- Professor of Clinical Neurosurgery, School of Medicine, State University of New York at Stony Brook, New York, and Chief of Neurosurgical Spine and Education, NYU Winthrop Hospital, NYU Winthrop NeuroScience/Neurosurgery, Mineola, New York 11501, United States.
DOI:10.25259/SNI_394_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. Review of Treatment Options for Smaller Benign Cranial Meningiomas: Observation, Stereotactic Radiosurgery, and Rarely, Open Surgery. 23-Aug-2019;10:167
How to cite this URL: Nancy E. Epstein. Review of Treatment Options for Smaller Benign Cranial Meningiomas: Observation, Stereotactic Radiosurgery, and Rarely, Open Surgery. 23-Aug-2019;10:167. Available from: http://surgicalneurologyint.com/surgicalint-articles/9590/
Abstract
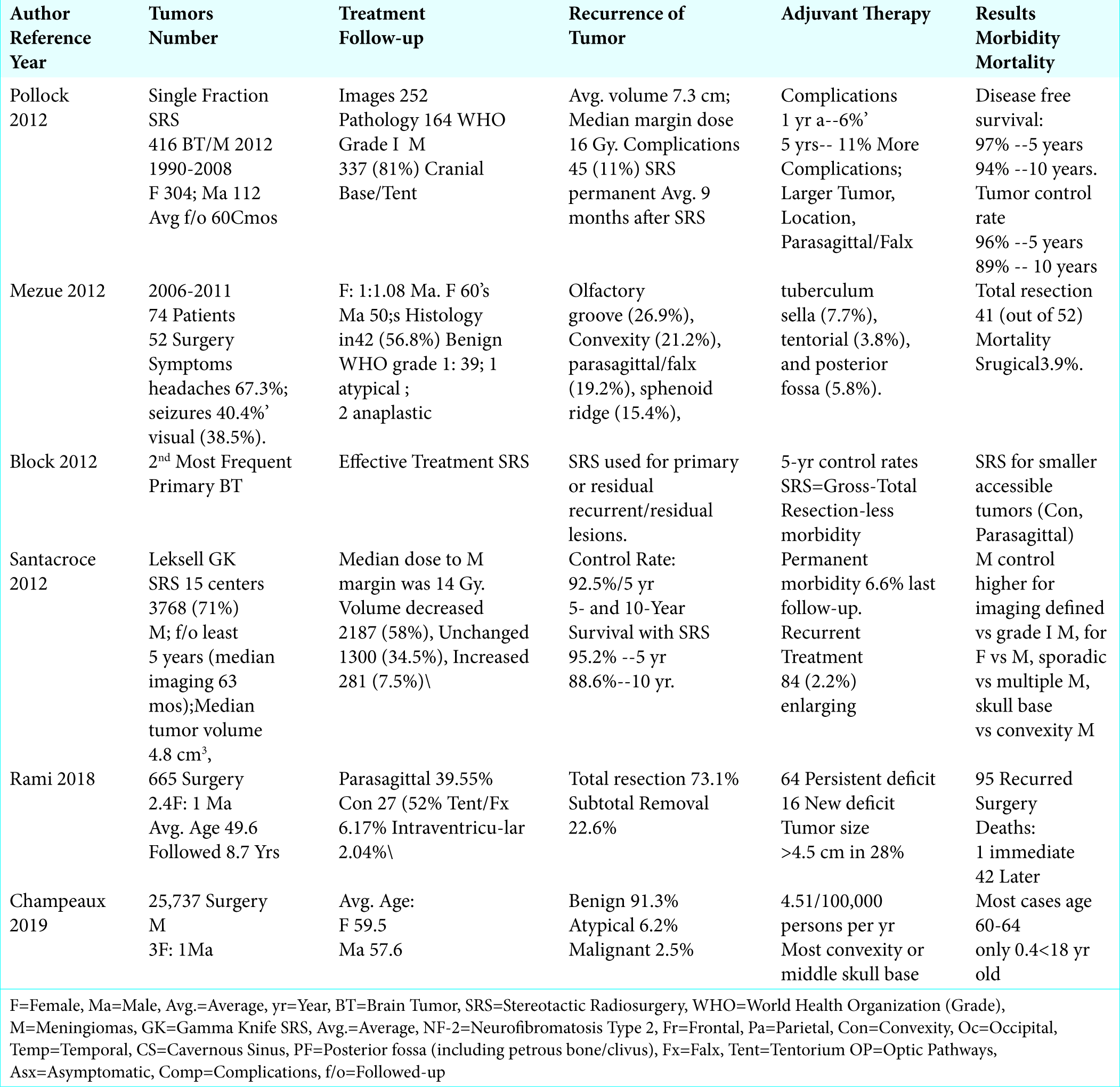
Background: MR/CT documented smaller cranial meningiomas in asymptomatic patients are often followed for years without requiring any intervention. Only a subset of patients who become symptomatic attributed to significant tumor growth, edema and/or mass effect may require stereotactic radiosurgery (SRS), and rarely, open surgery. Clearly, the decision for choosing any treatment modality must be made on a case by case basis and include an analysis of risks vs. benefits to the individual patient.
Methods: Patients with smaller benign asymptomatic meningiomas are followed with sequential MR studies that typically document lack of tumor progression, edema, or mass effect. Those who become symptomatic with the typical triad (i.e. headaches, seizures, or visual loss) and other focal neurological deficits may warrant SRS, and only occasionally, open surgery. Surgery may indeed be warranted in the presence of certain mitigating factors, (e.g. young age, lesions located adjacent to by not yet invading critical structures etc.).
Results: This review focused largely on smaller benign asymptomatic meningiomas. The non-operative/ conservative management vs. use of SRS vs. open surgery in select cases are discussed, along with a review of the morbidity/mortality of the respective interventions.
Conclusion: There are multiple treatment options for patients with smaller asymptomatic cranial meningiomas. SRS may be warranted for those who exhibit tumor growth, increasing edema, and/or mass effect. Only rarely is open operative intervention necessary; this must include consideration of other factors that may warrant early surgery. Notably, the 5-year survival rates for SRS ranged from 95.2% - 97%, while the 10-year survival rates varied from 88.6% - 94%.
Keywords: Cranial Meningiomas, Conservative Observation, Stereotactic Radiosurgery, Open Surgery, Symptoms, Headaches, Seizures, Visual Changes
INTRODUCTION
Benign cranial meningiomas are often followed for years in asymptomatic patients. Only a subset of patient who become symptomatic from documented tumor growth, onset of significant progressive edema, and/or mass effect, or with other unique clinical features placing patients at increased risk (e.g. young age, critical tumor location - near optic chiasm/skull base, other) may warrant stereotactic radiosurgery (SRS), or rarely, open surgery [
Symptoms of Cranial Meningiomas and Karnofsky Scales Before and After Surgery for Recurrent Lesions
In Mezue’s (2012) series of 74 patients with meningiomas, symptoms included; headaches (67.3%), seizures (40.4%), and visual impairment (38.5%), along with increased motor/sensory deficits [
Demographics of Cranial Meningiomas
More females than males develop cranial meningiomas, with ratios varying from 1.08:1 to 2.4:1 to 3:1 [
Location for Meningiomas
Location of Cranial Meningiomas in General
Cranial meningiomas occur in multiple locations [
Cyberknife SRS on 199 lesions; cavernous sinus (99); posterior fossa (28), petrous bone/clivus/anterior optic pathways (29), convexity (22), and falx/tentorium (21) [
Frequency and Locations of Convexity Meningiomas
In two respective series (2012 and 2018), 21.2%-27.5% of 739 meningiomas were convexity lesions [
Average Initial and Recurrent Meningioma Size
The average initial size of unoperated cranial meningiomas in Rami et al. (2018) series was > 4.5 cm in 28.07% of 665 cranial meningiomas [
Conservative Follow-Up of Asymptomatic Benign Meningiomas
Many benign cranial meningiomas may be followed conservatively without the necessity for SRS or open surgery. In 1995, Olivero et al. evaluated the growth rate for asymptomatic cranial meningiomas in 57 patients; notably, 25 of 57 tumors were convexity lesions [
Stereotactic Radiosurgery (SRS) for Benign Meningiomas
The Cyberknife or Gamma Knife (Leksell) SRS systems have gained increased favor over open surgery for the treatment of smaller primary, residual, and/or recurrent benign meningiomas. SRS is typically utilized when tumors are; located in eloquent areas, show little primary tumor growth, demonstrate mild/moderate non-progressive peritumoral edema, and/or where patients are neurologically stable or show only mild progression of neurological symptoms/signs. In 2009, Colombo et al. used Cyberknife SRS (CyberKnife; Accuray, Inc., Sunnyvale, CA) to treat 199 benign cranial meningiomas over an average period of 30 mos. [
Patients Undergoing SRS With/Without Prior Surgery
Three series utilized SRS to treat a total of 615 benign cranial meningiomas; 424 never had any surgery, while 191 had prior surgery [
Average Volumes of Cranial Meningiomas Treated with SRS
In four series, a total of 4508 cranial meningiomas ranging in size from 0.1 to 7.6 cm3 were treated with SRS [
SRS Radiation Doses
In several studies, SRS was typically administered for cranial meningiomas in single radiation doses averaging 14.0--18.5 Gy (range of from 12-25 Gy) [
Residual Volumes and 5 and 10-Year Survival Rates of Meningiomas After SRS
Several studies documented that SRS effectively treated primary, residual (e.g. postoperative), or recurrent cranial meningiomas; the vast majority demonstrated control or decrease in tumor size along with favorable 3, 5, and 10-year outcomes [
SRS Complications/Morbidity
The complication/morbidity rates of SRS for treating benign cranial meningiomas varied from 6.6% to 11% [
Open Surgery for Meningiomas
Demographics for Surgically Managed Meningiomas
For Morokoff et al. (published 2008; series1986-2005) series of 163 patients undergoing open surgery for cranial meningiomas, including 22% convexity lesions, and followed an average of 2.3 years (range 1-13 years), patients averaged 57 years of age (range 20-89 years old), and the female to male ratio was 2.7:1 [
Majority of Cranial Meningiomas Pathologically Documented as Benign (88.3%-91.3%)
The vast majority of cranial meningiomas are pathologically confirmed to be benign [
Extent of Surgical Resection
The extent of primary surgical resection of benign cranial meningiomas varies [
Meningioma Recurrence Following Open Surgery
There was an overall 14.2% incidence of recurrent cranial meningiomas following index open surgery for resection of tumors from all pathological groups [
Pathology of Recurrent Meningiomas with History of Prior Surgery
Although most recurrent meningiomas were initially benign Grade I tumors, those originally presenting with atypical and anaplastic changes were the most likely to recur [
Morbidity for Surgically Treated Meningiomas
Out of 828 patients from two series, following open resection of cranial meningiomas, new postoperative deficits were incurred in from 1.7-2.4% of patients, residual deficits were seen in 9.6%, and overall complications were noted in 9.4% of patients [
Mortality for Surgically Treated Meningiomas
Mortality rates following open surgical resection of cranial meningiomas ranged from 0-1.7% in the short- term (e.g. 30 days), and up to 6.3% over an average of 8.7 postoperative years [
CONCLUSION
Smaller benign cranial meningiomas in asymptomatic patients are often followed for years without requiring any treatment. However, patients who become symptomatic with MR/CT-documented significant tumor growth, peri-tumoral edema, mass effect, new neurological deficits or with other significant confounding factors (i.e. young age, lesions in/near eloquent locations) may warrant stereotactic radiosurgery (SRS), and only rarely, open surgery. Notably, the 5 year and 10-year survival rates following SRS are excellent; 5-year survivals ranged from 95.2% - 97%, and 10-year survivals from 88.6% - 94%. However, for SRS vs. open surgery, the SRS-related long-term sequelae must be carfully weighed against the short-term risks of direct open tumor resection.
References
1. Alvernia JE, Dang ND, Sindou MP. Convexity meningiomas: study of recurrence factors with special emphasis on the cleavage plane in a series of 100 consecutive patients. J Neurosurg. 2011. 115: 491-8
2. Bloch O, Kaur G, Jian BJ, Parsa AT, Barani IJ. Stereotactic radiosurgery for benign meningiomas. J Neurooncol. 2012. 107: 13-20
3. Champeaux C, Weller J, Katsahian S. Epidemiology of meningiomas. A nationwide study of surgically treated tumors on French medico-administrative data. Cancer Epidemiol. 2019. 58: 63-70
4. Colombo F, Casentini L, Cavedon C, Scalchi P, Cora S, Francescon P. Cyberknife radiosurgery for benign meningiomas: short-term results in 199 patients. Neurosurgery. 2009. 64: A7-13
5. Kondziolka D, Madhok R, Lunsford LD, Mathieu D, Martin JJ, Niranjan A. J Stereotactic radiosurgery for convexity meningiomas. Neurosurg. 2009. 111: 458-63
6. Mezue WC, Ohaegbulam SC, Ndubuisi CA, Chikani MC, Achebe DS. Management of Intracranial Meningiomas in Enugu, Nigeria. Surg Neurol Int. 2012. 3: 110-
7. Morokoff AP, Zauberman J, Black PM. Surgery for convexity meningiomas. Neurosurgery. 2008. 63: 427-33
8. Olivero WC, Lister JR, Elwood W. The natural history and growth rate of asymptomatic meningiomas: a review of 60 patients. J Neurosurg. 1995. 83: 222-4
9. Pollock BE, Stafford SL, Link MJ, Brown PD, Garces YI, Foote RL. Single-fraction radiosurgery of benign intracranial meningiomas. Neurosurgery. 2012. 71: 604-12
10. Rami A, Suzan E, Rafeed A, Nooruddeen AM, Lamees A, Duaa A. The Sovereignty of Primary Cranial Tumors-Meningiomas: Vetting the Cardinal Epidemiological Features. Med Arch. 2018. 72: 434-438
11. Santacroce A, Walier M, Régis J, Liščák R, Motti E, Lindquist C. Long-term tumor control of benign intracranial meningiomas after radiosurgery in a series of 4565 patients. Neurosurgery. 2012. 70: 32-9