- Chief of Neurosurgical Spine and Education, Winthrop University Hospital, Mineola, New York - 11501, USA
Correspondence Address:
Nancy E. Epstein
Chief of Neurosurgical Spine and Education, Winthrop University Hospital, Mineola, New York - 11501, USA
DOI:10.4103/2152-7806.196764
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. Should anyone perform percutaneous endoscopic laser diskectomy and percutaneous lumbar disc decompressions?. 26-Dec-2016;7:
How to cite this URL: Nancy E. Epstein. Should anyone perform percutaneous endoscopic laser diskectomy and percutaneous lumbar disc decompressions?. 26-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/should-anyone-perform-percutaneous-endoscopic-laser-diskectomy-and-percutaneous-lumbar-disc-decompressions/
Abstract
Background:Increasingly, pain management specialists (P-S) (e.g., anesthesiologists, radiologists, or physiatrists), who are not spinal surgeons, are performing percutaneous endoscopic laser diskectomy (PELD), percutaneous lumbar disc decompression (PLDD), and target percutaneous laser disc decompression (T-PLDD) in patients with minimal/mild disc herniations. Here, theoretically, the laser vaporizes/shrinks a small portion of disc tissue that lowers intradiscal pressure/volume, and thereby provides “symptomatic relief” (e.g., low back pain/radiculopathy). Nevertheless, the vast majority of these patients experience spontaneous relief of their complaints over several months without any intervention.
Methods:A literature review revealed that P-S specialists are performing PELD/PLDD/T-PLDD to address minimal/mild disc herniations. However, multiple well-designed studies confirmed that PELD/PLDD/T-PLDD were ineffective for managing acute/chronic pain in these patients.
Results:Several randomized clinical trials documented the lack of clinical efficacy of PELD/PLDD/T-PLLD procedures over microdiskectomy. PELD/PLDD/T-PLDD correlated with only 60–70% success rates with higher reoperation rates (e.g., up to 38%) vs. 90% success rates for routine microdiskectomy (e.g., with faster recovery and only 16% reoperation rates). Nevertheless, without surgical training, P-S are performing these procedures and are, therefore, unable to adddress perioperative/postoperative PELD/PLDD/T-PLDD surgical complications.
Conclusions:Pain management specialists, who are not trained spinal surgeons, should not perform PELD/PLDD/T-PLDD surgery to treat minimal/mild disc herniations. Not only do most of these discs resolve spontaneously over several months but also they are largely ineffective. Furthermore, there is no evidence to support the superiority of PELD/PLDD/T-PLDD procedures over microdiskectomy even if performed by spinal specialists.
Keywords: Pain management specialists: Not surgeons, percutaneous lumbar endoscopic diskectomy, spinal surgery
INTRODUCTION
Should pain management specialists (P-S) (e.g., anesthesiologists, radiologists, and physiatrists), who are not spinal surgeons, perform percutaneous endoscopic laser discectomy (PELD), percutaneous lumbar disc decompression (PLDD), and target percutaneous laser disc decompression (T-PLDD) for minimal/mild disc herniations? Here, in theory, the laser vaporizes/shrinks a small portion of disc tissue that lowers the intradiscal pressure/volume, and provides “symptomatic relief” of low back pain/radiculopathy. However, the natural history for these minimal/mild disc hernations is that the vast majority spontaneously resolve over several months without any intervention. Furthermore, when “surgery” is indicated, several well-designed studies have shown that PELD/PLDD/T-PLDD are ineffective in the management of acute/chronic pain in patients with minimal/mild lumbar disc herniations and have lower success rates (60–70%) and higher reoperation rates (38%) vs. routine microdiskectomy [e.g., 90% success rates/faster recovery rates and fewer reoperations (16% rates)].
Natural history of lumbar disc herniations: The majority spontaneously improve
Many patients with unilateral radiculopathy due to minimal/mild disc bulges experience spontaneous clinical/radiographic [magnetic resonance (MR)-documented] improvement of their discopathy/radiculopathy without PELD/PLDD/T-PLDD.[
Pain management specialists perform percutaneous injections, including epidural spinal injections, but are not spinal surgeons
In a commentary in 2013, Epstein noted that P-S perform multiple unnecessary epidural spinal injections (ESI) that are “typically short-acting and ineffective over the longer-term.”[
“Pros” for PELD/PLDD/T-PLDD based on studies without clinical control groups or independent observers
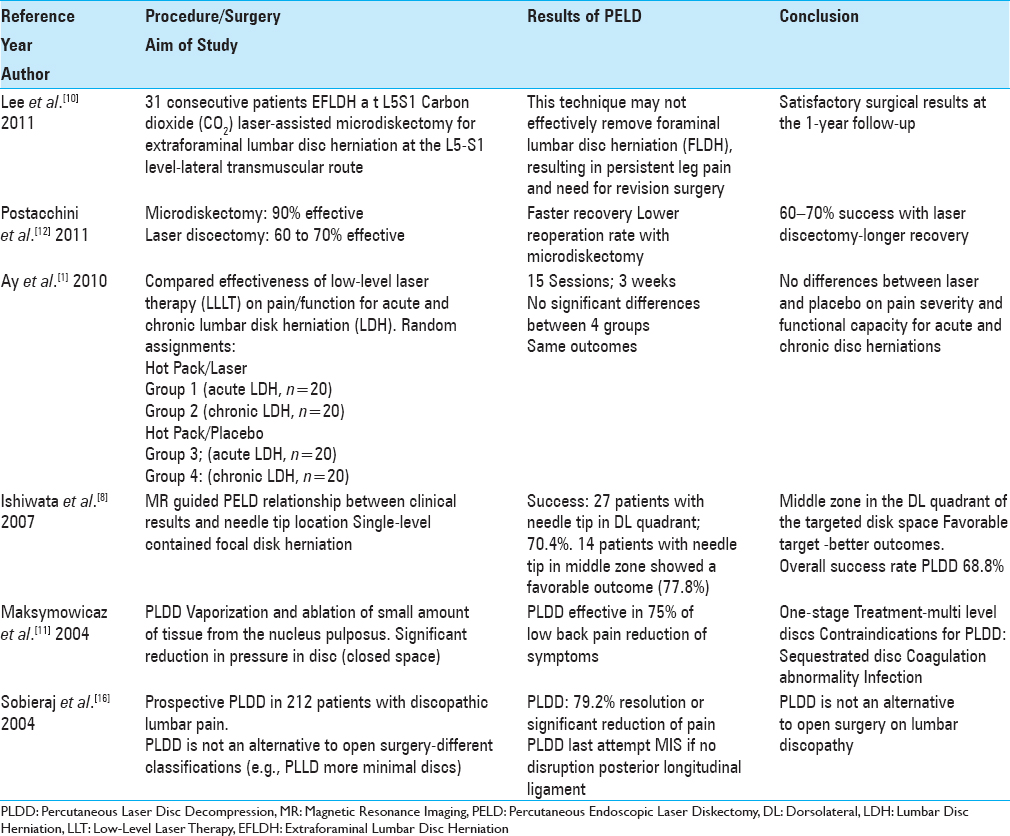
Several poorly designed studies without clinical control groups or independent observers, documented the safety/efficacy/outcomes of PELD/PLDD/T-PLDD [Tables
Treatment with PLDD fails to demonstrate loss of disc height on radiographic studies
Ren et al. evaluated the medium-term results of neuroradiological imaging following 22 PLDD, looking for confirmation of loss of disc height [
“Cons,” including lack of efficacy, of PELD/PLDD/T-PLDD substantiated in multiple well-designed prospective randomized trials
Multiple prospective randomized trials documented the lack of efficacy of PELD/PLDD/T-PLDD alone or compared with microdiskectomy.[
PELD/PLDD ineffective in managing acute/chronic pain in a clinical randomized double blind placebo-controlled trial versus experimental dog model
In a randomized, double blind, placebo-controlled trial, Ay et al. determined that low-level laser therapy (LLT) proved of no benefit (was ineffective) for patients with acute/chronic pain attributed to lumbar disc herniations (LDH) [
SUMMARY
Pain management specialists, who are not spinal surgeons, are increasingly performing PELD/PLDD/T-PLDD operations for minimal/minor lumbar disc herniations, which many contend, would resolve spontaneously over several months duration. Furthermore, the “pros” for these procedures comes from typically poorly designed clinical studies, without controls or independent evaluators.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ay S, Doğan SK, Evcik D. Is low-level laser therapy effective in acute or chronic low back pain?. Clin Rheumatol. 2010. 29: 905-10
2. Brouwer PA, Brand R, van den Akker-van Marle ME, Jacobs WC, Schenk B, van den Berg-Huijsmans AA. Percutaneous laser disc decompression (PLDD) versus conventional microdiscectomy in sciatica: A randomized controlled trial. Spine J. 2015. 15: 857-65
3. Casey E. Natural history of radiculopathy. Phys Med Rehabil Clin N Am. 2011. 22: 1-5
4. Deen HG. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002. 27: 2081-2
5. Draper WE, Schubert TA, Clemmons RM, Miles SA. Low-level laser therapy reduces time to ambulation in dogs after hemilaminectomy: A preliminary study. J Small Anim Pract. 2012. 53: 465-9
6. Epstein NE. The risks of epidural and transforaminal steroid injections in the Spine: Commentary and a comprehensive review of the literature. Surg Neurol Int. 2013. 22: S74-93
7. Goupille P, Mulleman D, Mammou S, Griffoul I, Valat JP. Percutaneous laser disc decompression for the treatment of lumbar disc herniation: A review. Semin Arthritis Rheum. 2007. 37: 20-30
8. Ishiwata Y, Takada H, Gondo G, Osano S, Hashimoto T, Yamamoto I. Magnetic resonance-guided percutaneous laser disk decompression for lumbar disk herniation--Relationship between clinical results and location of needle tip. Surg Neurol. 2007. 68: 159-63
9. Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K. The natural history of herniated nucleus pulposus with radiculopathy. Spine. 1996. 21: 225-9
10. Lee DY, Lee SH. Carbon dioxide (CO 2) laser-assisted microdiscectomy for extraforaminal lumbar disc herniation at the L5-S1 level. Photomed Laser Surg. 2011. 29: 531-5
11. Maksymowicz W, Barczewska M, Sobieraj A. Percutaneous laser lumbar disc decompression-Mechanism of action, indications and contraindications. Ortop Traumatol Rehabil. 2004. 6: 314-8
12. Postacchini F, Postacchini R. Operative management of lumbar disc herniation: The evolution of knowledge and surgical techniques in the last century. Acta Neurochir Suppl. 2011. 108: 17-21
13. Ren L, Guo H, Zhang T, Han Z, Zhang L, Zeng Y. Efficacy evaluation of percutaneous laser disc decompression in the treatment of lumbar disc herniation. Photomed Laser Surg. 2013. 31: 174-8
14. Ren L, Guo B, Zhang T, Bai Q, Wang XH, Zhang L. Medium-term follow-up findings in imaging manifestation after percutaneous laser disc decompression. Photomed Laser Surg. 2013. 31: 247-51
15. Singh V, Manchikanti L, Calodney AK, Staats PS, Falco FJ, Caraway DL. Percutaneous lumbar laser disc decompression: An update of current evidence. Pain Physician. 2013. 16: SE229-60
16. Sobieraj A, Maksymowicz W, Barczewska M, Konopielko M, Mazur D. Early results of percutaneous laser disc decompression (PLDD) as a treatment of discopathic lumbar pain. Orthop Traumatol Rehabil. 2004. 6: 264-9
17. Zhao XL, Fu ZJ, Xu YG, Zhao XJ, Song WG, Zheng H. Treatment of lumbar intervertebral disc herniation using C-arm fluoroscopy guided target percutaneous laser disc decompression. Photomed Laser Surg. 2012. 30: 92-5