair of CSF leak caused by encephalocele.
Case Description:A retrospective chart review was conducted on a 50-year-old female who presented with sudden onset spontaneous right nostril CSF leak due to the right lateral sphenoid sinus recess encephalocele, for which she underwent surgical repair. After resecting the encephalocele, cadaver crushed bone was used to fill the skull base defect. Following, an absorbable sponge from the extra-small BMP kit was cut in half and soaked with recombinant human BMP-2 (rhBMP-2) before being laid over the bony defect. On postoperative clinic visits at 2 weeks and at 3 months, the patient demonstrated good recovery without evidence of recurrent CSF leak. On follow-up computed tomography imaging at 9 months’ postsurgery, there was no evidence of recurrent CSF leak or encephalocele, infection, ectopic bone formation, excessive inflammation, or neoplasm.
Conclusion:In this case, we demonstrate the successful use of BMP for the repair of CSF leak due to encephalocele. It is our extrapolation that the pro-inflammatory properties of rhBMP-2 lead to the prevention of recurrent CSF leak.
Keywords: Bone morphogenetic protein, cerebrospinal fluid leak, encephalocele, encephalocele repair
INTRODUCTION
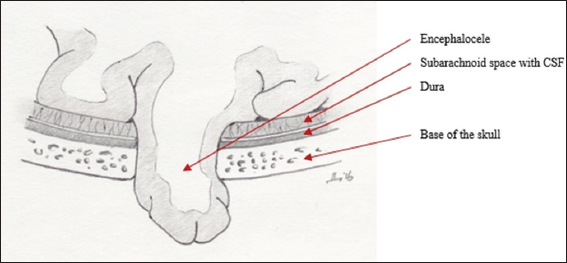
A herniation of brain parenchyma through a skull defect is considered to be heterotopic brain tissue known as encephalocele [
We present a case of spontaneous right lateral sphenoid sinus encephalocele with CSF leak in a 50-year-old female who underwent a right middle fossa craniotomy for resection of the encephalocele. In our institution, we have developed a technique for the repair of dural defect for recurrent CSF leak with the use of recombinant human bone morphogenetic protein-2 (rhBMP-2) after transsphenoidal pituitary resection. BMPs are signaling molecules and belong to a superfamily of proteins known as transforming growth factor-β that are mostly involved in osteogenesis.[
CASE REPORT
A 50-year-old female without a significant history of infection, tumor, or trauma presented to the neurosurgery clinic with profuse watery drainage from her right nostril. The drainage was found to be consistent with CSF. The computed tomography (CT) and magnetic resonance imaging demonstrated a defect in the middle cranial fossa on the right with the encephalocele extending into the sphenoid sinus [
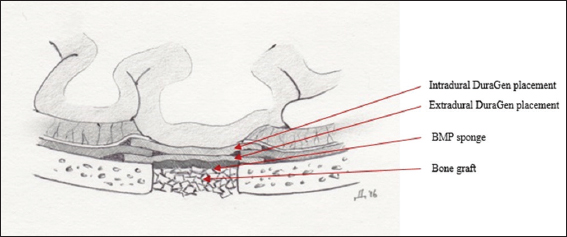
A lumbar drain was inserted before surgery. A right temporal craniotomy was performed in a standard fashion. Using the microscope, the dura was separated from the middle cranial fossa until the dural defect and encephalocele were identified. The encephalocele was pulled through the bony defect. At this point, the dura was incised. The temporal lobe was identified and gently lifted to expose the encephalocele which was protruding through the dural defect. Following, the encephalocele was resected and was measuring 2 cm × 2 cm × 0.4 cm. The bony defect was then repaired by tamping crushed cancellous cadaver bone into the opening. The absorbable sponge from the extra-small BMP kit was soaked with rhBMP-2, cut in half, and laid over the bony defect. A piece of collagen matrix (DuraGen®) was placed above the BMP sponge to completely cover the BMP. Another piece of DuraGen® was laid inside the dural defect due to the lack of access to the dural defect for primary repair [
The lumbar drain remained in place and was open to drain for 7 days. The patient was discharged home on the postoperative day 8. She was followed up clinically at 2 weeks, 3 months, and 9 months after the surgery. CT scan at 9 months’ postsurgery showed no findings to indicate recurrent CSF leak, encephalocele, infection, extraneous bony growth, excessive inflammation, or neoplasm [
DISCUSSION
Encephaloceles are uncommon abnormalities of brain tissue herniations through a skull defect that can be of congenital, iatrogenic, posttraumatic, or spontaneous origin.[
In our case, we were able to show a safe and effective technique for the repair of CSF leak secondary to the right lateral sphenoid sinus recess encephalocele with the use of BMP. In 2002, rhBMP-2 was approved by the United States Food and Drug Administration for use in lumbar fusions due to its osteoinductive properties.[
In recent years, articles have been published on complications associated with the use of BMP that includes ectopic bone formation, osteolysis, and malignancies with higher BMP dose formulations.[
CONCLUSIONS
Encephaloceles are rare brain parenchymal herniations through a skull defect, that if left untreated may lead to CSF fistula formations, seizures, and meningitis. Here we demonstrate a safe application of BMP in the repair of encephalocele and persistent CSF leak.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bano S, Chaudhary V, Yadav SN, Garga UC. Occult spontaneous lateral intrasphenoidal encephalocele:A rare presentation. J Neurosci Rural Pract. 2013. 4: S109-11
2. Cahill KS, McCormick PC, Levi AD. A comprehensive assessment of the risk of bone morphogenetic protein use in spinal fusion surgery and postoperative cancer diagnosis. J Neurosurg Spine. 2015. 23: 86-93
3. Carragee EJ, Chu G, Rohatgi R, Hurwitz EL, Weiner BK, Yoon ST. Cancer risk after use of recombinant bone morphogenetic protein-2 for spinal arthrodesis. J Bone Joint Surg Am. 2013. 95: 1537-45
4. Gonen L, Handzel O, Shimony N, Fliss DM, Margalit N. Surgical management of spontaneous cerebrospinal fluid leakage through temporal bone defects--case series and review of the literature. Neurosurg Rev. 2016. 39: 141-50
5. Huang RL, Yuan Y, Tu J, Zou GM, Li Q. Exaggerated inflammatory environment decreases BMP-2/ACS-induced ectopic bone mass in a rat model:Implications for clinical use of BMP-2. Osteoarthritis Cartilage. 2014. 22: 1186-96
6. Lobo BC, Baumanis MM, Nelson RF. Surgical repair of spontaneous cerebrospinal fluid (CSF) leaks:A systematic review. Laryngoscope Investig Otolaryngol. 2017. 2: 215-24
7. Louie PK, Hassanzadeh H, Singh K. Epidemiologic trends in the utilization, demographics, and cost of bone morphogenetic protein in spinal fusions. Curr Rev Musculoskelet Med. 2014. 7: 177-81
8. Martín-Martín C, Martínez-Capoccioni G, Serramito-García R, Espinosa-Restrepo F. Surgical challenge:Endoscopic repair of cerebrospinal fluid leak. BMC Res Notes. 2012. 5: 459-
9. Roehm PC, Tint D, Chan N, Brewster R, Sukul V, Erkmen K. Endoscope-assisted repair of CSF otorrhea and temporal lobe encephaloceles via keyhole craniotomy. J Neurosurg. 2018. 128: 1880-4
10. Sheikh Z, Javaid MA, Hamdan N, Hashmi R. Bone regeneration using bone morphogenetic proteins and various biomaterial carriers. Materials (Basel). 2015. 8: 1778-816
11. Slavnic D, Cook R, Bahoura M, Paik G, Tong D, Houseman C. Bone morphogenetic protein in the repair of cerebrospinal fluid leak after transsphenoidal surgery. Asian J Neurosurg. 2018. 13: 1279-
12. Tebruegge M, Curtis N. Epidemiology, etiology, pathogenesis, and diagnosis of recurrent bacterial meningitis. Clin Microbiol Rev. 2008. 21: 519-37
13. Wind JJ, Caputy AJ, Roberti F. Spontaneous encephaloceles of the temporal lobe. Neurosurg Focus. 2008. 25: E11-