- Department of Neurological Surgery, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, USA
Correspondence Address:
Paul Page
Department of Neurological Surgery, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin, USA
DOI:10.4103/sni.sni_32_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Paul Page, David Niemann, Colin Son, Yiping Li. Retained distal protection device during carotid artery stenting necessitating carotid endarterectomy: A complication and management considerations. 19-Jun-2018;9:123
How to cite this URL: Paul Page, David Niemann, Colin Son, Yiping Li. Retained distal protection device during carotid artery stenting necessitating carotid endarterectomy: A complication and management considerations. 19-Jun-2018;9:123. Available from: http://surgicalneurologyint.com/surgicalint-articles/retained-distal-protection-device-during-carotid-artery-stenting-necessitating-carotid-endarterectomy-a-complication-and-management-considerations/
Abstract
Background:Neuroendovascular techniques have significantly altered the treatment paradigm of cerebrovascular diseases. Since the introduction of distal cerebral protection devices (DCPD), the incidence of embolic strokes during carotid artery stenting (CAS) has been significantly reduced. Treatment guidelines for retained foreign bodies in the cerebral vasculature do not exist.
Case Description:Here, we present the case of an 88-year-old male who, during carotid artery angioplasty and stenting for symptomatic carotid artery stenosis, suffered from a retained distal protection device ultimately requiring open surgical carotid endarterectomy including removal of the retained device and stent.
Conclusions:Carotid artery angioplasty and stenting utilizing distal protection devices is a commonly employed technique that may rarely result in retained devices. Knowledge of how to retrieve foreign bodies and the salvage techniques are essential to prevent complications from CAS.
Keywords: Carotid stent, foreign body, retained device
INTRODUCTION
Neuroendovascular techniques have significantly altered the treatment paradigm of cerebrovascular diseases. Indications continue to expand with improvements in adjunctive devices that have made endovascular surgery safer and more effective. Despite these advances, embolic events continue to be one of the most devastating complications associated with intraluminal procedures.
Since the introduction of distal cerebral protection devices (DCPD), the incidence of embolic strokes during carotid artery stenting (CAS) has been significantly reduced.[
Treatment guidelines for retained foreign bodies in the cerebral vasculature do not exist. Medical management using antiplatelet and anticoagulants have been successful in the treatment of retained microcatheters and wires. Free floating devices, such as aberrant coil loops, are often removed or immobilized due to higher risk of embolic complications. We describe a rare case of DCPD detainment after CAS and provide a detailed discussion of the evaluation and treatment options.
CASE REPORT
The patient was an elderly male with a past medical history of hypertension, dyslipidemia, and prior deep vein thrombosis on rivaroxaban who initially presented with 2 days of word finding difficulties. On initial presentation, he was found to have a moderate-to-severe mixed aphasia and mild right-sided pronator drift. CTA imaging showed evidence of severe stenosis in the left common carotid artery and there was evidence of low density on computed tomography (CT) in the middle cerebral artery distribution which was consistent with subacute infarction. Given his acute symptoms, the decision was made to proceed with intervention in a delayed fashion.
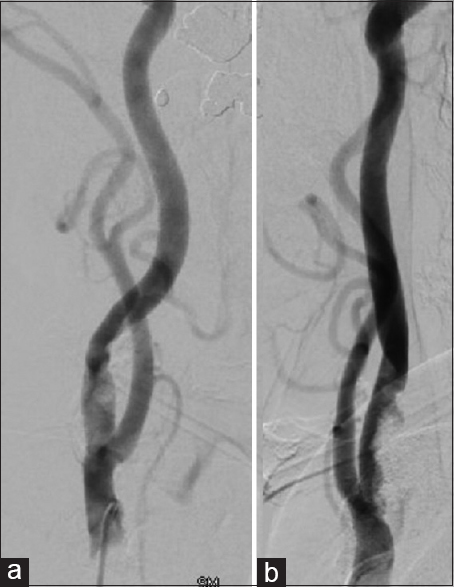
After discharge, the patient was started on aspirin and clopidogrel which were titrated based on his platelet reactivity units and arachidonic acid levels. The patient returned for scheduled CAS 2 months after his prior admission. The procedure occurred in the usual fashion under monitored anesthesia care and commenced without complications. Initial anteroposterior and lateral common carotid artery (CCA) injections demonstrated severe stenosis of 3 mm in diameter occurring just distal to the bifurcation of the common carotid artery [
At this point, an attempt was made to retrieve the Spider FX distal protection device; however, both ends of the recapture device were unable to be retracted. Repeat angiograms in multiple projections continued to show successful stent deployment with improved luminal diameter. Numerous attempts were made to navigate through the stent over the Spider FX wire an angioplasty balloon, diagnostic catheter, or dilator sheath, but all attempts were unsuccessful. Interval angiograms continued to demonstrate adequate flow through the stent without evidence of intraluminal complications such as dissection or thrombosis. After tedious intraluminal manipulation, a 017 microcatheter could traverse the stent but was too small to recapture the device.
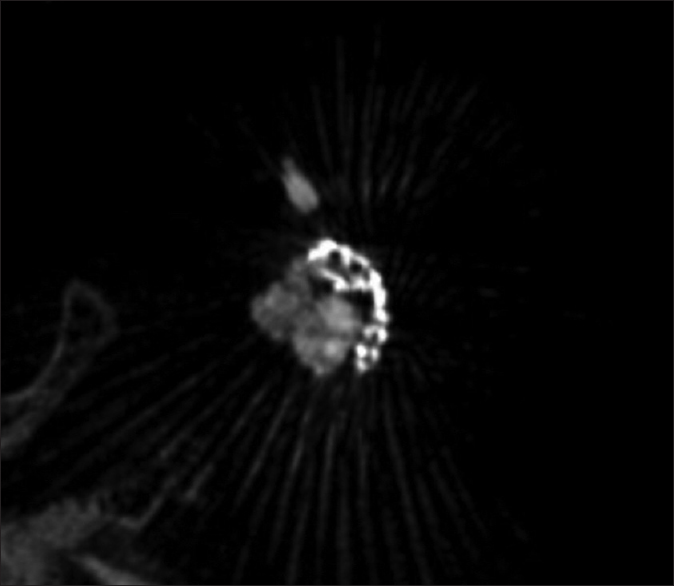
At this point, we felt two-dimensional (2D) angiography was not adequate in diagnosis, and therefore, a volume of interest Dyna CT with 3D reconstructions were obtained. 3D reconstructions demonstrated persistent stenosis within the mid portion of the stent and reticent calcified plaque [
Postoperatively, the patient was extubated in the intensive care unit and was found to be at his neurologic baseline. After being monitored in the intensive care unit for 1 day he was transferred to the general care floor and discharged on post-surgery day 2.
DISCUSSION
Unusual carotid foreign bodies have been described in multiple case reports ranging from firearm fragments and fish bones secondary to penetrating injuries to iatrogenic migration of wires, catheters, and balloons used during endovascular procedures.[
DCPD were designed to prevent distal migration of embolic plaques which most commonly occur during endoluminal manipulations of the carotid artery during CAS. Although rare, DCPD detainment can occur with incomplete stent deployment or stent fracture which may preclude the ability to retrieve the DCPD. The natural history of retained DCPD is unknown because of its porosity and ability to maintain distal cerebral blood flow which sets DCPD apart from other types of foreign bodies. Reports of successful treatment of retained DCPD with medical and surgical therapy have been reported in case reports, therefore, the optimal management of retained DCPD remains a challenge to the endovascular surgeon.[
Expectant management with dual antiplatelet and early anticoagulant therapy with wire removal at the femoral arteriotomy site is a reasonable consideration; however, risk of infection, arterial erosion, thromboembolic events, and further migration are reasons for surgical removal. Standard endovascular techniques are certainly viable options for foreign body removal. Strategies for device retrieval include manipulations to advance or retract the DCPD away from the anchor site and use of snares, forceps, or baskets to provide additional leverage, however, these maneuvers are often unsuccessful due to the size and expandable nature of the DCPD. The DCPD is often anchored along the wall of the internal carotid artery by the carotid stent or imbedded within its tines due to inadequate deployment; therefore, attempts to recapture the device through forceful manipulation is usually ineffective and often dangerous. Immobilization of foreign bodies against the arterial wall with a stent may be a reasonable alternative.[
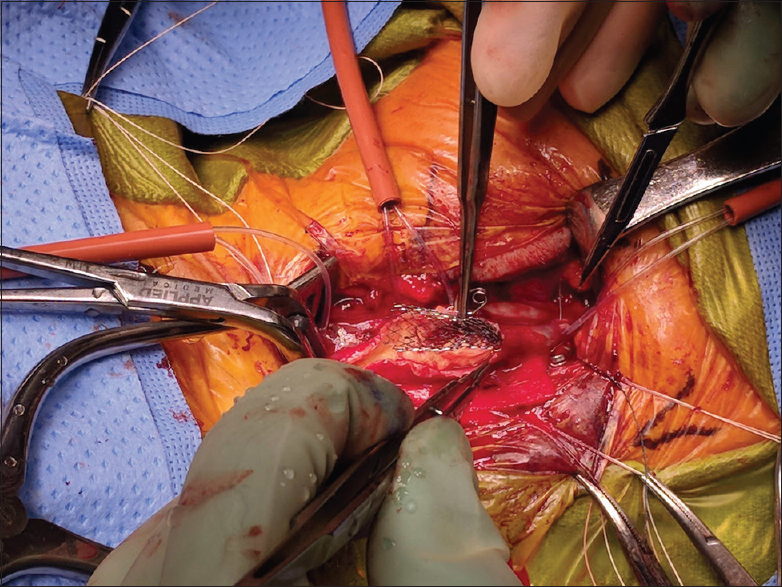
Endarterectomy for device retrieval is a familiar procedure to the neurological or vascular surgeon and can be performed safely in an emergent setting. Although most patients are on dual antiplatelet and anticoagulant therapy, intraoperative bleeding does not appear to be a major barrier to successful surgery, and therefore, reversal agents may not be required to prevent further propagation of any intraluminal thrombus. Open surgical repair requires adequate exposure of the common, external, and internal carotid arteries. The entire length of the endarterectomy may need to be performed using a number 11 blade as scissors are often unable to cut across the stent. Once the stent and DCPD are exposed, the proximal pusher wire may be cut and the stent with the device delivered en bloc. Repair of the endarterectomy may then proceed in the standard fashion using nonabsorbable sutures, and a drain should be left in place in case of persistent oozing within the surgical bed.[
Patient selection for CAS and avoidance of tortuous anatomy, heavily calcified plaques, and critically stenotic lesions may reduce the incidence of retained intraluminal devices. In all reported cases of retained DCPDs, the common variables include severity of stenosis and density of plaque; however, despite optimal patient selection and presurgical planning, complications may occur. Having a low threshold for obtaining 3D angiographic images is paramount in identifying and managing these complications. An in-depth knowledge of the delivery devices, rescue techniques, and salvage procedures are critical in preventing complications during CAS. Although medical therapy may be successful in certain scenarios, device retrieval is ideal if it can be performed safely. If endovascular techniques are unsuccessful in removing the DCPD, surgery is a viable option and can be performed safely despite antiplatelet and anticoagulant therapy.
CONCLUSION
No treatment guidelines exist for retained foreign bodies in the cerebral vasculature; however, the natural history for free floating devices is likely poor with high rates of embolic events. Knowledge of how to retrieve foreign bodies and the salvage techniques are essential to prevent complications from CAS.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cremonesi A, Manetti R, Setacci F, Setacci C, Castriota F. Protected carotid stenting: Clinical advantages and complications of embolic protection devices in 442 consecutive patients. Stroke. 2003. 34: 1936-41
2. Daugherty WP, White JB, Cloft HJ, Kallmes DF. Rescue retrieval of AngioGuard embolic capture system after failure of capture sheath retrieval in carotid angioplasty and stenting. AJNR Am J Neuroradiol. 2008. 29: 1594-5
3. Li T, Zha Y, Bo L, Wirthlin DJ, Zhang Q. Surgical management for retained distal embolic protection device and fractured guidewire after carotid artery stenting. J Surg Case Rep 2016. 2016. p.
4. Padar SC. Air gun pellet embolizing the intracranial internal carotid artery. J Neurosurg. 1975. 43: 222-4
5. Schutz A, Solymosi L, Vince GH, Bendszus M. Proximal stent fixation of fractured coils: technical note. Neuroradiology. 2005. 47: 874-8
6. Shilling K, Uretsky BF, Hunter GC. Entrapment of a cerebral embolic protection device--a case report. Vasc Endovascular Surg. 2006. 40: 229-33
7. Tang IP, Singh S, Shoba N, Rahmat O, Shivalingam S, Gopala KG. Migrating foreign body into the common carotid artery and internal jugular vein—a rare case. Auris Nasus Larynx. 2009. 36: 380-2