- Department of Orthopaedic Surgery, University of Toyama, Toyama, Japan
- Department of Neurosurgery, University of Toyama, Toyama, Japan
- Department of Diagnostic Pathology, University of Toyama, Toyama, Japan
Correspondence Address:
Yoshiharu Kawaguchi
Department of Neurosurgery, University of Toyama, Toyama, Japan
DOI:10.4103/sni.sni_221_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Miho Zaimoku, Yoshiharu Kawaguchi, Shoji Seki, Yasuhito Yahara, Naoki Akioka, Johji Imura, Tomoatsu Kimura, Satoshi Kuroda. Sporadic hemangioblastoma of the film terminale with peritumoral cyst. 10-Jan-2018;9:2
How to cite this URL: Miho Zaimoku, Yoshiharu Kawaguchi, Shoji Seki, Yasuhito Yahara, Naoki Akioka, Johji Imura, Tomoatsu Kimura, Satoshi Kuroda. Sporadic hemangioblastoma of the film terminale with peritumoral cyst. 10-Jan-2018;9:2. Available from: http://surgicalneurologyint.com/surgicalint-articles/sporadic-hemangioblastoma-of-the-film-terminale-with-peritumoral-cyst/
Abstract
Background:Spinal hemangioblastoma originating from the film terminale are rare tumors. Here, we present a film terminale hemangioblastoma and review the appropriate literature.
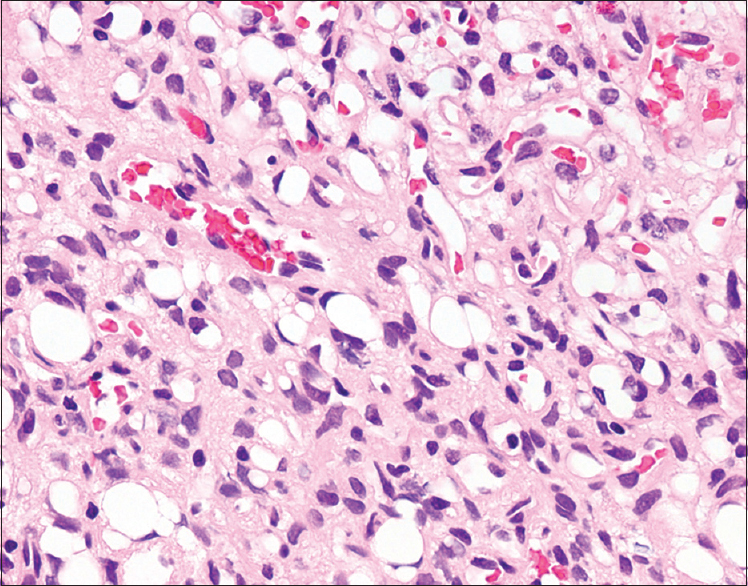
Case Description:A 37-year-old female presented with bilateral lower extremity pain without a focal neurological deficit. The magnetic resonance (MR) image demonstrated an intradural spinal tumor at the L1 level, which was accompanied by peritumoral cysts. In addition, there were multiple surpentine flow voids (e.g., consistent with torturous and convoluted vessels), which is typical for hemangioblastoma. At surgery, a spinal hemangioblastoma originating from the film terminale with peritumoral cysts at the L1 level was fully excised without producing a focal postoperative neurological deficit. Histological examination revealed stromal cells with vacuolated cytoplasm and small nuclei in a rich capillary network accompanied by several enlarged vessels. These finding were compatible with a hemangioblastoma.
Conclusions:We reported a rare case of a hemangioblastoma originating from the conus presenting at the L1 level. Complete surgical resection was accomplished without any motor deficit.
Keywords: Film terminale, hemangioblastoma, indocyanine green videoangiography, peritumoral cyst, surgical resection
INTRODUCTION
Spinal hemangioblastomas are rare tumors that account for approximately 3% of all intramedullary spinal tumors. They are often associated with von Hippel Lindau (vHL) disease. Spinal hemangioblastomas predominantly occur in the cervical and thoracic cord[
CASE REPORT
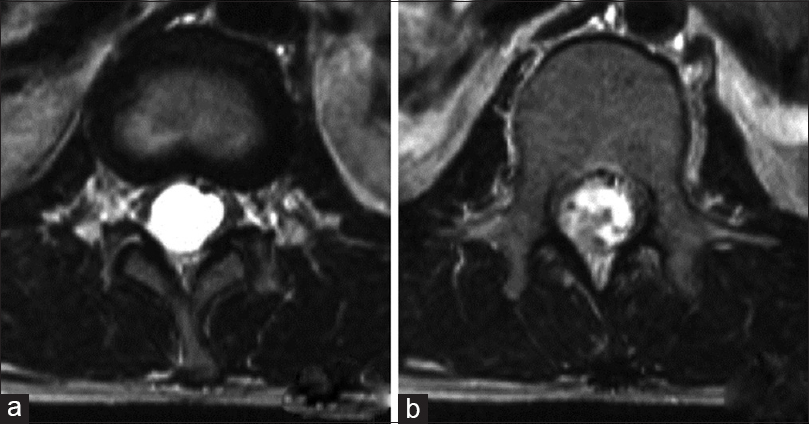
A 37-year-old female presented with bilateral lower extremity night pain for 2 months without any focal neurological deficits, including normal sphincter function. She had no family history of central nervous system (CNS) tumors, and screening for vHL disease was negative. The MR imaging demonstrated an intradural spinal tumor at the level of the conus (L1). The tumor was 8 × 6 mm and isointense on both T1-weighted (T1) and T2-weighted (T2) MR images [
Surgical excision of hemangioblastoma of the conus.
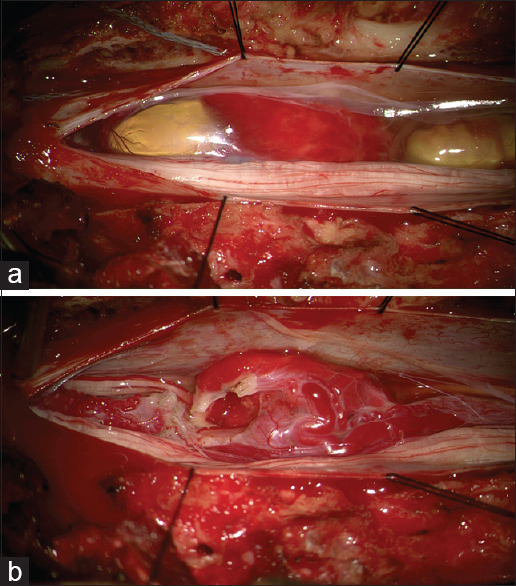
The patient underwent an L1 to L3 laminectomy. Under the operative microscope, the dura and arachnoid were opened, revealing a reddish tumor originating from the conus accompanied by cranial and caudal peritumoral cysts [Figure
Histology
The histological examination of the tumor was consistent with a hemangioblastoma; it revealed stromal cells with vacuolated cytoplasm and small nuclei in a rich capillary network with several enlarged vessels; there were no mitotic elements [
DISCUSSION
There are only 11 case reports of conus hemangiolastomas in the literature.[
Spinal angiography/embolization for hemangioblastomas
Spinal angiography is useful for detecting the location and vascularity of spinal hemangioblastomas tumor. In this case, it documented the hypervascularity of the lesion. It was also helpful in planning the surgical resection. Biondi et al. performed preoperative embolization in 4 cases with hemangioblastoma of the lower spinal region and determined it to be useful.[
Pathology/surgery for hemangioblastomas
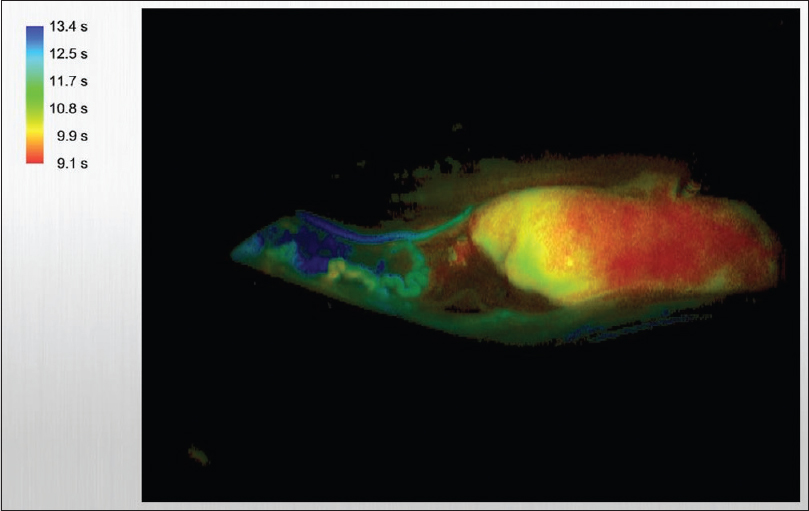
Hemangioblastomas are benign tumors that should undergo partial/complete resection, as dictated by their location. The use of ICG videoangiography effectively identifies the feeding and drainaging vessels, facilitating tumor resection.[
CONCLUSION
We presented a rare hemangioblastoma arising from the film terminale associated with cepahald/caudad peritumoral cysts. The preoperative routine/enhanced MR readily documented surpentine flow voids of torturous/convoluted vessels characteristic for hemangioblastoma. Surgical resection was accomplished without preoperative embolization, and the patient exhibited no permanent neurological deficit.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Biondi A, Ricciardi GK, Faillot T, Capelle L, Van Effenterre R, Chiras J. Hemangioblastomas of the lower spinal region: Report of four cases with preoperative embolization and review of the literature. AJNR Am J Neuroradiol. 2005. 26: 936-45
2. Ciappetta P, Occhiogrosso G, Domenicucci M, D’Andrea G, Bastianello S, Frati A. Hemangioblastoma of the filum terminale. Case report and review of the literature. J Exp Clin Cancer Res. 2007. 26: 281-5
3. da Costa LB Jr, de Andrade A, Braga BP, Ribeiro CA. Cauda equina hemangioblastoma: Case report. Arq Neuropsiquiatr. 2003. 61: 456-8
4. Escott EJ, Kleinschmidt-DeMasters BK, Brega K, Lillehei KO. Proximal nerve root spinal hemangioblastomas: Presentation of three cases, MR appearance, and literature review. Surg Neurol. 2004. 61: 262-73
5. Hao S, Li D, Ma G, Yang J, Wang G. Application of intraoperative indocyanine green videoangiography for resection of spinal cord hemangioblastoma: Advantages and limitations. J Clin Neurosci. 2013. 20: 1269-75
6. Kunihiro N, Takami T, Yamagata T, Tsuyuguchi N, Ohata K. Spinal hemangioblastoma of cauda equina origin not associated with von Hippel-Lindau syndrome-case report. Neurol Med Chir (Tokyo). 2011. 51: 732-5
7. Nadkarni TD, Menon RK, Desai KI, Goel A. Hemangioblastoma of the filum terminale. J Clin Neurosci. 2006. 13: 285-8
8. Saliou G, Giammattei L, Ozanne A, Messerer M. Role of preoperative embolization of intramedullary hemangioblastoma. Neurochirurgie. 2016. p.
9. Sergides IG, Wainwright KL, Biggs M. Incidental hemangioblastoma of the filum terminale. Acta Neurol Belg. 2009. 109: 55-6
10. Siller S, Szelényi A, Herlitz L, Tonn JC, Zausinger S. Spinal cord hemangioblastomas: Significance of intraoperative neurophysiological monitoring for resection and long-term outcome. J Neurosurg Spine. 2017. 26: 483-93